Archive : Article / Volume 1, Issue 2
- Research Article | DOI:
- https://doi.org/10.58489/2836-2179/009
Balanced Scorecard applied to Hospital Units - a systematic review of the literature
PhD student at the School of Economics and Management of Minho University, and is a professor of Accounting and Management.
Paula Cristina de Almeida Marques
Paula C. de A. Marques, (2022). Balanced Scorecard applied to Hospital Units - a systematic review of the literature. Journal of Emergency and Nursing Management. 1(2). DOI: 10.58489/2836-2179/009
© 2022 Paula C. de A. Marques, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 13-10-2022
- Accepted Date: 24-10-2022
- Published Date: 29-12-2022
BSC, Health, Hospital, Performance Evaluation
Abstract
As a result of the reality currently experienced in the health sector, where there is an increase in competitiveness and where cost control is increasingly evident, performance management in this area is distinct and more complex, compared to other areas. Thus, the Balanced Scorecard (BSC) emerged as the ideal tool to improve the performance of healthcare organizations.
The BSC is a management tool with the potential to clarify the strategic objectives of health organizations and to assist in the selection of the most appropriate performance indicators to use. For its success, it is important to align the organization's strategy with the services' strategy, as well as the involvement of managers.
This investigation has as main objective to make a diagnosis of the state of the art, regarding the implementation of the BSC in Hospital Units. To achieve this objective, a systematic review of the literature was carried out and nine questions related to the objective in question were answered.
From the investigation carried out, 24 articles were selected for the literature review, which met the inclusion criteria. From the analysis of these articles, it was possible to conclude that the implementation of this tool can represent an added value for the success of health organizations in general, and of Hospital Units in particular. Empirical evidence suggests that, through the implementation of the BSC, Hospital Units have managed to increase their level of quality, the satisfaction of users and professionals, as well as contributing to their efficiency and effectiveness. However, and despite its benefits, the implementation of the BSC is still not a linear process, with several limitations and/or difficulties being identified in the design and implementation process of this tool.
Conclusion
With this systematic literature review, our objective was to explore and understand the state of the art on BSC in Hospital Units. This tool is increasingly important in the health sector and, as such, it is pertinent to understand what had already been studied, thus allowing a better understanding of the subject.
The BSC is a management tool that initially appeared in 1992, by the hands of Kaplan and Norton, aimed at the private sector; only later did it gain relevance within health organizations and in the public sector. It is currently considered a very useful tool in the private sector, in the public sector, in the public-private sector and in the social sector. Traditionally made up of four perspectives, with the advancement of knowledge about this tool, it has already been possible to find new perspectives, which reflect, on the one hand, the need for organizations to move towards efficiency and, on the other hand, the permeability/flexibility of the BSC. to the needs of organizations. Regarding the indicators outlined for each perspective, they vary greatly from application to application, however,
Although all publications mention the importance that this tool assumes in the field of health, there are still many gaps in terms of its implementation. Kompouros (2013) points out as one of these gaps the reluctance to change, which, in many cases, can be due to the lack of knowledge about the BSC, the lack of a quality culture within organizations (El-Jardali et al., 2011) or the inability of leadership to communicate the purpose of implementing the BSC (Rabbani et al., 2011). It is thus clear that it is extremely important to create specific teams for the implementation of this tool, and that they are in the field, monitoring and evaluating the work developed, transmitting the feedback to the service, department and/or hospital institution and making adjustments as necessary.
Although not all the analysed publications specify the benefits achieved with the implementation of the BSC, those that do point to an increase in the satisfaction of users and professionals, an increase in quality and efficiency. The analysed literature is consensual, with regard to the main motivation for the implementation of the BSC, recognizing its potential as a driver for the improvement of care provided, as a performance evaluation system.
With the answer to each of the questions initially raised, we can reach some conclusions, which we refer to in the next paragraphs.
Most of the studies found were carried out in the last decade, they are mostly qualitative and were published in reputable magazines and newspapers in this area. Overall, these studies aimed to better understand the BSC tool and clarify its impact on improving the performance of Hospital Units.
Regarding the main motivation pointed out by the researchers for carrying out the study, those most frequently mentioned are related to the need to develop a performance evaluation system for Hospital Units and to deepen knowledge and empirical research on the application of this tool.
According to the publications analysed, the Public Sector Hospital Units are the ones where the BSC was most applied. With regard to geographic distribution, most studies were carried out in Asia and North America, with only four studies being identified in Europe.
Also, according to the reports found, it appears that during the design and implementation of the BSC, top management and direction, health professionals, reference professionals from each sector where the BSC is intended to be implemented, a panel of experts must be involved. in this tool, users and academics.
With regard to perspectives, the most frequently used is the financial perspective that takes the lead. Although most studies use the perspectives of the Kaplan and Norton model, some studies adapt them, and there are even studies that create new perspectives, it seems to us that this innovation is closely associated with the need to adapt to the reality of each organization. With regard to indicators, from the Customers perspective, the most used indicators are those related to the satisfaction rate: from the financial perspective, the most used are related to costs and expenses, margin and level revenue; from the Internal Processes perspective, the most used indicators are those related to the time factor, satisfaction, professional incidents and occupation, finally, from the Learning and Knowledge perspective, there is a large reference to indicators related to training and research, investment in technology and the environment organizational.
Regarding the elements pointed out as facilitators in the different publications, it is clear that open communication, the dissemination of results and the involvement of top managers contribute to the success in the design and implementation of this tool.
From the results found in the different publications, it is noticeable that the great advantage of the design and implementation of the BSC is to contribute to the improvement of the performance of Hospital Units.
Regarding the difficulties/limitations in the design and implementation of this tool, those that are most frequently mentioned are related to access to information, lack of collaboration with researchers, scarcity of human resources, and difficulties related to data (the way of data collection, timing, form of analysis). It is important to identify these limitations/difficulties as a way to overcome them in future investigations.
From the literature found, it is clear the importance that this tool assumes and it is understood that, increasingly, its positive impact at the level of organizations is recognized.
Investigation Limitations
During this literature review, the small number of studies found that met the inclusion criteria, the lack of articles that described the implementation of the BSC in Portugal and that were written in English and the difficulty of accessing to some studies identified as potentially interesting. Another of the limitations felt is related to the fact that not all studies identified indicators for each perspective, nor approach the BSC in the same way, which made the comparative analysis of the different works and the interpretation of data difficult.
Considering the limited time to carry out the study, the search only through the title became necessary, however it proved to be a limitation, and it may have left out some relevant studies.
Research Suggestions
For future investigations, it is suggested that a literature review be carried out with studies carried out in Portugal, in the health area, and that a comparison be made with the results obtained in other countries. Another suggestion is to broaden the inclusion criteria, as well as to review the descriptors, in an attempt to obtain a greater number of studies that allow more generalizations.
Also, according to the analyzed articles, we consider that in future investigations it would be important to apply the BSC complemented with other management tools, to compare the BSC and other performance evaluation methods and to carry out comparative studies between hospitals with the same characteristics in order to understand what factors can influence the application of this tool.
Introduction
According to data from the Organization for Economic Cooperation and Development (2015), Portugal spends more on the health sector than most countries, with hospitals responsible for more than half of public expenditure associated with health care (Alves, 2016). The aging of the population, technological advances, the pressure to reduce public expenditure associated with health care and the growing interest of the private and social sector in this area, raise challenges in the sector, making performance management in this area distinct and complex compared to other areas (Joyce, 2003). Consequently, the need to develop strategic and action plans arose, benchmarking gained prominence, and conditions began to be met for the application of the Balanced Scorecard (BSC) (Calhau, 2009).
The BSC emerged in 1992 with the aim of improving performance measurement systems in the private sector, but quickly gained prominence in the public sector (Alkaabi, Chehab & Selim, 2019). In Portugal, it was no different and came to help organizations in the effective measurement of organizational performance and in the implementation of strategies. It is a performance evaluation model that makes it possible to clarify the organization's objectives and the most appropriate indicators to be used, requiring alignment between the service's strategy and the organization's strategy, as well as the involvement of top and middle managers., for the success of the established methodology (Ojah, Malik & Ali, 2019; Freitas, 2015; Macedo, 2014; Pinto, 2013; Jordan, Neves & Rodrigues, 2011; Alvarez, 1999 cited in Santos, 2006;).
According to Al-kaabi, Chehab and Selim (2019), the BSC provides the basis for properly executing the organization's strategy and successfully managing change. For Pinto (2009), its implementation brings significant benefits in improving the performance of public organizations, if there is an alignment between structural changes, strategic priorities and operational efficiency.
