Current Issue : Article / Volume 3, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5127/016
A Comparative Evaluation of Dosal Usefulness in Total Scalp Irradiation according to Treatment Plans and Methods
- Department of Radiation Oncology, Yonsei University Yonsei Cancer Center
Byeol Nim Park
Byeol Nim Park, et.al., (2024). A Comparative Evaluation of Dosal Usefulness in Total Scalp Irradiation according to Treatment Plans and Methods. Radiology Research and Diagnostic Imaging. 3(1); DOI: 10.58489/2836-5127/016
© 2024 Byeol Nim Park, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 12-07-2023
- Accepted Date: 01-02-2024
- Published Date: 12-03-2024
Total scalp irradiation, Helical Tomo Therapy, Complete Block, Volumetric Modulated Arc Therapy
Abstract
Objective: The purpose of this study is to choose a treatment plan and equipment to maximize tangential irradiation to protect the normal brain tissues as much as possible during total scalp irradiation.
Subjects and Methods: After zoning the total scalp of a phantom and selecting a target area for treatment, the study made a Helical Tomo Therapy (HT) plan, a Helical Tomo Therapy with a Complete Block (HTCB) plan, and a Volumetric Modulated Arc Therapy (VMAT) plan. All of these plans made sure that the volume of a treatment plan with 95% of a prescription dose (40 Gy) would not exceed 95% of the entire volume and that Dmax would not be more than 110% of the prescription dose. The plans compared doses among organs at risk of damage including the brain. Doses in the brain tissues were assessed based on the volumetric criteria for normal tissues in Emami et al.
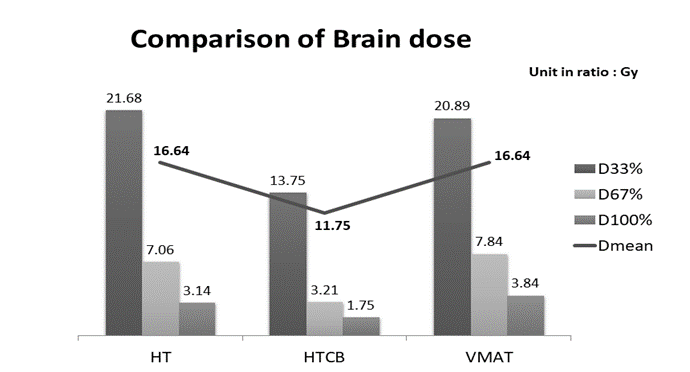
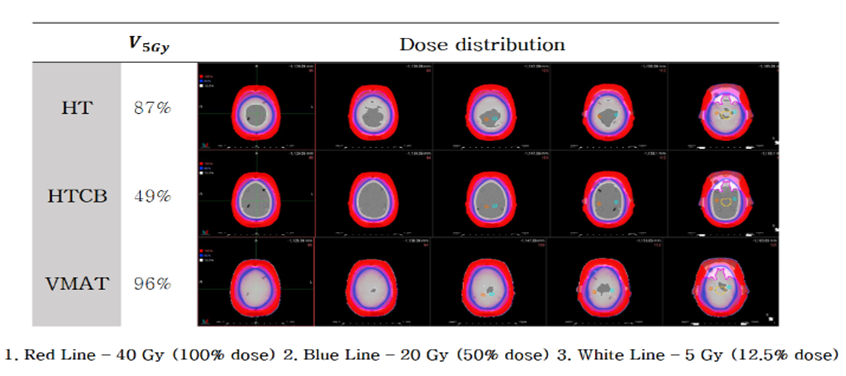
Results: HT, HTCB, and VMAT had a dose of 21.68 Gy, 13.75 Gy, and 20.89 Gy, respectively, in brain tissues at D33%, a dose of 7.06 Gy, 3.21 Gy, and 7.84 Gy, respectively, at D67%, and a dose of 3.14 Gy, 1.75 Gy, and 3.84 Gy, respectively, at D100%. They recorded a Dmean of 16.64 Gy, 11.78 Gy, and 16.64 Gy, respectively. These results show that the overall dose was low in the HTCB plan. When the volume of a low dose was calculated based on 5 Gy, they recorded 87%, 49%, and 96%, respectively, in V5Gy. In addition, the maximum dose in the remaining organ (brain stem, hippocampus, and both lenses) except for the optic pathway was the lowest in HTCB
Conclusion: The findings demonstrate that Tomo Therapy with a complete block minimized a dose in organs at risk of damage including the brain and hippocampus on both sides and accordingly reduced the probability of side effects such as radiation-induced brain injuries and a resulting decrease in neurocognitive functions. In addition to total scalp irradiation, if additional studies on ring targets treated in various areas are conducted to establish the benefits of tangential irradiation, it is believed that Tomo Therapy using Complete Block can be used to maximize tangential irradiation in treatment planning.
