Current Issue : Article / Volume 3, Issue 2
- Case Report | DOI:
- https://doi.org/10.58489/2836-497X/025
About a case: Hematocolpos in a 13-year-old girl
Taddart Casablanca Luxoria 24
Sanaa Benrahhal*
Sanaa Benrahhal, Yasmine Lyafi, Dounia Hachimi, Amine Lamrissi, Naima Samouh, (2024). About a case: Hematocolpos in a 13-year-old girl. Archives of Gynaecology and Women Health. 3(2); DOI: 10.58489/2836-497X/025
© 2024 Sanaa Benrahhal, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 22-07-2024
- Accepted Date: 10-08-2024
- Published Date: 16-08-2024
Hematocolpos, Gynecological examination, MRI
Abstract
Hematocolpos is a rare condition in which the vagina fills with menstrual blood, but this blood cannot drain normally outside the body. The main cause of this condition is usually an abnormal vaginal membrane or septum that partially or completely blocks the exit from the vagina. Diagnosis is based on a thorough gynecological examination, ultrasound and, in the most complex cases, MRI. Early management is essential to avoid complications of vaginal stenosis. We report the case of a 13-year-old girl diagnosed with hematocolpos and a hymenal imperforation, who underwent curettage of the septum with evacuation of the hematocolpos. Post-operative follow-up was favorable.
Introduction
Hematocolpos in adolescents is a rare condition that manifests itself as a distended, blood-filled vagina due to the accumulation of menstrual products caused by uterovaginal abnormalities. The main symptoms at menarche are periodic abdominal pain and primary amenorrhea. Hematometra is a term used to describe the distended, blood-filled uterus caused by extreme accumulation of menstrual products. The main causes of hematocolpos are imperforate hymen, vaginal atresia and complete vaginal septum (1,2). Diagnosis of a vaginal septum is based on a thorough clinical gynecological examination and, above all, on abdominal or transrectal ultrasound, or even transperineal ultrasound and, in more complex cases, MRI. Treatment is surgical and should be carried out as early as possible, as treatment after puberty is associated with a high rate of vaginal stenosis (3).
Case report
This is a 13-year-old patient from a non-consanguineous marriage, with no particular pathological history, menarche at the age of 12, presenting with increasingly incapacitating cyclical pelvic pain with no cycle, urinary or digestive disorders. Clinical examination: normally perforated annular hymen. Pelvic ultrasound showed haematometry (figure 1). On pelvic MRI, blind hemivagina with compressive left hematocolpos over a probable left vulvo-vaginal septum or imperforation (figure 2).
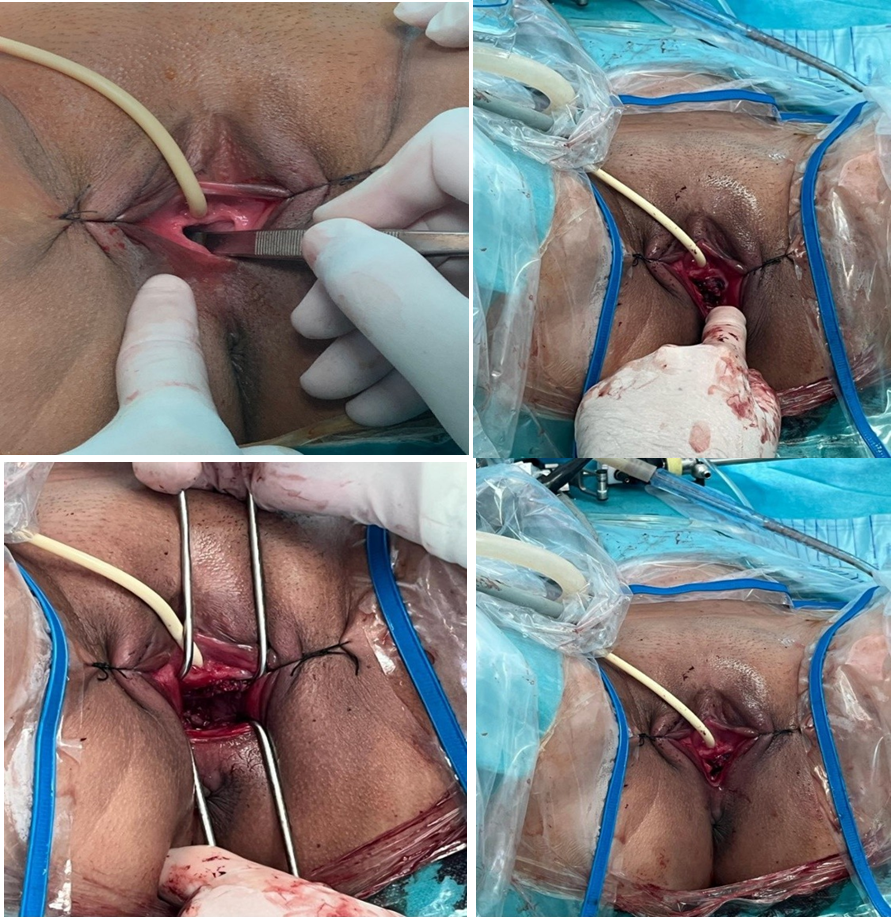
The patient underwent evacuation of the hematocolpos with curettage of the vaginal septum (figures 3). Post-op (figures 4 and 6)