This investigation has as main objective to make, through a systematic review of the literature, a diagnosis of the state of the art, regarding the implementation of the BSC in Hospital Units. Using the existing literature on this topic, it is us objective to answer the following questions: What are the characteristics of the publications that report the application of the BSC in hospitals?; What is the motivation for using the BSC?; What are the characteristics of the hospitals where the BSC was implemented?; Who are the actors in the process of designing and implementing the BSC?; What are the perspectives and performance indicators most frequently used in the application of the BSC in hospitals?; What are the facilitating factors in design and implementation?; What are the results obtained with the implementation of the BSC?; What are the difficulties and/or limitations to the implementation of the BSC?; What opportunities exist for future investigations in this area?.
This systematic literature review arises from the need to promote a better understanding of the subject under study, based on scientific evidence. Through a process of search, selection, organization and synthesis of studies on the implementation of this tool in Hospital Units, and, from the scientific knowledge extracted from them, it is intended, through a process of reflection, analysis and discussion of its content , contribute to the clarification and understanding of this tool, and what benefits can come from its implementation, thus facilitating its adoption and development, by presenting a summary of what has been studied worldwide. The aspects for which this systematic literature review stands out in relation to the existing ones are related to the fact that it focuses only on Hospital Units,
This investigation is divided into five chapters. In chapter one the introduction is made. In chapter two, we provide a framework for the tool under analysis, where general notions about the BSC will be discussed, namely: concept, objectives, perspectives, cause-effect relationship and strategic map, as well as the application of the BSC in the health sector. In chapter three, the methodology used during the investigation will be discussed. In chapter four we will present, analyze and discuss the results, based on the selected literature. Finally, in chapter five the conclusions, limitations and suggestions for future work will be presented.
The Balanced Scorecard
The application of the concept of strategy, associated with management, gained prominence in the middle of the last century (Banza, 2013; Silva, 2012; Barcellos, 2002). For Andrews (1980, p.46) “strategy is the pattern of objectives, purposes or goals and main policies and plans for achieving them, expressed in such a way as to define what business the company is or should be in and the type of company that it is. or shall be.” Mintzberg (1987, cited in Grant, 2013), argues that strategy cannot be seen as a single, finished concept, and, in this sense, defines the 5P's of strategy: Plan, an ordered and coherent sequence of actions; Pattern, coherence and consistency in behavior and decision making; Positioning, adjustment between capabilities and actions, and competition conditions in the surrounding environment; perspective, the way the company sees the world and wants to act in it; and Ploy, tactics to use to gain an advantage over the competition.
Mintzberg (1994) also argues that strategy should be seen as something that is shared and transversal to the different members of the organization and that is reflected in their actions and/or intentions. Other authors (Santos, 2008; Freire, 1997) add that the strategy essentially involves a set of decisions and actions, in which the main purpose is to add value to the customer, in the long term, thus leading to customer loyalty. same.
For the concept of strategy, two fundamental aspects should still be highlighted: first, the relevance of the direct influence of strategy on the future of organizations and, second, the definition of objectives, means and ways to achieve them, as well as their operationalization. in practice, they only make sense if thought of in an integrated and coherent way (Silva, 2012). Sometimes, the problem lies in a poor execution of the strategy, and not in a bad definition of it, a consequence of a misinterpretation of the intended.
As a result of changes in the environment where organizations are located, it has been necessary to invest in the development of knowledge and skills of human resources, in the development of strategic thinking and in the creation of models that are able to respond to new paradigms (Santos, 2008).
Strategic management can be seen as a plan that integrates from objectives to processes, and which makes the entire organization act with a view to achieving competitive results, and that guarantee its permanence in the market (Madaleno, 2015). For strategic planning to be successful, it is important that there is an alignment between it and tactical-operational planning, taking into account the internal and external conditions of the organization. There must also be a focus on innovation and differentiation, considering the relationship between the organization and the environment, thus allowing it to function as a whole towards the intended results (Pinto, 2009; Prieto, Carvalho & Fischmann, 2009; Marçal, 2008); Vieira, 2008; Oliveira, 2006). It can thus be said that strategic management seeks to mold itself to the organization, being characterized by its flexibility in the face of changes in the environment, thus allowing managers to have a broader view of the organization.
In summary, strategic management is assumed as a continuous and dynamic process of planning, organization, leadership and control, through which organizations define “where they are”, “where they want to go” and how “to get there”, being to such a clearly defined strategy is essential (Marçal, 2008; Santos, 2008). For this, it is necessary to act in accordance with the pre-defined path, but always adjusting to changes in the surrounding environment, with special relevance to customers' preferences/needs.
In the elaboration and implementation of strategic planning, Oliveira (2006) describes four phases: strategic diagnosis, company mission, prescriptive and quantitative instruments, control and evaluation. As the execution of the strategy is at the heart of the creation of value and the growth of the organization, the evaluation of its implementation must be the responsibility of the organization's leaders, and this process must include the review and adjustment of the strategy, as well as the processes that support it. (Marçal, 2008).
For Madaleno (2015), the clear definition of objectives, the adequate unfolding and linking of the strategy with the processes, as well as the control of its implementation through a performance measurement system, are crucial in order to achieve the organization's objectives. Despite its simplicity, there are many internal threats to strategy implementation, which can be classified into three groups: those that act on strategic orientation, those that affect the ability to learn, and those that affect the ability to implement the strategy (Beer & Eisenstat, 2000).
For the implementation of a strategic management model that leads to the organization's success in a constantly changing environment, Santos (2008) defends the need for commitment, dedication and involvement of top management; the promotion of a motivating environment, where participation is privileged, favorable to change, and where everyone is encouraged to contribute; adequacy of training to functions; an effective communication system; definition of deadlines for the development of the process; simplification and flexibility of the process, seeing it as a means and not an end to obtain and sustain competitive advantages.
Some authors argue that this process works better when there are performance indicators, thus ensuring adherence between processes/operations/strategy, because when performance measures exist, these will serve as a basis for analysis and decision-making (Skrinjar, Bosilj-Vuksic & Stemberger, 2008; Oliveira, Costa & Cameira, 2007).
In view of the great transformations that have been experienced in the health sector, both globally (where Portugal is no exception) and, considering the current economic and financial scenario, it has been necessary to resort to strategic management instruments in order to help organizations to assess their performance, using different approaches, methodologies, instruments and intervention levels, among which the Balanced Scorecard stands out (Serrano, 2017; Russo, 2015).
Fundamental Elements of the Balanced Scorecard
Performance management is defined by Pinto (2009: 30) “as an integrated system, composed of a set of processes, methodologies and solutions”. This concept has been around for many years and is part of the measurement system, where tools allow us to assess, monitor and review performance. The main objective of performance management is to motivate and align the organization with a view to achieving its mission, vision and strategic objectives, thus achieving better results (Freitas, 2015).
A performance measurement system can be defined as a set of metrics, composed of several elements, which are used to quantify both the efficiency and effectiveness of actions (Neely, Gregory & Platts, 1995). Efficiency refers to the economic use of resources and is a prerequisite for measuring an organization's performance, both in financial and non-financial terms (Lindlbauer, Jonas & Vera, 2016). Effectiveness assesses the outcome of a process where customer expectations/needs are or are not met (Neely, Gregory & Platts, 1995).
According to Rahimi et al. (2018), the causal relationship between indicators, evaluation and performance of the health organization is complex and multidimensional. Therefore, in order to have a powerful evaluation system and be successful in improving hospital performance, instead of focusing on a single dimension, it must pay attention to all dimensions of performance. Among the various instruments for evaluating performance, the Tableau de Bord, Performance Prism and Balanced Scorecard stand out. In recent years, in the health area, most organizations have resorted to the BSC to evaluate their performance, which is recognized as an ideal instrument to achieve organizational transformations and evaluate performance at an organizational and individual level,
For Calhau (2009: 8) “this tool fulfills three essential purposes: it is an efficient measurement system, a strategic management model and a mode of communication”. Unlike traditional performance appraisal systems, which are insufficient to understand, predict and control the determinants of organizational success, the BSC bets on valuing intangible assets, of a qualitative nature, such as service quality, satisfaction level and rate. retention of customers and employees, competence and motivation of human resources, capacity for innovation and adaptation, among others (Santos, 2008). Russo (2015) and Silva (2012) also add that traditional management control systems, being based only on financial criteria, only transmit results from the past, which makes the information incompatible with the strategic objectives. Such systems can lead to intangible indicators being ignored, such as, for example, customer and supplier loyalty, product innovation, process quality, motivation and a higher level of technical knowledge of employees, problem response, etc. It is these indicators that increasingly assume a prominent role in the competitiveness of organizations.
The BSC appears for the first time in 1992, developed by Kaplan and Norton, at a time when there was a great discredit for financial measures, and it was necessary to find new methods to measure the performance of companies. After its implementation, the results were visible and it was the beginning of its success (Calhau, 2009; Kaplan & Norton, 2004).