Objective
Angiosarcoma is a rare malignant tumor of the connective tissue that originates from endothelial cells. It often occurs in the head and neck region and is challenging to treat due to its local spread and simultaneous multifocal nature, making radical surgery almost impossible. Therefore, radiation therapy is performed to prevent local recurrence, including various types of cancers such as malignant melanoma, lymphoma, and fibrosarcoma, among others. However, total scalp irradiation poses challenges as the scalp has a wide, irregular range
and encompasses the normal brain tissue, leading to unclear radiation doses to numerous neuroanatomical structures and causing neurological impairments in cognitive development, hypothalamic-pituitary function, and brain function [1, 2]
Radiation-induced brain injury (RIBI), including temporal lobe necrosis and neurocognitive function (NCF) decline, is associated with late neurotoxicity resulting from radiation therapy [3, 4, 5, 6]. Therefore, various studies have been conducted aiming to reduce radiation doses to the brain tissue and minimize risks to several vulnerable organs within the brain during total scalp treatment [7, 8, 9, 10, 11, 12].
Initially, three-dimensional conformal radiation therapy (3D-CRT) combined with electron beams and X-rays was commonly used. However, limitations such as decreased dose homogeneity in curved areas due to the diversity of source-skin distance (SSD) and the occurrence of high-dose and low-dose regions at the junction where the radiation field coincides with the treatment plane led to the introduction of intensity-modulated radiation therapy (IMRT) as an alternative [7, 10, 12].
IMRT requires geometric characteristics that utilize tangential fields by manipulating the multi-leaf collimator (MLC) due to the morphological features of the target. Reports have indicated that treatment planning techniques and equipment selection can affect the dosimetric outcomes [8, 10, 12].
Therefore, in this study, we compared and evaluated different treatment modalities to maximize tangential fields for optimal protection of normal brain tissue. We analyzed and compared helical Tomo Therapy (HT) planning, helical Tomo Therapy with a complete block (HTCB) using a complete block, and volumetric modulated arc therapy (VMAT) planning.
Subjects and Methods
Computed Tomography (CT) Imaging and Target Delineation
An ATOM phantom (Sun Nuclear Corporation, AU) was used, and a hard bolus (EZ bolus, Klarity Medical Products, USA) was applied. CT images for simulation were acquired using an Aquilion Exceed LB CT scanner (Canon Medical System, USA) with a slice thickness of 3mm. For structures such as bilateral eyeballs, optic nerves, lenses, brainstem, and hippocampus that were not present in the phantom, three-dimensional volumes based on their actual anatomical structures were referenced.
The target volume was delineated as the clinical target volume (CTV), representing the total scalp. A 5mm margin was added to create the planning target volume (PTV), and a prescription dose of 40 Gy (2 Gy per fraction) was set. All treatment plans were calculated to ensure that 95% of the prescribed dose (38 Gy) covered at least 95% of the PTV, and the maximum dose (Dmax) did not exceed 110% of the prescribed dose. The MIM Maestro Software System (Version 7.17) was used to normalize the dose so that 40 Gy encompassed 95% of the PTV for comparison and analysis.
