Current Issue : Article / Volume 3, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-3582/013
Acute Cardiac Tamponade Following Adult Allogeneic Hematopoietic Transplantation
1Houston Methodist Hospital, Houston, USA.â¯
2Center for Cell and Gene Therapy, Baylor College of Medicine and Houston Methodist Hospital, USA
Rammurti Kamble M.D
Rammurti Kamble, et.al., (2024). Acute Cardiac Tamponade Following Adult Allogeneic Hematopoietic Transplantation. Journal of Hematology and Disorders. 3(1); DOI: 10.58489/2836-3582/013
© 2024 Rammurti Kamble, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 30-05-2024
- Accepted Date: 07-06-2024
- Published Date: 12-07-2024
Cardiac tamponade, Pericardial effusion, Allogeneic hematopoietic transplant
Abstract
Large pericardial effusions (LPEs) and consequent acute cardiac tamponade (ACT) are rare in adult hematopoietic transplants. Amongst 553 allogeneic hematopoietic transplantation (allo-HCT), a total of 5 (0.9%) developed ACT at <100 days from allo-HCT (days +1, +16, + 22, +60 and day +91). The median time to neutrophilic engraftment was 20 days (range, 12-30). ACT preceded engraftment in 3 patients. ACT manifested as acute, new, or worsening shortness of breath. All 5 patients had no acute GvHD (aGVHD) or CMV reactivation/infection. Pericardial fluid was serous in 2 and serosanguinous in 3 patients. A cumulative total of 1700 ml, 1500 ml, 150 ml, 300 ml, and 800 ml pericardial fluid were removed. Laboratory analysis did not support bacterial or viral etiology and rheumatologic profiles were negative. Histology of pericardial tissue from 2 patients who underwent pericardial window showed benign fibro adipose tissue with reactive mesothelial tissue with fibrous adhesions. There was no evidence for acute inflammatory or infectious processes. We highlight LPE development as a possible severe complication in patients undergoing allo-HCT that requires prompt intervention.
Introduction
Allogeneic stem cell transplant (allo-HCT) is commonly utilized for a variety of hematological disorders. Frequently reported adverse outcomes include, graft-versus-host-disease (GVHD), infections, volume overload, engraftment syndrome, veno-occlusive disease, transplant associated microangiopathy amongst others [1]. Development of LPEs following allo-HCT is relatively common in the pediatric population with reported incidence of up to 17.6-21% [2]. In adults however, LPEs are distinctly uncommon with reported incidence of <1>not associated with acute GVHD, but rather, with cardiac toxicity from conditioning regimens [1]. In comparison, the development of late LPE (after 100 days) is mostly thought to be related to chronic GVHD-related serositis [5].
The major determinant of whether a pericardial effusion will cause acute pericardial tamponade (ACT) is the rapidity with which fluid accumulates. A chest X-ray may not show cardiomegaly in ACT as at least 200 ml of pericardial fluid must accumulate before enlargement of cardiac silhouette [6].
We herein document development of ACT within first 100 days of allo-HCT in 4 patients and discuss the clinical manifestations that are unique to allo-HCT patients, relationship to GvHD, therapeutic interventions and recurrences.
Methods
Following approval from the Institutional Review Board (IRB), patient, disease and transplant characteristics were analyzed. Between August 2008 and June 2023, a total of 512 patients underwent 553 allo-HCTs at our Institution. Donor source comprised of matched sibling donor (MSD) in 130, mismatched sibling donor (MMSD) in 1, matched unrelated donor (MUD) in 249, mismatched unrelated donor (MMUD) in 132 and haploidentical (Haplo) donor in 41 allo-HCT) ACT was defined by pericardial effusion leading to cardiac tamponade on echocardiogram. Early LPE was defined by development of LPE within 100 days of allo-HCT; those that developed after 100 days were labeled late LPEs. A total of 5 (0.9%) ACT occurred among 533 allo-HCT.