Kaplan and Norton (1997: 25), refer that the BSC translates the “Mission and strategy into objectives and measures, organized through indicators to inform employees about current and future success vectors. By linking the company's desired results with the drivers of those results, executives hope to channel the energies, skills and specific knowledge of people across the company to achieve long-term goals.”
For the operationalization of the BSC, the use of indicators that are related to the strategic objectives of the organization is used (Madaleno, 2015). As mentioned, such indicators are not limited to evaluating only financial aspects, but also measuring and controlling non-financial indicators (Ojah, Malik & Ali, 2019; Tuan, 2020), which are considered fundamental for achieving the objectives of the organization (Prazeres, Lopes & Meira, 2013). The BSC, by focusing on non-financial indicators combined with financial ones, allows the analysis of all factors surrounding the organization that help in its process of adaptation and change in a world of economic globalization, where competition is increasing (Chavan, 2009).; Chow et al., 1998). In the same way, to recognize that non-financial measures are essential to achieve strategic objectives, is to accept that the complementarity between financial and non-financial indicators can be the pillar for an organization's success (Rompho, 2011; Kaplan & Norton, 1996). It also seeks to respond to the criticisms made to traditional strategic measurement systems, which only valued financial aspects, thus proving to be unsuitable for organizations where intellectual capital is prominent and where the ability to adapt to the demands of the surrounding environment is extremely important. for their success (Manica, 2009; Norreklit, 2003; Ahn, 2001; Kaplan & Norton, 1996). it is to accept that the complementarity between financial and non-financial indicators can be the pillar for an organization's success (Rompho, 2011; Kaplan & Norton, 1996). It also seeks to respond to the criticisms made to traditional strategic measurement systems, which only valued financial aspects, thus proving to be unsuitable for organizations where intellectual capital is prominent and where the ability to adapt to the demands of the surrounding environment is extremely important. for their success (Manica, 2009; Norreklit, 2003; Ahn, 2001; Kaplan & Norton, 1996). it is to accept that the complementarity between financial and non-financial indicators can be the pillar for an organization's success (Rompho, 2011; Kaplan & Norton, 1996). It also seeks to respond to the criticisms made to traditional strategic measurement systems, which only valued financial aspects, thus proving to be unsuitable for organizations where intellectual capital is prominent and where the ability to adapt to the demands of the surrounding environment is extremely important. for their success (Manica, 2009; Norreklit, 2003; Ahn, 2001; Kaplan & Norton, 1996).
According to Tuan (2020) and Martins (2015), by recognizing management weaknesses and inaccuracies, the BSC gives us an indication of what companies should measure to "balance" the financial perspective, providing us with feedback regarding the internal processes of the business and external results, with the aim of continuously improving strategic performance and results.
For Rua e Silva (2016) and Kaplan and Norton (1996), as the BSC is a management tool that aims to provide a global and integrated view of the organization's performance, it is important that there is a good communication of the strategy to the entire organization. and its relationship with the critical success factors, as these condition the organization's performance in the medium and long term. Thus, Alvarez et al. (2019) and Barboza (2011) refer that, in order to apply this tool, it is essential that there is an identification of objectives, indicators and goals by perspective, based on the mission and strategic vision.
According to a study carried out on the implementation of the strategy using the BSC, the following principles are identified as best practices with a view to success and achieving tangible benefits (Kaplan & Norton, 2000): mobilizing change through leadership executive; translate the strategy into operational terms; align the organization to the strategy; transform strategy into an everyday task for everyone, and transform strategy into an ongoing process. These authors (Kaplan & Norton, 2006) refer that, among these principles, the one that most facilitates the successful implementation of the strategy is organizational alignment.
It can thus be said that the BSC is a measurement instrument that allows clarifying and translating the organization's vision and strategy, of continuous learning, a communication tool made up of balanced performance indicators that facilitate the alignment between the operational part and the strategic objectives, which allows the monitoring and feedback of actions and practices by the leaders of organizations, and which facilitates the planning and allocation of resources (Tarigan & Bachtiar, 2019; Jordan, Neves & Rodrigues, 2011; Niven, 2002; Malina & Selto , 2001; Epstein & Manzoni, 1998; Kaplan & Norton, 1996). This tool considers the balance between short- and long-term objectives, financial and non-financial indicators, result indicators and inducing indicators, as well as between internal and external performance perspectives.external, thus leading to the achievement of the organization's strategy, increasing its efficiency and effectiveness (Santos, 2008; Kaplan & Norton, 1996).
The BSC uses a strategic map to materialize the organization's vision and strategy. This map includes the objectives, organized according to four different perspectives: financial, customers, internal processes and learning and growth (Freitas, 2015; Calhau, 2009; Kaplan & Norton, 1997). By considering these four perspectives, it allows managers to define which are the most important perspectives and objectives according to the organization's vision and strategy, always bearing in mind that none of them works in isolation or autonomously.
The implementation of the BSC implies: identifying the mission, vision, strategy and critical success factors, selecting indicators, evaluating, creating action plans and monitoring and managing (Kaplan & Norton, 2001). In addition to these processes, the implementation of the BSC implies the definition of a cause-effect relationship between perspectives, strategic objectives and indicators, so that the causal relationship that was assumed when defining the strategy is perceptible (Pinto, 2009). Kaplan and Norton (1996) stated that in order to have a link between the BSC, the organization's policies and strategies, three principles must be respected: interconnection with financial objectives, cause-effect relationships and performance indicators.
After being implemented, it is expected that: the strategy leads to the implementation of corrective actions, the strategic indicators are applied in the organization's processes, a systematized view of organizational performance is provided, a culture of learning and continuous improvement is developed, there is attribution of incentives and the strategy implemented is regularly tested (Kaplan & Norton, 2008).
Thus, the logic of this tool lies in its integrated operation, with the objectives and indicators establishing cause-effect relationships among themselves. In this sense, the objectives placed at the bottom are those that will lead to the achievement of the objectives placed at the top, that is, it is through the chain and the relationships established between them that the organization's strategy is achieved. This model is characterized, therefore, by its flexibility, it can be adjusted according to the organization, being subject to adaptations and refinements (Niven, 2005).
According to Collis and Rukstad (2008), Padoveze (2007), and Kaplan and Norton (1996, 1992), when considered a strategic management tool for management control, it allows informing stakeholders of strategic decisions and actions, and involves all stakeholders, thus facilitating the understanding of the vision and strategy, leading to alignment in all its aspects. When used properly, it plays an extremely important role in communicating organizational strategy to different employees, allowing feedback and linking long-term strategy with short-term actions, while creating strategic awareness among employees. It is in this context that the approach adopted by the BSC will help managers to define the organization's strategy.
Mission, Vision, Values and Strategy
In order to put the organization's strategy into practice and for it to move towards success, it is necessary that there is a clear definition of the organization's mission, vision, values and strategy, using financial and non-financial performance indicators (for example, Dias, 2014; Kaplan & Norton, 2001).
For all these reasons, it is important to clarify these four concepts.
- Mission: defines the organization's raison d'être, its uniqueness, its central purpose and what social function it performs (Hitt, Ireland & Hoskisson, 2009; Kaplan & Norton, 2004; Niven 2003; Tachizawa & Rezende, 2000). It must be clearly defined, it must make sense to the internal public and be understood by the external public, being specific to the organization in question (Dias, 2014). It can be seen, therefore, that it should serve as a guide for stakeholders. It is important to be considered in the implementation of the BSC, as it is the starting point for the strategy. Kaplan and Norton (2004) refer that the mission must define the direction of activities and which values guide these activities, as well as clearly assume the way to compete in the market and add value to customers. An effective mission is, for Pinto (2009),
achieve, involving not only the organization, but all stakeholders. According to Serrano (2017), the definition of the mission assumes greater importance when dealing with public or non-profit organizations. For this author, in private sector organizations, mission is not a central issue, whereas in public and social sector organizations, mission assumes an extremely important role, as they are totally mission-oriented.
- Vision: is a clear, precise and comprehensive statement that reflects the organization's intentions and aspirations, that is, what the organization wants to achieve in the future (Hitt, Ireland & Hoskisson, 2009; Kaplan & Norton, 2004; Niven, 2003; Tachizawa & Rezende, 2000), with the use of resources, products and services that it has or will have (Pinto, 2009). It must be market-oriented, convey how it wants to be perceived by the outside and reflect its values and aspirations (Senge, 2010; Hitt, Ireland & Hoskisson, 2009; Kaplan & Norton, 2004), thus presenting itself as essential for any type of business. organization: public, private, public-private or non-profit (Pinto, 2009). The mission and vision, are the pillars on which top management will rely to start the process of building and implementing the strategy (Serrano, 2017), and the vision should only be formulated after defining the organization’s mission and values (Pinto, 2009). The vision is thus seen as the starting point for the definition of priorities and as one of the fundamental pillars for the construction of programs and strategic maps that will serve as a guiding guide for the organization and that will help it to achieve success (Serrano, 2017).).