Helical Tomo Therapy (HT) Planning
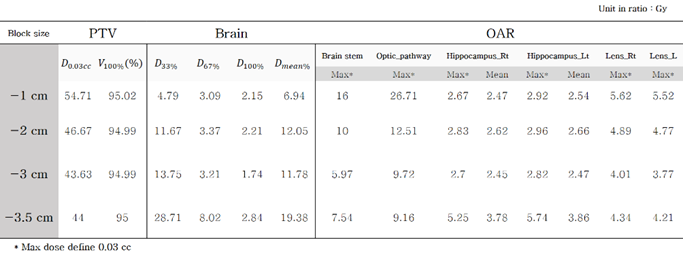
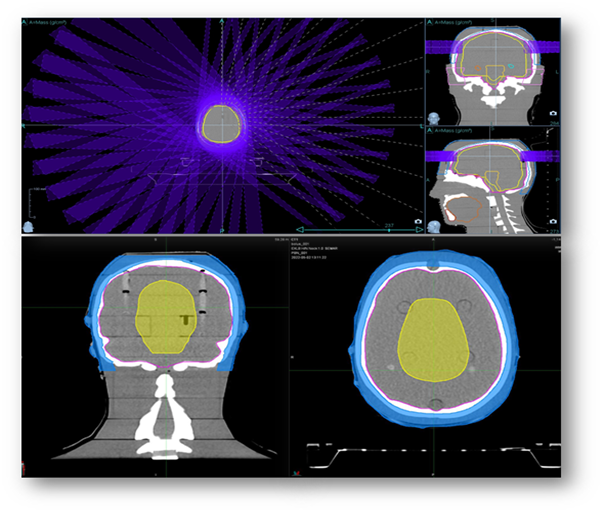
The Precision treatment planning system (Version 2.0.1.1, Accuray, USA) was used for Tomo Therapy planning. Two different planning methods were employed: the standard helical Tomo Therapy (HT) planning, which optimizes the dose by setting conditions for the volume of the brain, and the HT with a complete block, which optimizes the dose by restricting the entry and exit speeds within the specified volume. The modulation factor and pitch were set to converge to recommended values of 20 seconds for the gantry period, and the field width was set to 2.5 cm. For the complete block method, the brain volume was reduced by 1 cm, 2 cm, 3 cm, and 3.5 cm in different plans to meet the dose conditions for the planning volume while providing the best protection for normal brain tissue. The reduction in the left-right direction was defined as 3 cm, and in the superior-inferior direction, it was 1 cm. The energy used was 6 MV with flattening filter-free (FFF). (Fig. 1, Table 1)
Table 1. Comparison of treatment plans by complete block size
Volumetric Modulated Arc Therapy (VMAT) Planning
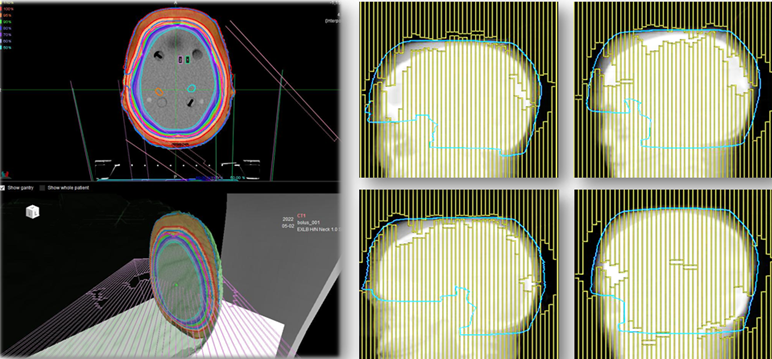
The Ray Station treatment planning system (Version 5.0.2.35, Ray Station Laboratories, Sweden) was used for VMAT planning. Three arcs were used, with a couch angle of 0° and gantry angles ranging from 181° to 179°. The collimator angles followed the angles of the hippocampus, with conditions set at 315°, 45°, and 0°. The energy used was 6 MV with a flattening filter (FF). (Fig. 2)
Evaluation of treatment plans
To evaluate uniform dose distribution in the tumor tissue and assess the reduction in dose to normal organs, we first calculated the Homogeneity Index (HI) [Equation 1] and Conformity Index (CI) [Equation 2] of the dose distribution [13, 14].