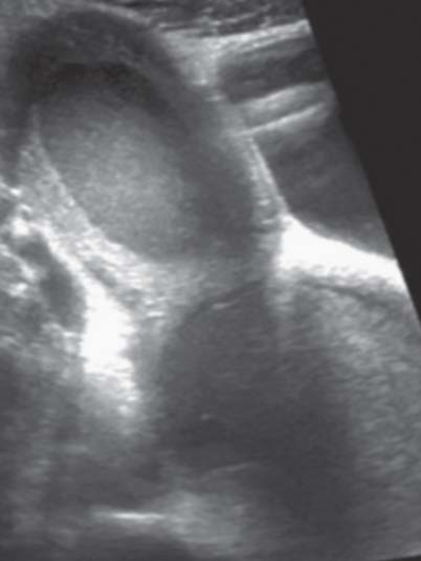
Fig 1: sagittal ultrasound section of a hematocolpos with upstream hematometry
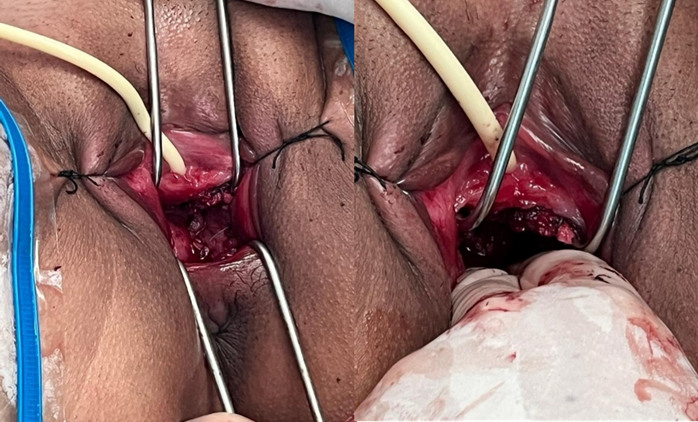
Fig 2: MRI image of compressive hematocolpos with blind hemivagina
Figu 3: Intraoperative perineal view, evacuation of the hematocolpos and cure of the vaginal septum.

Fig 4: post operative evolution
Discussion
Imperforate hymen is the most common obstructive congenital anomaly of the female genital tract, with an incidence of between 0.01% and 0.05% in newborns (4,5). The effect of maternal estrogen secretion during the prenatal or postnatal period can lead to the secretion of mucus by the cervical glands (6). Imperforate hymen, transverse vaginal septum and vaginal atresia with or without a persistent urogenital cloacal sinus are common causes of secretory hydrometrocolpos (7). Hymenal perforation usually occurs during fetal life or the perinatal period (9), but cases of spontaneous hymen rupture have been reported during adolescence (10). The clinical presentation of imperforate hymen is varied, ranging from incidental finding, lower midline abdominal mass with or without prominent hymen, urinary retention, urinary tract infection, acute renal failure, constipation, acute abdomen with paralytic ileus, primary amenorrhea/cyclic abdominal pain and respiratory distress (11). Pelvic, transperitoneal or transrectal ultrasound, if necessary, is used for diagnosis, usually describing a large cystic mass in the pelvis, compressing and displacing the bladder. According to Nussbaum et al (12), the role of ultrasound in such cases includes: defining the nature and complexity of the lesion, including a bulging hymen, detecting associated renal or uterine anomalies, detecting the upper level and length of the obstruction, and the presence and patency of the cervix. CT or MRI may be used for diagnosis, particularly in cases where the transverse vaginal septum is high (13). Rarity, variable presentation and lack of awareness on the part of physicians can lead to delayed diagnosis or unnecessary abdominal exploration (14). Early detection and treatment of obstructive
genital anomalies could lead to 100% reversal of endometriosis. This would, of course, reduce long-term morbidity such as dysmenorrhea and infertility. During the follow-up period of our patients, no endometriosis symptoms such as dysmenorrhea, dyspnea or infertility were reported (15). Standard treatment is surgical hymenectomy with T, X, plus or cruciform incisions and removal of excess hymenal tissue (16). Acar et al (17) reported an incision and placement of a Foley catheter to be left in situ for 2 weeks with topical estrogen cream after a single dose of prophylactic ceftriaxone. In their series, an annular hymen formed and defloration was observed in all patients.