- Values: they are principles that guide an organization, portray its beliefs and define the perception of what is important, right and wrong, fair and unfair (Sousa, 2016; Senge, 2010; Niven, 2003) and are interconnected with the mission, allowing them to have a logical continuity (Kaplan & Norton, 2008; Collins & Porras, 1996). According to Sousa (2016) and Werner and Xu (2012), values are the guiding principles of an organization, thus defining how the organization should act in accordance with its mission, while accompanying the organization to achieve your vision.
- Strategy: set of hypotheses, decisions and actions that represent the way forward to reach the desirable future, described in the vision and that allow adding value to stakeholders (Dias, 2014; Kallás & Coutinho, 2005; Kaplan & Norton, 1997). Alves (2016) states that the definition of strategy assumes a special prominence in the BSC and its execution is one of the most difficult tasks of the leaders, being for it is important that there is a clarification of the strategic orientation before the implementation of this tool.
For Pinto (2009), the mission, vision, and values highlight the “why” and “who”, whereas the strategy tells us “How”. After defining and clarifying these concepts, organizations are in a position to prepare and implement the BSC (Dias, 2014).
Objectives, Indicators, Goals and Initiatives
The BSC cannot be seen only as a measurement system, but as a management system (Gallon et al., 2008). As such, it allows organizations to measure and qualify their vision and strategy and translate it into action. As mentioned above, this tool is based on four perspectives (Financial, Customers, Internal Processes and Learning and Growth), each of which has its own strategic objectives. In turn, these objectives will allow the organization to achieve its mission and vision (Kaplan & Norton, 1997).
According to Norreklit (2000) and Mooraj, Oyon and Hostettler (1999), for each of the strategic objectives, indicators are defined, and the choice of these must be made taking into account some criteria, namely: link to the strategy, accessibility and relevance. The same authors state that, in these indicators, cause-effect relationships are a central aspect of the BSC.
When using the BSC, managers have at their disposal four management processes that, alone or together, help to combine long-term goals with short-term goals, namely vision translation, communication and connection, planning of business and feedback and learning (Kaplan & Norton, 1996). These management processes provide the necessary steps to achieve financial success in future terms, based on non-financial indicators (Kaplan & Norton, 1996; Malina & Selto, 2001). For these authors, the achievement of short-term financial goals should not be considered satisfactory when it is expected that long-term measures are not being properly implemented. It is important that managers who use the BSC do not rely only on short-term financial measures. term, as performance indicators, as they give us information about how well the past has worked, but little information about what the future might look like.
The use of this tool only makes sense when the process begins with top management, allowing it to translate the organization's strategy into strategic objectives. For Kallás and Ribeiro (2008), these objectives should be organized in a diagram so that cause-effect relationships can be identified in different perspectives. For Alves (2016), when translating the vision and strategy, the BSC facilitates the definition of actions to be taken to define the strategic map, as well as helping to create consensus among managers of the organization's vision and strategy. According to Padoveze (2007), if there is communication and association between objectives and strategic measures, managers can ensure that all employees understand the long-term strategy, and that everyone's objectives are aligned.
The choice of indicators is an extremely important task, as the wrong choice can lead to wasted investments. After choosing these, they should be reviewed between top management and middle management, which facilitates the evaluation of strategies according to new information that emerges about competitors, customers, markets, technologies and suppliers (Kaplan & Norton, 2004, 1996).
Some authors (Bourguignon, Malleret & Norreklit, 2004; Ittner & Larcker, 1998) argue that, being a flexible system, the BSC facilitates the definition of both the number of indicators and the weight that each one should assume, which can be adjusted by the organization itself. In a study carried out by Inamdar, Kaplan and Bower (2002), in nine health organizations, these authors define that each perspective should ideally have the following weight: clients 33%; internal processes 27%; financial 23%; learning and growth 17%, however, it will be up to each organization to define the weight to be attributed according to its reality and strategy.
For the implementation of the BSC to be successful, as important as the definition of objectives and indicators, is the definition of goals and initiatives (Serrano, 2017):
- Goals: must be clear and concise, stipulated for each of the perspectives and must state what the organization hopes to achieve (Alves, 2016). Your choice should fall on the aspects that lead to an improvement in the organization's performance, as well as the aspects that help it to improve its range of skills (Alves, 2016). According to the same author, each objective has associated goals, and should facilitate the achievement of the organization's strategy. If the objective does not prove useful in consolidating the organization's strategy, it must be eliminated or the strategy must be changed.
- Indicators: help to assess the success of each objective, that is, they facilitate the assessment of the degree of achievement of each objective (Alves, 2016). Indicators should be of two types, lagging indicators and leading indicators. The BSC is stronger the better the mix of indicators used in each of the strategic areas (Norreklit, 2000; Epstein & Manzoni, 1998).
- goals: they define the level of performance or the rate of improvement intended for each of the defined indicators (Alves, 2016) and must be adapted to each of the strategic objectives, based on real estimates, the time needed to produce benefits and the resources available (Caldeira, 2010; Kaplan & Norton, 2009). Its definition must be cautious, so that it can be achieved, as the definition of unrealistic goals can lead to demotivation of professionals (Caldeira, 2010; Kaplan & Norton 2004).
- Initiatives: they are seen as action plans, where the actions that will contribute to achieving established goals are defined (Werner & Xu, 2012). Kaplan and Norton (2009) state that initiatives are the force that drives the organization to fight inertia and resistance to change.
Cause-Effect Relationships and Strategic Map
For Kaplan and Norton (1996), within the BSC, strategy is nothing more than a set of hypotheses about causes and effects, that is, for every action there will be a reaction, with an impact on the organization's business and that will influence the implementation of your strategy(ies). To implement the BSC, it is necessary to establish cause-effect relationships between the four perspectives, between outcome measures and between performance vectors. Pinto (2009) also corroborates this idea. By stating that this tool's fundamental principle is the definition and verification of cause-effect relationships between perspectives, objectives, goals and indicators.
When developing the BSC in for-profit organizations, the focus is on financial objectives, however, in public sector organizations (non-profit) this tool begins with the definition of the organization's mission (Pinto, 2009). This author also states that cause-effect relationships go through the formulation of simple questions that will lead to the definition of objectives and strategies, which in turn will contribute to the correct identification of which competencies and infrastructures the organization needs. bet so that it can support internal processes and, therefore, satisfy customers. Cause-effect relationships allow us to assess the extent to which the BSC portrays the organization's strategy,
For Alvarez et al., (2019) the strategic map is developed by analyzing the cause-effect relationships between the different objectives. It is a graphic relationship, the way in which the objectives are related in one perspective and also the relationship they establish between the other perspectives, constituting what is called alignment of objectives. This alignment makes it possible to clarify that the achievement of some goals leads to the achievement of others (Alvarez et al., 2019).
The strategic map, when adjusted to the organization's strategy, indicates the path to transform intangible assets into tangible assets, that is, it describes how the former lead to performance improvements in internal processes, which in turn translate into in creating value for customers, shareholders and the community. This strategic map is constructed by establishing a vertical vector through the four perspectives and promotes communication within the organization, while constituting a strategic feedback system (Sousa, 2016; Marçal, 2008; Norreklit, 2003; Ahn, 2001; Kaplan & Norton, 2000, 1996; Mooraj, Oyon & Hostettler,
1999).
Cause-effect relationships are used to communicate how employees can contribute to the achievement of established goals, thus implying that there is a clear link with the implementation of the strategy. Cause-effect relationships also facilitate understanding regarding the allocation of resources and capabilities (Caudle, 2008; Ahn, 2001). In turn, the strategic map creates the foundation for the implementation of strategies quickly and effectively (Kaplan & Norton, 2001), and can be seen as the structure that is used to communicate the history of the strategy to the target audience (Alves, 2016). And helping organizations to see their strategies in a coherent, integrated and systematic way (Quintella, 2004).
This framework clarifies the organization's strategy and values, making it easier for employees to understand how their activities can contribute to the organization's success. This understanding on the part of everyone is essential for the implementation of the strategy to be successful (Barbosa & Perez, 2016; Madaleno, 2015; Maia, Oliveira & Martins, 2008; Atkinson, 2006; Niven, 2005). Smith (2007) states that strategic maps are a great means of communication, as they indicate which are the most critical processes and what positive impact would be obtained in financial terms and on customer satisfaction if improvements were made to them.