D5%= Dose delivered to 5% of the PTV
D95%= Dose delivered to 95% of the PTV

TV = Target Volume
A value close to 1.0 for both the Conformity Index (CI) and Homogeneity Index (HI) indicates an ideal dose distribution in the target
All treatment plans were delivered using a linear accelerator (Versa HD, Elekta, SE) and Tomo Therapy (Radixact, Accuray). The accuracy of the dose distribution was validated using a quantitative evaluation method called the Gamma Index, which combines the actual dose difference (DD) and distance-to-agreement (DTA). Based on this validation, the dose comparison was performed for critical organs at risk, including bilateral eyeballs, optic nerves, lenses, brainstem, and hippocampus. For brain dose evaluation, the average dose, low-dose region (V5Gy), and dose levels of 1/3 (D33%), 2/3 (D67%), and 3/3 (D100%) of the brain tissue, according
to the evaluation criteria from Emami et al.'s study, were considered. Additionally, the beam on time (BOT) and Monitor Units (MU) of each treatment plan were compared. [15]
Results
Evaluation of Planning Target Volume (PTV)
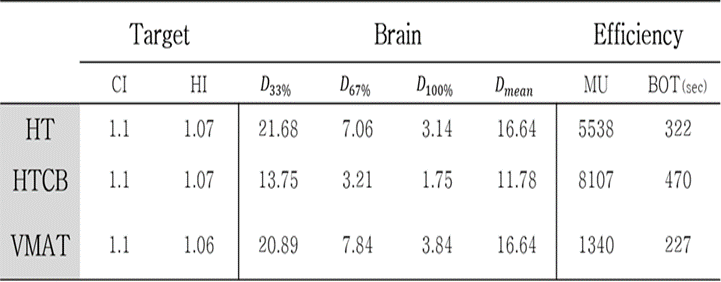
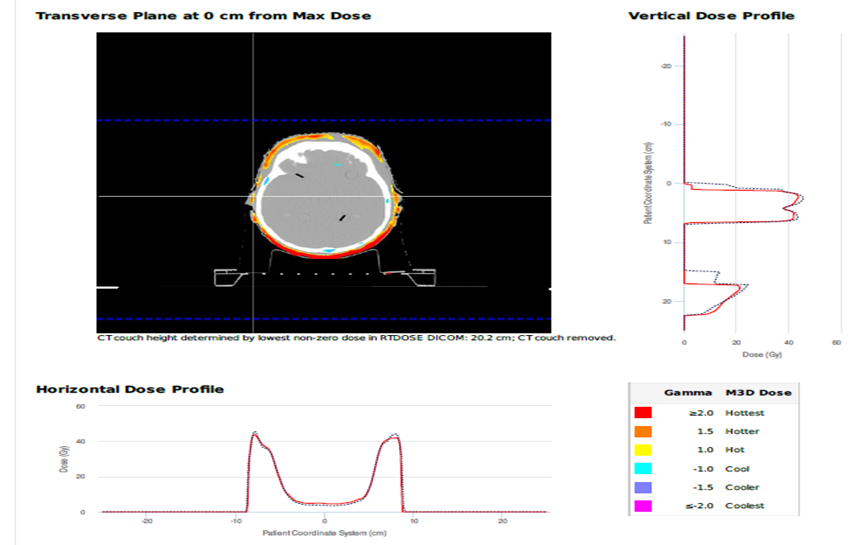
When the prescribed dose was normalized to be included in 95% of the PTV, the Conformity Index (CI) values for HT, HTCB, and VMAT were all 1.1, and the Homogeneity Index (HI) values were 1.07, 1.07, and 1.06, respectively (Table 2). Furthermore, a Delivery QA was conducted to verify the dose distribution in the treatment plan, and it met the criteria of a local gamma passing rate of 3 mm/3% (95% confidence interval) (Fig. 3).