Patients were evaluated by cardiologists who facilitated ACT management. All patients underwent therapeutic pericardial paracentesis and placement of pericardial drain or pericardial window. Cumulative total pericardial fluid volume drain was calculated. Pericardial fluids were analyzed for cell counts, cellular differential, chemistry, LDH, viral infections (CMV, HHV-6, adenovirus and coxsackievirus) and tuberculosis. Engraftment was characterized by three consecutive days of absolute neutrophils over 500 and platelets count of over 20,000. Engraftment syndrome was defined by presence of fever, rash and non-cardiogenic pulmonary edema after neutrophil engraftment. When available, laboratory parameters for immunological and or systemic collagen vascular disorders were collected. Pericardial histology was available in 2 patients who underwent pericardial window.
Results
We identified 5 adult patients between August 2008 and June 2023 with early LPEs that led to ACT. As reported in Table 1, the median age of 3 females and 2 male was 50 years (range 19-65). All but 1 patient (#5) received high-dose cyclophosphamide either as part of conditioning or post-transplant GvHD prevention. Conditioning comprised of: Busulfan, Fludarabine and Thiotepa and post-transplantation Cyclophosphamide (n=1), Cyclophosphamide, Total Body Irradiation and Alemtuzumab (n=2), or cyclophosphamide and anti-thymocyte globulin (n=1), Busulfan, Clofarabine (n=1). Donors were MUD (n=3), MSD (n=1), or haplo (n=1).
The median time to neutrophil engraftment was 20 days (range, 12-21 days). All 5 patients developed ACT at less than 100 days from allo-HCT on days +1, +19, + 22, +60 and +91 after allo-HCT. ACT manifested as acute, new or worsening shortness of breath. Three patients developed LPE before engraftment. At the time of ACT, all were negative for CMV infection and acute GvHD (aGVHD). Pericardial fluid was serous in 2 and serosanguinous in 2 patients. Laboratory analysis did not support bacterial (e.g., tuberculosis) or viral (e.g., CMV, HHV-6, adenovirus and coxsackievirus) infections, and rheumatologic profiles were negative. ACT was treated with either pericardiocentesis with pericardial drain or pericardial window. A cumulative total of 1700 ml, 1500 ml, 150 ml,300 ml, and 800 ml pericardial fluid were removed from each of the patients. LPEs reoccurred in 2 patients (Patient 1 and 2); one recurrence (Patient 2) necessitated pericardial drainage for ACT physiology. Additionally, all patients received short courses of corticosteroids.
For Patients 2 and 4, who underwent placement of pericardial windows, biopsies of the pericardial tissue were negative for infection and acute inflammation. Patient 2 had benign fibroadipose tissue with reactive mesothelial tissue and skeletal muscle. Patient 4’s biopsy revealed skeletal muscle fibers and fibroadipose tissue with focal fibrous adhesions.
At median follow-up of 40 months (range, 6-165 months), 3 of the 5 patients are alive after alloHCT. None of the LPE was associated with acute GvHD. No patient developed constrictive pericarditis. Patient 2 relapsed with leukemia at 60 days post allo-HCT. Three months after her first transplant, she received a second transplant (5.946X106 CD34/kg cells) from the same donor. She was conditioned with cyclophosphamide, total body irradiation, and alemtuzumab (Campath) for her first transplant, then alemtuzumab for 3 days for the second transplant. A bone marrow biopsy on day +30 showed no leukemia. ACT occurred on Day +60 from her second transplant. Unfortunately, on day +150 she was hospitalized with mycobacterium avium pneumonia and disseminated Mucormycosis to which she succumbed. Patient 3’s who developed ACT day-1 had transient HHV-6 viremia on Day +12 which responded to foscarnet. This patient continues to be in good health 16 years post-transplant.
Table 1: Patient, disease, and transplant characteristics.