For Sousa and Rodrigues (2002), the strategic map must translate the organization's strategy into operational terms, as well as being a facilitating element for the evaluation of performance.
According to Kaplan and Norton (2001), it is in the strategic map that the essential objectives are explained, as well as the links that define the organization's strategy. Among these, the following stand out:
-Objectives to increase shareholder value;
- Market share, acquisition and retention of target customers;
- Value proposition that contributes to a higher profit margin;
- Innovation and excellence in products, services and processes;
- Necessary investments in human and technological resources to generate and maintain growth.
The strategy map is built from top to bottom, improves clarity and focus, as well as represents the missing link between strategy formulation and execution (Kaplan & Norton, 2004). According to Penha and Costa (2012), the strategic map includes four stages: definition of the strategy; identification of essential perspectives for the development of the strategy; definition of the strategic objectives to be achieved in each perspective, and finally representation of the cause-and-effect relationship between the perspectives/objectives.
It is up to each organization to customize its strategy map according to its specific objectives. Kaplan and Norton (2004) argue that organizations can develop and communicate their strategies using approximately two to three dozen objectives, provided that the strategic map is well prepared and clearly identifies the cause-and-effect relationships between them. they.
In 1996, the same authors stated that the BSC is based on the global vision of the organizations' strategy, supported by four perspectives, and that for each of them objectives and indicators are defined that need to work in an integrated and balanced way. For Norreklit (2000), it is these relationships that distinguish the BSC from other strategic management systems. A failure to achieve the objectives of one perspective will lead to efficiency drops in the other perspectives, thus causing an imbalance in the BSC, and negatively affecting the implementation of the strategy, as well as the fulfilment of the organization's mission and vision. That said, it is clear that the strategic maps are the basis for the construction of the BSC.
prospects
The BSC is based on the organization's strategic vision and is supported by four perspectives: financial, customers, processes and learning. For each of these perspectives, objectives and indicators are stipulated, which act in an integrated manner and establish, among the four perspectives, cause-effect relationships (Serrano, 2017; Sousa, 2016; Alves, 2016; Dias, 2014; Kaplan & Norton, 1996).
It is thus clear that this tool does not only include financial indicators, but also non-financial indicators, and it is with the use of these indicators of a non-financial nature that manages to achieve its objective of measuring the performance of the organization (Dias, 2014; Corral & Urieta, 2001). Pinto (2009) draws attention to the fact that this tool makes it possible to establish a link between short-term objectives and the long-term strategy, which is one of the aspects that puts him at the forefront in terms of management systems. performance measurement.
Kaplan and Norton (1997) state that short and long-term objectives, results and performance vectors should be defined having as a reference point the performance measurement of the four perspectives and, given that the BSC is a tool for systemic nature, these objectives must be clearly and balanced, which is the level of integration of the organization's strategy, thus avoiding that the focus is only on one of the perspectives.
It only makes sense to think about these perspectives, when the organization's vision and strategy are placed at the center of them. Pinto (2009) complements this theory and states that vision and strategy are not only the starting point, but also the light that should direct the way, with a view to achieving the organization's long-term goals.
For each of the perspectives, there are defined questions, which indicate what should be measured in each of them (Kaplan & Norton, 1996, 1992):
- Financial: To be financially successful, how should we present ourselves to shareholders?
- Clients: To achieve our vision, how should we present ourselves to our clients?
- Internal Processes: To satisfy customers and shareholders, what processes must we excel at?
- Learning and Growth: To achieve our vision, will we continually be able to change and improve?
Financial Perspective: for a long time, financial indicators were considered the only way to measure an organization's performance. The BSC seeks to go further and consider the interaction between this perspective and the others, thus, allowing managers to identify in which perspectives they should act at a given moment to achieve financial goals.
According to Serrano (2017), this perspective represents the most traditional way of evaluating results, and it is the one that is most used to evaluate the results of organizational performance, it is closely related to the interests of shareholders, which are mainly of financial character.
The financial perspective considers the balance between short and long-term objectives, and for many organizations it occupies the top of the strategic map (Kaplan & Norton, 2001, 1993, 1992), especially in private organizations. In the case of public organizations, this can appear either at the top of the strategic map next to the customers' perspective, or in second place, immediately before the customers' perspective.
For Kaplan and Norton (1997), financial objectives and indicators play a dual role. If, on the one hand, they define the expected financial performance of the strategy, on the other hand, they serve as a reference for the objectives and indicators of all other perspectives.
According to Ferreira (2012), the isolated use of economic and financial indicators can harm the creation of long-term value, as it tends to focus attention on short-term results. The importance of all the objectives and indicators of the remaining perspectives being linked to the objectives of this perspective is highlighted, orienting towards long-term goals, while ensuring that all strategies and initiatives are directed towards achieving the financial objectives. Financial indicators are different depending on the life cycle of the organization, the most used being the rate of return, cost reduction rate, growth and sales volume, percentage of investment, return on investment, net income for the period, among others (Zhou et al., 2020; Jordan, Neves & Rodrigues, 2011; Kaplan & Norton, 2001; Lipe & Palter, 2000).
When it comes to public and non-profit hospitals, Dias (2014) states that the objective is not the return of shareholders, as such, the fundamental thing is for the organization to have financial resources, to know how to monetize them and transform them into benefits for their employees. customers/users. Serrano (2017) reinforces the previous idea and adds that, in the BSC, financial indicators are of great importance in this type of organizations, as the human, material and financial resources are essential for the proper functioning of organizations.
Customers Perspective: many organizations stipulate their mission with customer focus. By assuming this position, the customer perspective becomes the priority of top managers (Dias, 2014; Pinto, 2009; Caudle, 2008; Mooraj, Oyon & Hostettler, 1999; Kaplan & Norton, 1996, 1992). Kaplan and Norton (1996) mention that this concern is important not only in the private sector, but also in the public sector and non-profit organizations.
This perspective translates the mission and strategy into customer-oriented objectives. As such, it is necessary to identify the customer segments and markets where they wish to compete, and that these objectives are communicated to the entire organization (Alves, 2016; Martins, 2015; Russo, 2015; Dias, 2014; Caldeira, 2010; Kaplan & Norton, 1996). Kaplan and Norton (1997) state that when organizations do not understand customer needs, they end up losing them to others where there is greater appreciation of customer needs/preferences.
According to Santos (2008), this perspective is concerned with the way the organization is seen by its customers and with the way it would like to be seen by them. As such, it is concerned with creating value for the customer so that it becomes loyal (Russo, 2015), allowing the alignment of its results indicators related to customers (satisfaction, loyalty, retention, capture) with specific market segments. (Serrano, 2017; Banza, 2013). It is thus understood the importance of finding key indicators adjusted to the organization's strategy, and that help it to understand both customers and their needs. As it is related to customer satisfaction, it is important that all elements of the organization make the relationship and satisfaction of their needs a priority.
Kaplan and Norton (1996, 2000) state that the focus of any strategy is the value proposition for the customer, which is achieved through the combination of a set of aspects, namely products and services, relationship with customers and external image. These authors point out as value propositions: operational excellence; customer intimacy; and product leadership.
Internal Processes Perspective: considers the measures/efforts that the organization makes to improve existing operational processes, in order to meet the expectations of customers, shareholders, as well as achieving the organization's financial objectives. In general, this perspective seeks to achieve what is the quality desired by the customer, without ever forgetting the strategic objectives of the organization (Russo, 2015; Dias, 2014; Werner & Xu, 2012; Caldeira, 2010; Manica, 2009; Matos & Ramos, 2009; Pinto, 2009; Kaplan & Norton, 1996, 1992).
For Martunis et al. (2020), the perspective of internal processes refers to the organization's ability to perform work activities as planned.
Serrano (2017) and Kaplan and Norton (1996) tell us that core processes are those that have the greatest impact on customer satisfaction and that organizations should decide which processes and competencies they should achieve excellence in, as well as how to specify the objectives and indicators for each one of them, in order to achieve competitive advantage. In this way, excellence is achieved through processes, actions and decisions that occur throughout the organization, with innovation processes assuming a leading role towards good financial performance. It is therefore essential that these organizations identify which are the key processes for creating value, in order to improve them.
The perspective of internal processes, with the aim of achieving the strategic objectives of the organization, seeks to find a solution to the following challenges: growth; produce value; deliver the proposed value to customers; value assets; improve processes and reduce production component costs (Serrano, 2017; Santos, 2008). According to Alves (2016) and Dias (2014), cycle time, costs, quality, productivity and innovation are used as main indicators.
Managers must stipulate a value chain of internal processes that must focus on three major areas: innovation, operations and after-sales (Kaplan & Norton, 1997). By carrying out measurements from this perspective, managers can better understand and know how their business, products and services work. services, according to the customer's requirements. The better the managers know the process, the better the adequacy of the strategies.
Learning and Growth Perspective: from this perspective, the main sources are: people, systems and procedures (Russo, 2015; Kaplan & Norton, 1996). The BSC emphasizes the importance of investing in learning, always with an eye on the future, and considering that in order to face technological changes it is necessary to invest in continuous learning (Massingham, Massingham & Dumay, 2018; Martins, 2015; Dias, 2014) so that the organization can grow and develop in the medium/long term (Alves, 2016). For Martunis et al. (2020), this perspective represents the organization's effort to improve the quality of the performance of its human resources.
It is in this perspective that the main competencies and skills, technologies, values and culture necessary, which support the organization's strategy and where priorities are defined that help in the construction of an organizational environment that supports innovation, growth and change (Dias, 2014; Kaplan & Norton, 2004, 2001, 1996).
According to Kaplan and Norton (2004, 1996), this perspective considers a series of intangible values, such as human capital, information capital and organizational capital, which establish cause-effect relationships with the other perspectives, thus leading to success. end obtained from the top perspective – customer perspective, in the case of the public sector. For this to happen, it is necessary to invest in the retraining of employees, in the development of technologies, and in the alignment of organizational procedures and routines, to fill the gaps between the necessary and existing capabilities (Kaplan & Norton, 2004; Mooraj)., Oyon & Hostettler, 1999).
With regard to the learning and growth perspective, Kaplan and Norton (1997) refer to the needs of the organization, that is, what it needs to develop in order to grow in the long term. As such, this perspective uses indicators such as professional satisfaction, professional training and length of service.
This perspective stands out from the others, because its objectives are defined after identifying the needs in the other perspectives, and thus the one that will be the inducer of the results achieved in the other perspectives, given the interdependence relationship between them (Norreklit, 2003).; Santos, 2008).
For Pinto (2009), this perspective underlines which factors, in terms of resources and infrastructure, in which the organization should invest in order to be competitive, being increasingly important, as it is concerned not only with maintenance, but also with the long-term sustainability of the organization (Alves, 2016). It is essential for the success of the organization that human resources have adequate training, are motivated, involved and aligned, as only then will they lead to success (Kaplan & Norton, 1996).
The BSC gives the manager a view of the business from these four perspectives, in a quantifiable and objective way, avoiding excess information (Dias, 2014; Kanji & Sá', 2002). According to Serrano (2017), the four perspectives are interconnected in a cause-effect relationship, and the vision and the strategy simultaneously represent the pillars and the starting point for the construction and development of the BSC.
Although the literature highlights the importance of the four perspectives, it is important to understand the order stipulated for the different perspectives, depending on the scope of the organization (public, private, public-private and social).
BSC in the Health Sector
The health sector has an enormous impact in terms of economic significance, representing one of the biggest consumers of public resources, at the same time that it is subject to enormous criticism from citizens, given that its function is to prevent disease and treat their health. However, it must always be kept in mind that we live with a scarcity of resources and with virtually unlimited needs, so careful decision-making is extremely important when it comes to the use of resources. In this context, the use of the BSC represents a valuable tool in the management of organizations operating in the health sector, given its characteristics of complexity and high degree of uncertainty (Inamdar, Kaplan & Bower, (2002). Zelman, Pink and Matthias (2003) also state that the use of the BSC is extremely important for the hospital environment, as it allows establishing a link between practice, quality, results, value and costs. Other authors also argue that by using this tool it is easier to achieve alignment between organizational strategy, action plans and performance management, as there will be a union between vision, values and day-to-day operations (Carvalho, Dias & Prochnik, 2005).
The use of the BSC in healthcare for the first time was Griffith's responsibility in 1994. Since then, its use in this field has gained prominence. According to Inamdar, Kaplan and Bower (2002), the use of the BSC in this area represents a valuable tool in the management of organizations operating in the health sector, given its characteristics of complexity and high degree of uncertainty.
Silva and Prochnik (2005) and Baraldi (2002) point out as the main aspects that underlie the use of this tool in health organizations, the following:
- Difficulty linking indicators to strategic planning;
- Problematic information systems;
- Lack of formal measurement systems;
- Deficit of coordination between health professionals and administrators;
- Wide range of consumer needs;
- Greater competitiveness.
Several factors boosted the use of the BSC in hospital institutions, including strong economic and financial pressures related to rising health care costs, political pressures to contain public expenditure, and technological advances. All these aspects led managers to implement management tools, which until then were developed in the private sector, but with proven evidence that they led to increased performance when associated with an efficient management of resources (Quesado & Macedo, 2010). As a result of growing budgetary constraints in this area, the introduction of management systems becomes increasingly important, as it facilitates monitoring, evaluation, and decision-making support with a view to improving the performance of organizations. As management systems are traditionally applied in the private context, Tarigan and Bachtiar (2019) and Niven (2005) report that more and more public hospitals use the BSC, and have managed to obtain attractive results, as it allows them to find ways to articulate your strategies, and quantify your success with regard to achieving goals.
Santos (2008) mentions that the successful implementation of the model is laborious and must come from the top management, which is the one who prepares the policies and is responsible for their execution. In the health area, the use of this tool must include the use of indicators of structure, processes, results and those related to the external environment or environment. Through this set of indicators, it is possible to obtain information with the objective of achieving efficiency and effectiveness (Bittar, 2001). Kaplan and Norton (2001) refer that to implement the BSC in health it is necessary to: mobilize change through executive leadership, translate the strategy into operational terms, align the organization with the strategy, transform the strategy into a task for all, and convert strategy in an ongoing process.
Although the strategy is the focal point of the BSC, public organizations find it difficult to outline it clearly and concisely. For Kaplan and Norton (2001), this must encompass the organization's mission, it must be visible to everyone, allowing them to understand its purpose.
Although it was created to be implemented in private institutions, some changes are necessary when implementing it in the public sector. Several authors state that, contrary to the private sector, public organizations do not present the financial perspective as a final objective, and as such, the perspective placed at the top is the Customer perspective (Tarigan & Bachtiar, 2019; Kaplan, 2010; Caldeira, 2010; Matos & Ramos, 2009; Pinto, 2009; Kaplan & Norton, 1997; Niven, 2005). In public organizations, financial objectives will be seen as a facilitating or restrictive element towards customer satisfaction (Alves, 2016; Niven, 2005).
- Mission – appears at the top of the BSC and works as a fifth perspective. In public hospitals, the Mission should be more comprehensive and towards which the objectives, goals and initiatives stipulated for the other perspectives must converge (Dias, 2014; Tarigan and Bachtiar, 2019).
- Customer Perspective – assumes the main role, right after the mission.
- Financial Perspective – it is no longer at the top and comes before the customers, meaning that it is a resource and, at the same time, a constraint associated with the existing budgetary rules in the sector.
The adoption of the BSC in many world health organizations has led them to success, as it is used as a tool that helps in the control of management and allows a better assessment of their efficiency and effectiveness (Ribeiro, 2008). Thus, this tool, when applied to health, does not represent just a simple instrument of measurement and control, but an evolution in terms of strategic management. The successful implementation of the BSC has been considered an asset at the level of health organizations, as it helps to improve the performance of the hospital, as well as the national health system (Ba-Abaad, 2009). Zelman, Pink and Matthias (2003) also state that the use of the BSC is extremely important for the hospital environment, as it allows establishing a link between practice, quality, results, value and costs.
There are several successful cases reported, of which the following stand out:
- According to data published at Duke Children's Hospital, in the United States, the BSC began to be used in 1996, and in 2000, user satisfaction had already improved by 18%, professional satisfaction by 45%, the average patient stay went from 7, 9 to 6.1 days, the readmission rate from 7 to 3%, and the cost per patient decreased by about
5,000 dollars (Meliones, 2000). These changes made the hospital, which was in a situation of loss, start to make a profit (Meliones, 2000).
- Another example, which demonstrates the good results obtained with the application of the BSC, is the case of a Thai hospital that applied this tool in the emergency department and found that: the levels of satisfaction of its employees increased; there were improvements in the performance time of the laboratories, which in turn led to improvements in patient care, in turn increasing service satisfaction; in operational terms positive results were obtained; and that investment in training, in the areas of customer service and communication, contributed to increased user satisfaction (Matos & Ramos, 2009).
- Hospital Nove de Julho, in São Paulo, one of the first to implement the BSC in Brazil, also recorded positive results after using this tool, having already received awards for quality and customer service (Alves, 2016).
- At Mackay Memorial Hospital in Taiwan, the BSC was implemented in 2001, with the aim of increasing the hospital's competitive advantage. According to Chang et al. (2008), the implementation of this tool contributed to learning and continuous improvement, allowing the administration to improve the view on the industry, as well as on the competitive position of the hospital. With the results achieved after the implementation, this hospital was able to reinforce its competitive advantage (Chang et al., 2008).
In Portugal, although the importance of performance evaluation is recognized, it is still at an embryonic stage (Pinto, 2009) and the dissemination and study of the BSC is not as advanced as in other European and North American countries (Russo, 2009). 2015). However, Calhau (2009) and Matos (2006), refer that, when implemented, there is a great acceptance by health professionals in the implementation of this tool in Portuguese hospitals, representing the BSC a means to improve the efficiency and effectiveness of same. Management based on the BSC can lead to a more efficient use of public resources, the satisfaction of social needs and the balance between the State's obligations towards taxpayers (Russo, 2015). Serrano (2017), refers that also in Portugal there have been cases of success with the implementation of the BSC in the health sector. For this author, success stories should be used and replicated in different health organizations, provided they are adapted accordingly. By assuming this policy, we would move towards a greater approximation of the different professional classes in the achievement of common goals, improvement in organizational communication, improvement of the quality of the service provided to the user and in the creation of value for them.
Benefits and Difficulties in Applying the BSC Applied to Health Organizations
Reviewing the existing literature on this tool (e.g., Oyewo, Oyedokun & Azuh, 2019; Cruz, Geada & Silva, 2012; Silva & Nunes, 2007; Matos, 2006; Walker & Dunn, 2006; Pereira, 2005; Inamdar, Kaplan & Bower, 2002; Sanchez, Stadnick & Erdmann, 2002) the following benefits achieved with the use of the BSC by health organizations are pointed out:
- It helps to clarify and reach consensus on the strategy;
- Improves the alignment of all professionals around a user-centered strategy, making the strategy a continuous process and a function of all;
- Clarifies the allocation of responsibilities for hospital performance;
- Contributes to the simplification, monitoring and evaluation of the implementation of strategic objectives;
- Increases the credibility of management bodies;
- Facilitates the decision-making process;
- Establishes the essential principles and processes for the implementation of the strategy;
- Optimizes resource allocation;
- Allows you to have a financial and non-financial view of the organization;
- Increases employee motivation;
- Contributes to staff development and retention;
- It allows the development of an information measurement and reporting system, which helps in evaluating the progress and success of the strategy;
- Allows the creation of a communication and collaboration mechanism between professionals;
- Encourages continuous improvement and learning;
- It favors the development of new products;
- It makes management more efficient and systematic;
- Contributes to the improvement of medical care;
- Improves internal processes;
- Allows the maintenance of financial stability;
- It contributes to the reduction of costs, without this having an impact on the quality of the service provided.
Despite all the listed benefits associated with using the BSC, it is also possible that its implementation will not be successful, which may be due to the lack of commitment by top management, little involvement by professionals, too long development processes, recourse to inexperienced consultants and implementation for remuneration purposes (Kaplan & Norton, 2000). Given that these difficulties are felt in other sectors, it is not expected that the situation will be different in the health sector (Carvalho, Dias & Prochnik, 2005).
The problems, described in the literature (eg García, 2007; Silva & Nunes, 2007; Matos, 2006; Carvalho, Dias & Prochnik, 2005; Cruz, 2005; Silva & Prochnik, 2005; Zelman, Pink & Matthias, 2003) associated with the use of the BSC in health can be divided between internal and external, of which some stand out:
- Conflict of interest between administration and clinicians;
- Deficit in the dissemination of performance evaluation methods;
- Ignorance of the BSC;
- Lack of commitment from top management;
- Inexperience in the use/monitoring and evaluation of indicators;
- Difficulty justifying the money invested;
- Difficulty in grouping and selecting the large number of indicators from different sources of information;
- Failure to select performance evaluation indicators.
Although it has limitations, it is important to emphasize that the BSC proves to be a great tool to be used in the public sector. In order to contribute to the improvement of the performance of health organizations, this tool needs, however, to be implemented in a thoughtful and organized way. The success of its implementation depends on effective guidance, monitoring and evaluation (El-Jardali, Saleh & Jamal, 2011).
A recent literature review (Aryani & Setiawan, 2020) led to three fundamental conclusions: that the BSC is widely used, contributing both to the improvement of organizational performance and to the development of the organization's strategy; the Balanced Scorecard implementation status reveals a high level of success, and a low level of failure; although it has limitations, the benefits obtained with its implementation outweigh the limitations and reinforces the view that the BSC is a valid tool to consider in terms of performance management.
However, there are many studies that highlight the non-generalization of its use, the result of a set of barriers that can prevent or limit the chances of success (Quesado, Guzmán and Rodrigues, 2018). For this reason, several authors (Tarigan & Bachtiar, 2019; Gao et al., 2018; Quesado, Guzmán & Rodrigues, 2018; Madsen & Stenheim, 2015; Lueg, 2015; Hoque, 2014; Lueg & Julner, 2014; Lin et al. al., 2013; Lueg & Silva, 2013), refer to the need to develop more studies in this area of knowledge.
The literature review carried out shows that empirical research on this topic is still not enough, and the results obtained are often inconsistent. Although there are already some literature reviews on this topic, they focus essentially on the success or failure in the implementation of the BSC. It is therefore essential to review the literature that, in a systematic way, can clarify and standardize the process of implementing the BSC in the health sector in its different contexts (ie public, private, public-private and social sectors). It is here that this research intends to make its contribution, by identifying and systematizing which indicators are most used worldwide, in each of the perspectives, thus facilitating the most appropriate choice for each reality.
It is in this sense that it seems important to us to answer some questions, namely: What are the characteristics of the publications that report the application of the BSC in hospitals?; What is the motivation for using the BSC?; What are the characteristics of the hospitals where the BSC was implemented?; Who are the actors in the process of designing and implementing the BSC?; What are the perspectives and performance indicators most frequently used in the application of the BSC in hospitals?; What are the facilitating factors in design and implementation?; What are the results obtained with the implementation of the BSC?; What are the difficulties and/or limitations to the implementation of the BSC?; What opportunities are there for future investigations in this area?
Using a literature review as a methodology, we intend to obtain the answer to these questions, present an overview of the existing literature on the application of the BSC in Hospital Units, and summarize the main indicators used in the application of this tool, as well as the main results obtained with its implementation and possible gaps in this area of knowledge. The achievement of these objectives may facilitate the adoption and development of this tool in health institutions, by presenting a summary of what has been studied worldwide.
Methodology
In this chapter, the methodology used in this investigation will be discussed, in order to obtain theoretical support, regarding the research strategy and the procedures adopted for its realization.
In order to carry out this investigation, we chose to carry out a systematic literature review, as it seems to us to be the most appropriate methodology for achieving the research objective and, at the same time, responding to the questions listed above. In addition, this methodology allows the collection of data on the subject under study, through research, selection and synthesis of literature, that is, it will allow us to search for articles that focus on the application of the BSC in a hospital context, draw conclusions about the state of the art and identify aspects that require special attention.
Systematic Review of Literature
The literature review is crucial in any research, it is essential in academic research and very useful for the analysis of studies on emerging topics (Xiao & Watson, 2017; Jabbour, 2013). According to Xiao and Watson (2017) the advancement of knowledge must be built, based on the work already carried out, because using these it is possible to understand the breadth and depth of the existing work, as well as identify gaps to be explored. Pare et al. (2015) reinforce this assumption and state that the literature review also allows assessing the validity and quality of existing work, revealing weaknesses, inconsistencies and contradictions. According to Xiao and Watson (2017), literature review is as valid and reliable as empirical investigations.
For Petticrew and Roberts (2006:2), “systematic literature reviews are a method of making sense of large bodies of information, and a means of contributing to the answers to questions about what works and what does not – and many other types of question too”. Nicholson, McCrillis and Williams (2017) state that when summarizing the results of original studies on a given topic, systematic reviews of the literature are considered as high-quality evidence, they are increasingly assumed as the most important and there has been a growing increase in the use of systematic review as a research methodology.
The main objective of this research methodology is to provide a critical analysis and a synthesis of the main evidence related to the subject under study (Sampaio & Mancini, 2006).
The systematic review of the literature is based on scientific methods, which will act as a limiting factor for possible errors, by identifying, evaluating and synthesizing all relevant studies in the study area.(Petticrew & Roberts, 2008). The identification of all studies is, however, one of the main difficulties of a systematic literature review.
Higgins and Green (2011), editors of the Cochrane Collaboration, state that a systematic review of the literature has as main characteristics: a set of clear and precise objectives with previously defined eligibility criteria for the studies; an explicit and reproducible methodology; a systematic investigation that attempts to identify all studies that meet the eligibility criteria; an assessment of the validity of the results of the studies included in the sample and a systematic and summarized presentation of the characteristics and results of the studies included in the sample.