Table 2. Comparison of treatment plans
a) Helical Tomo Therapy
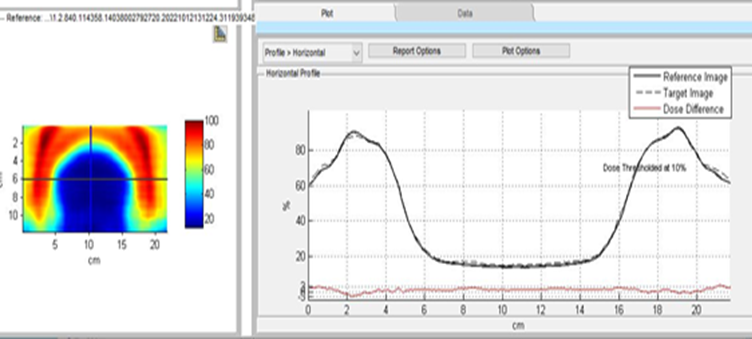
b) Helical Tomo Therapy with Complete Block
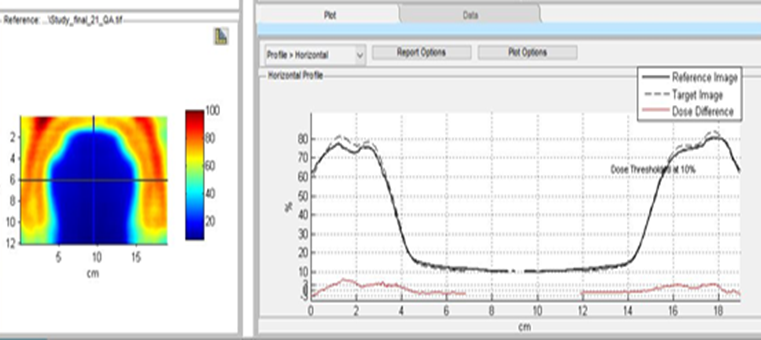
c) Volumetric Modulated Arc Therapy,
Comparison of Dose to Organs at Risk (OAR)
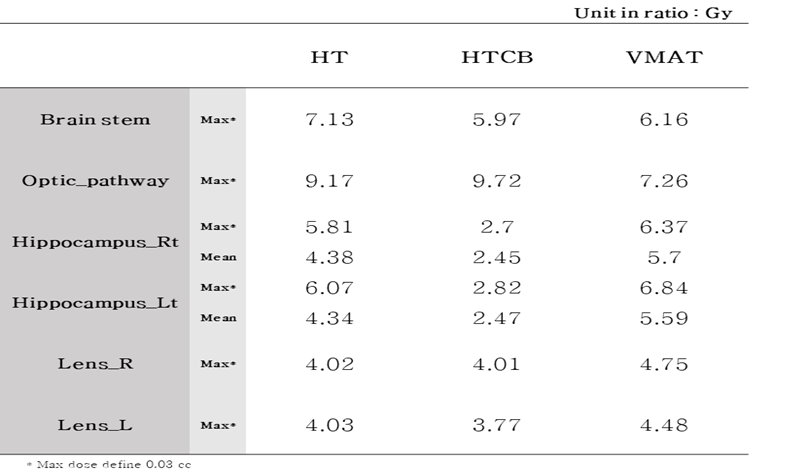
For the brain tissue, the dose values at D33% were 21.68 Gy, 13.75 Gy, and 20.89 Gy for HT, HTCB, and VMAT, respectively. The dose values at D67% were 7.06 Gy, 3.21 Gy, and 7.84 Gy, and the dose values at D100% were 3.14 Gy, 1.75 Gy, and 3.84 Gy for HT, HTCB, and VMAT, respectively. The Dmean values were 16.64 Gy, 11.78 Gy, and 16.64 Gy for HT, HTCB, and VMAT, respectively. The HTCB plan generally showed lower dose values compared to the other plans (Table 2, Fig. 4). When assessing the low-dose region with a threshold of 5 Gy, the V5Gy values were 87%, 49%, and 96% for HT, HTCB, and VMAT, respectively (Fig. 5). Additionally, for other dose values under the same constraint, the maximum dose to the brainstem, hippocampus, and bilateral eyeballs, excluding the optic nerves, was lowest in the HTCB plan. (Table 3)
Table 3. OAR results of HT, HTCB and VMAT plan
Monitor Units (MU) and Beam on Time
To evaluate the efficiency of radiation therapy, MU and beam on time were compared. The beam on time was 322 seconds, 470 seconds, and 227 seconds for HT, HTCB, and VMAT, respectively, with VMAT having the lowest value. The MU values were 5538, 8106, and 1340 for HT, HTCB, and VMAT, respectively, with VMAT showing the lowest value (Table 2).