Conclusion
Hematocolpos and vaginal septum are rare medical conditions that can affect women's well-being and reproductive health. By understanding the possible causes, symptoms and treatment options of these conditions, healthcare professionals can provide appropriate support to affected patients. It is essential to consult a doctor in the event of symptoms such as abdominal pain, menstrual difficulties or pain during intercourse, in order to benefit from an accurate diagnosis and a suitable treatment plan. With proper medical management, most women with hematocolpos and vaginal septum can lead healthy, fulfilling lives (18).
Conflict of interest
No conflict of interest
References
- Hein, K. (1984). The first pelvic examination and common gynecological problems in adolescent girls. Women & Health, 9(2-3), 47-63.
- CREATSAS, G., CARDAMAKIS, E., HASSAN, E., DELIGEOROGLOU, E., SALAROS, N., & ARAVANTINOS, D. (1994). Congenital uterine anomalies with obstructed cervix, hemivagina, or both during adolescence: report of 22 cases. Journal of gynecologic surgery, 10(3), 159-167.
- Rock, J. A., & Breech, L. L. (1997). Surgery for anomalies of the mullerian ducts. The Linde’s operative gynecology. 8th ed. Philadelphia: Lippincott-Raven, 687-729.
- Lui, C. T., Chan, T. W. T., Fung, H. T., & Tang, S. Y. H. (2010). A retrospective study on imperforate hymen and haematometrocolpos in a regional hospital. Hong Kong Journal of Emergency Medicine, 17(5), 435-440.
- Mwenda, A. S. (2013). Imperforate Hymen-a rare cause of acute abdominal pain and tenesmus: case report and review of the literature. Pan African Medical Journal, 15(1).
- Yıldırım, G., Gungorduk, K., Aslan, H., Sudolmus, S., Ark, C., & Saygın, S. (2008). Prenatal diagnosis of imperforate hymen with hydrometrocolpos. Archives of gynecology and obstetrics, 278(5), 483-485.
- Celayir, A. C., Kurt, G., Sahin, C., & Cici, I. (2013). Spectrum of etiologies causing hydrometrocolpos. Journal of neonatal surgery, 2(1).
- Garcia Rodriguez, R., Pérez González, J., Garcia Delgado, R., Rodriguez Guedes, A., de Luis Alvarado, M., Medina Castellano, M., & Garcia Hernandez, J. A. (2018). Fetal hydrometrocolpos and congenital imperforate hymen: prenatal and postnatal imaging features. Journal of Clinical Ultrasound, 46(8), 549-552.
- Hegazy, A. A., & Al-Rukban, M. O. (2012). Hymen: facts and conceptions. The Health, 3(4), 109-115.
- Hamouda, B., Ghanmi, S., Soua, H., & Sfar, M. T. (2016). Spontaneous rupture of the imperforate hymen in two newborns. Archives de Pediatrie: Organe Officiel de la Societe Francaise de Pediatrie, 23(3), 275-278.
- Ramareddy, R. S., Kumar, A., & Alladi, A. (2017). Imperforate hymen: varied presentation, new associations, and management. Journal of Indian Association of Pediatric Surgeons, 22(4), 207-210.
- Nussbaum, A. R., Sanders, R. C., & Jones, M. D. (1986). Neonatal uterine morphology as seen on real-time US. Radiology, 160(3), 641-643.
- Burgis, J. (2001). Obstructive Müllerian anomalies: case report, diagnosis, and management. American journal of obstetrics and gynecology, 185(2), 338-344.
- Patton, P. E., Novy, M. J., Lee, D. M., & Hickok, L. R. (2004). The diagnosis and reproductive outcome after surgical treatment of the complete septate uterus, duplicated cervix and vaginal septum. American journal of obstetrics and gynecology, 190(6), 1669-1675.
- Sanfilippo, J. S., & Lara-Torre, E. (2009). Adolescent gynecology. Obstetrics & Gynecology, 113(4), 935-947.
- Jones, H. W., & Rock, J. A. (2015). Te Linde's operative gynecology. Lippincott Williams & Wilkins.
- Ali, A., Çetin, Ç., Nedim, Ç., Kazım, G., & Cemalettin, A. (2003). Treatment of imperforate hymen by application of Foley catheter. European Journal of Obstetrics & Gynecology and Reproductive Biology, 106(1), 72-75.
- Bailey KV, Ashburn JC. Vaginal Septum. [Updated 2021 Jul 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan