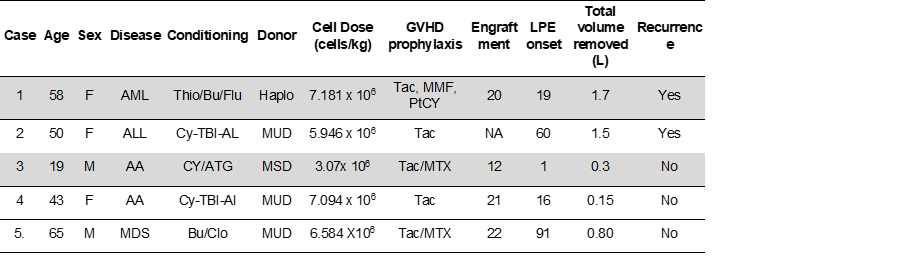
AML= Acute myeloid leukemia, ALL= Acute Lymphoblastic Leukemia, Thio= Thiotepa, Bu= Busulfan, Flu= Fludarabine, Haplo= Haploidentical, Tac= Tacrolimus, MMF= Mycophenolate sodium, PtCY= Post-transplant Cyclophosphamide, Cy= Cyclophosphamide, TBI= Total body Irradiation, Al= Alemtuzumab, MUD= Matched Unrelated Donor, MTX= Methotrexate, AA= Aplastic Anemia, ATG= Anti Thymocyte Globulin, MDS= Myelodysplastic Syndrome, Clo =Clofarabine
Discussion
Although rare, LPE in adult allo-HCT can lead to life threatening ACT. In patients undergoing allo-HCT, recognition of ACT is complex. These patients can develop dyspnea, chest pain, hypotension, tachycardia or syncope from a variety of causes. A chest X-ray may not show cardiac enlargement as development of ACT depends on the rapidity of pericardial fluid collection rather than total volume of fluid. High index of suspicion leading to prompt cardiac doppler echocardiogram is therefore necessary. We did not find a correlation of ACT with engraftment, engraftment syndrome, volume overload or acute GvHD.
Our results are similar to those reported in the literature. A single-center retrospective study of 620 adults who received allo-HCTs, identified 20 (3.2%) who developed pericarditis. Of these, only 2 (0.32%) developed LPE and cardiac tamponade [5]. A report of 12 adult patients identified the following risk factors for LPE: Age over 50, multiple allo-HCT, and presence of chronic GvHD [3]. The median time for onset of LPE for all 12 patients was 270 days after transplant. Of these, 3 patients had early-onset LPE at days +9, +14, and +25. While two of these patients received conditioning regimens of cyclophosphamide and total body irradiation (TBI); the third received a fludarabine-based regimen. The authors concluded that late-onset LPE was significantly associated with chronic GVHD, while early-onset LPE is associated with conditioning with cyclophosphamide. These results were similar to an earlier retrospective single-institution study of 346 allo-HCT patients between 2005 and 2008 that identified 2 patients with early-onset large LPE at +42 and +51 days [7]. Interestingly, both patients had just undergone their second transplant. In the 7 total patients who developed early or late LPE, median time to diagnosis was 229 days (range, 42-525 days), and 6 had concurrent pleural effusions consistent with polyserositis seen in GVHD [7]. In addition to conditioning with cyclophosphamide, early LPE in particular is associated with late neutrophil engraftment and transplant - associated microangiopathy (TA-TMA) [1, 8].