Conclusion
The low-dose radiation effect on the brain is known to disrupt the blood-brain barrier, and minimizing the radiation dose to the whole brain, along with reducing the dose to the hippocampus, can help mitigate radiation-induced neurotoxicity due to blood-brain barrier disruption and subsequent chemotherapy. (3) Therefore, in this study, we compared and evaluated the dose distribution in normal brain tissue for HT, HTCB, and VMAT treatment plans to select treatment planning methods and equipment that benefit from the advantages of tangential irradiation.
As a result, when the prescribed dose was normalized to be included in 95% of the planning target volume (PTV), the CI values for HT, HTCB, and VMAT plans were all 1.1, and the HI values were 1.07, 1.07, and 1.06, respectively. There was not a significant difference in the evaluation indices for the PTV volume among the treatment plans.
However, for brain tissue, the HTCB plan showed the lowest values for D33% 13.75 Gy, D67% 3.21 G, and D100% 1.75 Gy. The mean dose Dmean for the HTCB plan was 11.78 Gy, while it was 16.64 Gy for both HT and VMAT plans. The V5Gy values were 87% and 96% for HT and VMAT plans, respectively, but only 49% for the HTCB plan, indicating a significant reduction in the low-dose region. Moreover, the maximum hippocampal dose in the HTCB plan was reduced by approximately 4 Gy (2.82 Gy on the left and 2.7 Gy on the right) compared to the VMAT plan (6.84 Gy on the left and 6.37 Gy on the right). Additionally, when comparing the MU values and beam on time (BOT), the VMAT plan had the lowest values. These findings suggest that VMAT may be beneficial for patients who prioritize reduced treatment time, and contrary to previous research results highlighting the advantages of Tomo Therapy in dose distribution, VMAT can also achieve a similar dose distribution in normal brain tissue. [7]
However, it should be noted that even low doses can affect cognitive function. Therefore, Tomo Therapy, which effectively reduces the low-dose region, is considered a good alternative. This is because Tomo Therapy has unique geometric characteristics that allow intensity modulation for all voxels through binary multileaf collimators (MLC) and spiral pitch, enabling effective restriction of the low-dose region. (16,17) According to the RTOG study, it has been reported that in fractionated brain radiation therapy for benign and low-grade brain tumors, an equivalent dose in 2 Gy (EQD2) with a biological equivalent dose (BED) higher than 7.3 Gy (assuming an α/β ratio of 2 Gy) is associated with bilateral hippocampal neurocognitive function impairment. In our study, by using the Complete Block technique, we were able to minimize the dose to the hippocampus and other organs at risk within the brain, along with reducing the overall brain tissue dose. This treatment plan demonstrates the potential to reduce the probability of radiation-induced brain damage and related side effects such as cognitive function decline. [18]
In the future, additional research should be conducted to establish the advantages of tangential irradiation for ring-shaped targets treated in various regions such as the abdomen, upper extremities, and lower extremities. If such research is carried out, it may be possible to achieve dose-optimized results without increasing the burden on patients and treatment facilities by applying Tomo Therapy treatment plans using the Complete Block method.
References
- Wolden, S. L., Barker, C. A., Kushner, B. H., Bodduluri, H., Della‐Biancia, C., Kramer, K., ... & Cheung, N. K. V. (2008). Brain‐sparing radiotherapy for neuroblastoma skull metastases. Pediatric Blood & Cancer, 50(6), 1163-1168.
- Tofilon, P. J., & Fike, J. R. (2000). The radioresponse of the central nervous system: a dynamic process. Radiation research, 153(4), 357-370.
- Dunlop, A., Welsh, L., McQuaid, D., Dean, J., Gulliford, S., Hansen, V., ... & Newbold, K. (2015). Brain-sparing methods for IMRT of head and neck cancer. PLoS One, 10(3), e0120141.
