Article In Press : Article / Volume 3, Issue 1
Case Report | DOI: https://doi.org/.
A Bizarre Bronchoscopic Appearance in Cases of Pneumomediastinum Linked to The Coronavirus
- Service de pneumologie de lâhôpital militaire dâinstruction Mohamed V. BP 10045 Rabat. Maroc.
Correspondng Author: Anass Benali
Citation: Anass Benali, Ismail Abderrahmani Rhorfi, Hicham Souhi, Hanane El Ouazzani, Ahmed Abid. (2024). A bizarre bronchoscopic appearance in cases of pneumomediastinum linked to the coronavirus. International Journal of Pulmonology and Disorders. 3(1).
Copyright: © 2024 Anass Benali, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2023-09-12, Received Date: 2023-09-12, Published Date: 2024-03-12
Abstract Keywords: COVID-19; pneumonia; pneumomediastinum; bronchial mucosa; bronchoscopy.
Abstract
The description of lesions of the bronchial mucosa during Covid-19 remains exceptional in the literature review. Our observation concerns a 29-year-old patient with no history presenting an acute clinical situation made up of the combination of subcutaneous emphysema and pneumomediastinum whose etiological exploration confirms the diagnosis of severe acute respiratory syndrome coronavirus 2 (SARS COV-2). The peculiarity of our work is the discovery of a bizarre appearance during the bronchoscopy performed during this clinical presentation which is described as rare in Covid-19.
Introduction
The global, health, economic and social impact of SARS-COV-2 is continuously evaluated. The spontaneous alveolar air leakage is a rare complication of Covid-19 pneumonia.
We describe a particular aspect of the bronchial mucosa never described before during pneumomediastin in a 29 year old man with covid19 pneumonia.
Observation
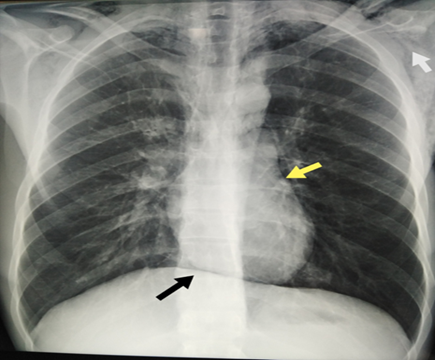
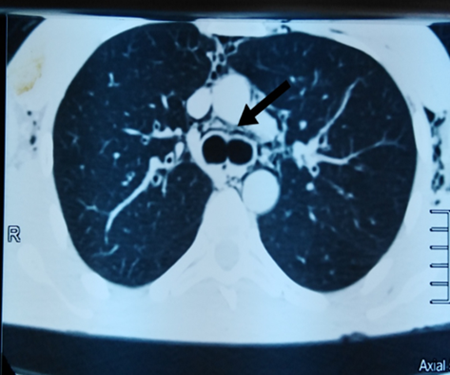
Mr. Y.E, 29 years old, never treated for tuberculosis, without a history of digestive diseases, tobacco and cannabis smoker for 15 years and without notion of recent thoracic trauma, admitted to the pulmonology department for acute dyspnea occurring for one-week, physical examination reveals subcutaneous emphysema in the neck and upper trunk with polypnea at 25 cycles per minute and 93% ambient air saturation. Standard chest x-ray and Chest CT scan without contrast media injection show pneumomediastinum (figure 1, 2). Flexible bronchial endoscopy performed to look for a cause for pneumomediastinum reveals a bizarre aspect never seen before in such a situation, it is in fact a riddled aspect of the bronchial mucosa which presents multiple small ulcers located at the entrance to the right upper lobe bronchus and at the entrance to the intermediate trunk, with purulent secretions (figure 3, 4). The microbiological samples taken at the end of this fibroscopy show: a negative test for Koch's bacillus by GeneXpert MTB / RIF, but they confirm the presence of coronavirus by Polymerase Chain Reaction (PCR). The patient is put on standard covid-19 treatment with antibiotic therapy and oxygen therapy. The course within a week is favorable with the disappearance of subcutaneous emphysema and improvement in general condition and saturation.


Discussion
Pneumomediastinum is part of the air leak syndrome and this term refers to the abnormal existence of extra-alveolar air in the mediastinum, this is a condition found in different circumstances, the pathophysiology of pneumomediastinum depends on the clinical circumstances in which it occurred, most often it is the result of an alveolar rupture, sometimes it can be the result of an air leak from the upper airways, lower airways or digestive tract [1]. Pneumomediastinum can be spontaneous or secondary, in the secondary one, these air leaks are often traumatic or iatrogenic or infectious [2]. Pneumomediastinum is a rare complication of Covid-19 pneumonia and it occurs mainly in men in 60% of cases with an unfavorable outcome in 50% of cases [3]. In a patient infected with the severe acute respiratory syndrome coronavirus 2 ( SARS-CoV-2), the role of bronchoscopy in diagnosis was treated by the American Association of Bronchoscopy and Interventional Pulmonology (AABIP), indeed this role is limited and its indication must be reserved for urgent cases, especially for therapeutic purposes as for symptomatic tracheal or bronchial stenosis, symptomatic airway obstruction, massive hemoptysis etc, but also for diagnostic purposes and we can accept the suspicion of lung cancer or suspected infection in immune-compromised patients. The brochoscopy should follow precautions to reduce the risk of exposure and contamination of personnel [4]. Emergency bronchoscopy has an essential place in the diagnostic strategy in the thoracic trauma responsible for pneumomediastinum and/or bilateral pneumothorax and subcutaneous emphysema. It clearly describes trachea-bronchial lesions; it determines their severity and therefore guides subsequent therapeutic management [5].
Conclusion
the realization of the bronchoscopy during the pneumomediastinum whatever the cause must be encouraged so that it guides us the etiological diagnosis, at the same time to discover new endoscopic aspects in particular in the Covid-19 and thus to be among the diagnostic criteria especially if the PCR is negative.
Thanks
Pneumology department of the military hospital of Rabat who contributed to the realization of this article.
Declaration of Interests
The authors declare that they have no conflicts of interest in relation to this article.
References
- Cheng, G. S., Varghese Jr, T. K., & Park, D. R. (2016). Pneumomediastinum and mediastinitis. In Murray and Nadel's Textbook of Respiratory Medicine (pp. 1496-1510). WB Saunders.
- Caceres, M., Ali, S. Z., Braud, R., Weiman, D., & Garrett Jr, H. E. (2008). Spontaneous pneumomediastinum: a comparative study and review of the literature. The Annals of thoracic surgery, 86(3), 962-966.
- Quincho-Lopez, A., Quincho-Lopez, D. L., & Hurtado-Medina, F. D. (2020). Case report: pneumothorax and pneumomediastinum as uncommon complications of COVID-19 pneumonia—literature review. The American journal of tropical medicine and hygiene, 103(3), 1170.
- Vergnon, J. M., Trosini-Desert, V., Fournier, C., Lachkar, S., Dutau, H., Guibert, N., ... & Froudarakis, M. (2020). Bronchoscopy use in the COVID-19 era. Respiratory medicine and research, 78, 100760.
- Groenendijk, M. R., Hartemink, K. J., Dickhoff, C., Geeraedts Jr, L. M., Terra, M., Thoral, P., & Hashemi, S. M. (2014). Pneumomediastinum and (bilateral) pneumothorax after high energy trauma: Indications for emergency bronchoscopy. Respiratory medicine case reports, 13, 9-11.