In the absence of GVHD-related serositis, we can only postulate what may have led to these LPE. Potential causative factors include cyclophosphamide cardiotoxicity, fluid overload, capillary leak syndrome, engraftment syndrome, TA-TMA, and autoimmune phenomenon. Cyclophosphamide dose-dependent cardiotoxicity can potentially be augmented with prior myocardial irradiation and/or previous anthracycline exposure [9]. Three of the 4 patients described here received cyclophosphamide as part of conditioning or post-transplant GVHD prophylaxis. Through direct oxidative damage to the myocardium and endothelial cell damage, cyclophosphamide causes capillary microthrombosis and fibrin deposition, potentially leading to heart failure and arrhythmias [9]. On autopsy, patients may have myocardial edema or necrosis, serosanguinous pericardial effusions, and fibrinous pericarditis [9]. Notably, in the cases presented, fluid analysis has shown largely serous or serosanguinous transudative fluid with normal levels of nucleated cells, mesothelial cells, and (when available) protein. For the patients who underwent pericardial window placement, biopsy was negative for infiltrative disease, but showed signs of possible active or resolving inflammation through reactive mesothelial tissue and fibrous adhesions. This would appear to implicate a role for high-dose cyclophosphamide in the development of LPE. In 2 patients LPE occurred days before engraftment while in another, it was during the peri-engraftment period.
After pericardial drainage, there is no consensus on systemic treatment for serositis. Though diuretics help alleviate the associated fluid overload; it has very little impact on LPE. Corticosteroids are commonly offered to counter inflammation, while non-steroidal anti-inflammatory are generally avoided given concurrent thrombocytopenia. Colchicine, which is commonly used in pericarditis may also be difficult to administer due to its potential adverse effect of marrow suppression and the development of cytopenia.
References
- Kubo, H., Imataki, O., Fukumoto, T., Oku, M., Ishida, T., Kubo, Y. H., ... & Kadowaki, N. (2021). Risk factors for and the prognostic impact of pericardial effusion after allogeneic hematopoietic stem cell transplantation. Transplantation and Cellular Therapy, 27(11), 949-e1.
- Cox, K., Punn, R., Weiskopf, E., Pinsky, B. A., & Kharbanda, S. (2017). Pericardial effusion following hematopoietic cell transplantation in children and young adults is associated with increased risk of mortality. Biology of Blood and Marrow Transplantation, 23(7), 1165-1169.
- Liu, Y. C., Chien, S. H., Fan, N. W., Hu, M. H., Gau, J. P., Liu, C. J., ... & Tzeng, C. H. (2015). Risk factors for pericardial effusion in adult patients receiving allogeneic haematopoietic stem cell transplantation. British Journal of Haematology, 169(5), 737-745.
- Pfeiffer, T. M., Rotz, S. J., Ryan, T. D., Hirsch, R., Taylor, M., Chima, R., ... & Dandoy, C. (2017). Pericardial effusion requiring surgical intervention after stem cell transplantation: a case series. Bone marrow transplantation, 52(4), 630-633.
- Freyer, C. W., Fradley, M., Madnick, D., Carver, J. R., Frey, N. V., Gill, S. I., ... & Loren, A. W. (2021). Characterization of pericarditis following allogeneic hematopoietic cell transplantation. Transplantation and Cellular Therapy, 27(11), 934-e1.
- Spodick DH. Acute cardiac tamponade. N Engl J Med. 2003 Aug 14;349(7):684-90.
- Norkin, M., Ratanatharathorn, V., Ayash, L., Abidi, M. H., Al-Kadhimi, Z., Lum, L. G., & Uberti, J. P. (2011). Large pericardial effusion as a complication in adults undergoing SCT. Bone marrow transplantation, 46(10), 1353-1356.
- Postalcioglu, M., Kim, H. T., Obut, F., Yilmam, O. A., Yang, J., Byun, B. C., ... & Abdi, R. (2018). Impact of thrombotic microangiopathy on renal outcomes and survival after hematopoietic stem cell transplantation. Biology of Blood and Marrow Transplantation, 24(11), 2344-2353.
- Dhesi, S., Chu, M. P., Blevins, G., Paterson, I., Larratt, L., Oudit, G. Y., & Kim, D. H. (2013). Cyclophosphamide-induced cardiomyopathy: a case report, review, and recommendations for management. Journal of investigative medicine high impact case reports, 1(1), 2324709613480346.