- Lee, P. W., Hung, B. K., Woo, E. K., Tai, P. T., & Choi, D. T. (1989). Effects of radiation therapy on neuropsychological functioning in patients with nasopharyngeal carcinoma. Journal of neurology, neurosurgery, and psychiatry, 52(4), 488.
- Abayomi, O. K. (2002). Pathogenesis of cognitive decline following therapeutic irradiation for head and neck tumors. Acta Oncologica, 41(4), 346-351.
- Cheung, M. C., Chan, A. S., Law, S. C., Chan, J. H., & Vincent, K. T. (2000). Cognitive function of patients with nasopharyngeal carcinoma with and without temporal lobe radionecrosis. Archives of Neurology, 57(9), 1347-1352.
- Song, J. H., Jung, J. Y., Park, H. W., Lee, G. W., Chae, S. M., Kay, C. S., & Son, S. H. (2015). Dosimetric comparison of three different treatment modalities for total scalp irradiation: the conventional lateral photon–electron technique, helical tomotherapy, and volumetric-modulated arc therapy. Journal of radiation research, 56(4), 717-726.
- Mizuno, T., Tomita, N., Takaoka, T., Tomida, M., Fukuma, H., Tsuchiya, T., & Shibamoto, Y. (2021). Dosimetric comparison of helical tomotherapy, volumetric-modulated arc therapy, and intensity-modulated proton therapy for angiosarcoma of the scalp. Technology in Cancer Research & Treatment, 20, 1533033820985866.
- Wojcicka, J. B., Lasher, D. E., McAfee, S. S., & Fortier, G. A. (2009). Dosimetric comparison of three different treatment techniques in extensive scalp lesion irradiation. Radiotherapy and Oncology, 91(2), 255-260.
- Ostheimer, C., Hübsch, P., Janich, M., Gerlach, R., & Vordermark, D. (2016). Dosimetric comparison of intensity-modulated radiotherapy (IMRT) and volumetric modulated arc therapy (VMAT) in total scalp irradiation: a single institutional experience. Radiation oncology journal, 34(4), 313.
- Agazaryan, N., Tenn, S., Liu, A., Chow, P., Lee, C., Alexander, S., ... & Steinberg, M. (2010). SU‐GG‐T‐573: Total Scalp Irradiation: Comparison between Volumetric Modulated Arc Therapy, Helical Tomotherapy and Conventional Electron and Photon Field Combination. Medical Physics, 37(6Part25), 3319-3319.
- Orton, N., Jaradat, H., Welsh, J., & Tomé, W. (2005). Total scalp irradiation using helical tomotherapy. Medical Dosimetry, 30(3), 162-168.
- Kataria, T., Sharma, K., Subramani, V., Karrthick, K. P., & Bisht, S. S. (2012). Homogeneity Index: An objective tool for assessment of conformal radiation treatments. Journal of medical physics/Association of Medical Physicists of India, 37(4), 207.
- Menon, S. V., Paramu, R., Bhasi, S., & Nair, R. K. (2018). Evaluation of plan quality metrics in stereotactic radiosurgery/radiotherapy in the treatment plans of arteriovenous malformations. Journal of Medical Physics, 43(4), 214.
- Emami, B., Lyman, J., Brown, A., Cola, L., Goitein, M., Munzenrider, J. E., ... & Wesson, M. (1991). Tolerance of normal tissue to therapeutic irradiation. International Journal of Radiation Oncology* Biology* Physics, 21(1), 109-122.
- Mizumatsu, S., Monje, M. L., Morhardt, D. R., Rola, R., Palmer, T. D., & Fike, J. R. (2003). Extreme sensitivity of adult neurogenesis to low doses of X-irradiation. Cancer research, 63(14), 4021-4027.
- Rong, Y., & Welsh, J. S. (2011). Dosimetric and clinical review of helical tomotherapy. Expert review of anticancer therapy, 11(2), 309-320.
- Gondi, V., Hermann, B. P., Mehta, M. P., & Tomé, W. A. (2012). Hippocampal dosimetry predicts neurocognitive function impairment after fractionated stereotactic radiotherapy for benign or low-grade adult brain tumors. International Journal of Radiation Oncology* Biology* Physics, 83(4), e487-e493.