According to Donato and Donato (2019), there are four fundamental criteria for carrying out a systematic literature review:
- be exhaustive: including all relevant literature in the field;
- follow a rigorous methodology – by defining the research question, designing a protocol, searching the literature, collecting, sorting and analyzing the literature. It is important that this entire process is documented;
- have a rigorous and high-sensitivity search strategy to find all potentially relevant articles, and this search should be done in different databases and other resources;
- involve at least two people in article screening and data extraction.
According to the literature, there are several steps involved in carrying out a systematic literature review, namely:
- Formulate the research question(s): before starting the investigation, it is necessary to define in a clear, precise and objective way which (which) the investigation question(s) are. It is important that each question is neither too restrictive (as it can make it difficult to select studies, making generalization limiting), nor too comprehensive (as it will compromise the applicability of the conclusions to the population) (Donato & Donato, 2019; Wright et al., 2007).
- Produce an investigation protocol and register it: after defining the research question(s), it is important to create a research protocol, which includes the question(s) to be investigated, the methods that will be used in the review and the objectives to be achieved. It will also be important that the protocol also includes the search terms, databases and other resources to be consulted, in order to minimize the bias of the conclusions. It is also important that this protocol includes the definition of inclusion and exclusion criteria, indicates how the selection of studies will be carried out, and that the strategy for data synthesis is specified. The realization of this protocol is crucial to help ensure consistency, transparency and integrity (Donato & Donato, 2019; Petrou, Kwon & Madan, 2018).
- Define inclusion and exclusion criteria: this is where the authors explicitly define the criteria to use to select the studies they will include and which studies they will exclude (Donato & Donato, 2019).
- Develop a research strategy and search the literature: Finding the relevant studies is a key component of conducting a systematic literature review. For this methodology to be successful, exhaustive research is essential, so that all relevant studies on the subject under study can be identified. As such, the research strategy must be rigorously developed and have high sensitivity, thus ensuring that all studies with potential for the investigation being carried out are found (Donato & Donato, 2019; Uttley & Montgomery)., 2017).
- Selection of studies: at this stage it is necessary to examine titles and abstracts to remove obviously irrelevant documents; obtain the full texts of potentially relevant articles; examine whether the studies meet the eligibility criteria, and in case of doubt, contact the authors to clarify the eligibility of the study; decide on inclusion of studies before proceeding with data collection. It is desirable that the evaluation of the eligibility of the studies be conducted by at least two investigators. It is also advisable to use a flowchart, where the number of remaining articles in each phase of selection of the studies is evident (Donato & Donato, 2019; Ward, Usher-Smith & Griffin, 2019; Petrou, Kwon & Madan, 2018).
- Assessment of the quality of studies: when reading studies, quality assessment scales should be used. The method chosen should be the one that best fits the type of review being carried out (Donato & Donato, 2019).
- Data extraction: after applying the exclusion criteria and the final list of studies having been identified, different methods can be used to extract the data. Both extraction requirements and extraction forms must be tailored to the research question(s). As a rule, these data are extracted into tables that compile the relevant information from all studies, and which allow the analysis of results (Harris et al., 2014; Wright et al., 2007).
- Data synthesis and assessment of the quality of evidence:in order to be able to draw valid and logical conclusions, after data collection, these have to be summarized and combined with the results of the different studies. For Donato and Donato (2019), the synthesis must take into account the strength of the evidence, verify that the observed effects are consistent between the different studies, and, if divergences arise, seek to identify the causes of these divergences. After all these requirements are met, it is possible to draw conclusions, and researchers should always direct the analysis to the starting question(s) and ask if the evidence obtained is sufficient to answer the research question(s). (Donato & Donato, 2019).
- Dissemination of results: after the conclusion of the work, its publication becomes important.
Main steps of the systematic review of the literature on the application of the BSC in Hospital Unit
In order to better understand the application of the BSC in hospital institutions, a systematic review of the literature was used, as already mentioned. This methodology is intended to identify and systematize relevant information on this topic. After having previously explained what a systematic literature review is, we will now describe each of the stages of our investigation.
General Objective and Research Questions
The general objective of this research is to make a diagnosis of the state of the art regarding the implementation of the BSC in Hospital Units. To achieve this objective, the following research questions were elaborated: What are the characteristics of the publications that report the application of the BSC in hospitals?; What is the motivation for using the BSC?; What are the characteristics of the hospitals where the BSC was implemented?; Who are the actors in the process of designing and implementing the BSC?; What are the perspectives and performance indicators most frequently used in the application of the BSC in hospitals?; What are the facilitating factors in design and implementation?; What are the results obtained with the implementation of the BSC?; What are the difficulties and/or limitations to the implementation of the BSC?; What suggestions are made for future investigations in this area? To answer these questions, we carried out a systematic review of the literature.
descriptors
The search for publications in the databases was performed according to the following descriptors: (“Scorecard” OR “BSC”) AND “hospital”. The use of the Boolean operator “OR” allowed us to combine the different descriptors (“scorecard” and “BSC”), in the same way, in the different databases. In turn, the Boolean operator “AND” allowed us to find articles that bring together two or more ideas, that is, in which both terms (that is, scorecard or BSC and hospital) appear simultaneously in the document.
Search sources
In this study, our focus was on works published in specialized journals. Using the keywords mentioned above, the “Scopus” and “Web of Science” databases were used, and the survey was carried out on 04/30/2022. In this survey, a total of 83 publications (53 in “Scopus” and 30 in “Web of Science”) were identified with potential interest. A second search was carried out in the Medline database, on 05/13/2022, using the same criteria that were used in the first search. Subsequently, third research was carried out, based on the bibliographic references of the literature reviews found in previous researches.
Inclusion criteria
As inclusion criteria, the following were defined:
- Articles that present the aforementioned descriptors in the title;
- Articles written in all languages;
- Empirical articles focused on the application of the BSC in a hospital context;
- Articles published in scientific journals;
Exclusion Criteria
In addition to defining inclusion criteria, it became pertinent to define exclusion criteria as well. As such, among all the articles selected, those that contained the criteria identified below were excluded:
- Not focused on the application of the BSC to hospital evaluation;
- Non-empirical, although focused on the BSC in a hospital context;
- Written in research format, conference minutes or opinion article;
- Literature reviews;
- Full text not found, after best efforts on the author's part.
Selection of articles
The research took place in three phases, with the 1st phase of the research only covering the Scopus and Web of Science databases, which resulted in 83 articles (N = 83).
In a first phase, these articles were organized by author(s), article title, place of publication, year of publication, and abstract. After removing the duplicate articles, 55 articles remained for analysis, which took place, first, through the title and abstract.
From this first screening, and taking into account the inclusion and exclusion criteria, 36 articles were excluded (19 articles did not focus on the application of the BSC; nine articles did not provide access to the full text; three articles discussed literature reviews; one article was written in Spanish, one article did not address the application of the BSC in the hospital area, one article was not published in a peer-reviewed journal, but in a hospital journal, and two articles did not discuss empirical applications).
With the exclusion of these articles, 19 articles remained for analysis. Given the reduced number of articles, it was considered prudent to carry out a new search, in an attempt to increase the number of articles that met the criteria to be included in this study.
The second search was carried out in the Medline database, on 03/13/2020, using the same criteria that were used in the first search. The main objective of using this database is to increase the number of articles relevant to the review in question. With this research, 41 publications were found, of which 3 were selected. The reason for excluding the remaining 38 publications was: 31 articles were duplicated; two articles did not focus on the application of the BSC; one article discussed a systematic review; one corresponded to a book; two articles did not have a full text and one article did not discuss an empirical application. In order to ensure that no relevant article was left out, it was decided to carry out a third search.
In this research, the bibliographic references of the literature reviews that appeared in the previous listings, and from which we had access to the full text, were analyzed. Following this analysis, 15 potential articles were identified, of which, after analysis, only two articles were selected. The reason for excluding the remaining 13 articles was as follows: four articles for not being an empirical study, three articles for being a literature review, one article for not focusing on the application of the BSC and five articles for not being able to access the text complete despite our best efforts. In total, 24 articles were included in this review (Appendix 1). It should be noted that in articles where the full text was not found and which were potentially relevant to the study, an email was sent to the respective authors, the full text has not been received. The flowchart below shows the process of obtaining the final sample (Figure 3.1).
In order to answer the research questions and achieve the objectives of this work, a summary table of the articles reviewed was constructed, which contains information on: article authors, study objective(s), study motivations, hospital characteristics (public, private, public-private and social), country where implementation took place, level of implementation (global/specific), stakeholders, perspectives, performance indicators, facilitating factors, main conclusions, benefits, risks, study difficulties, limitations to the use of the BSC and suggestions for future investigations.
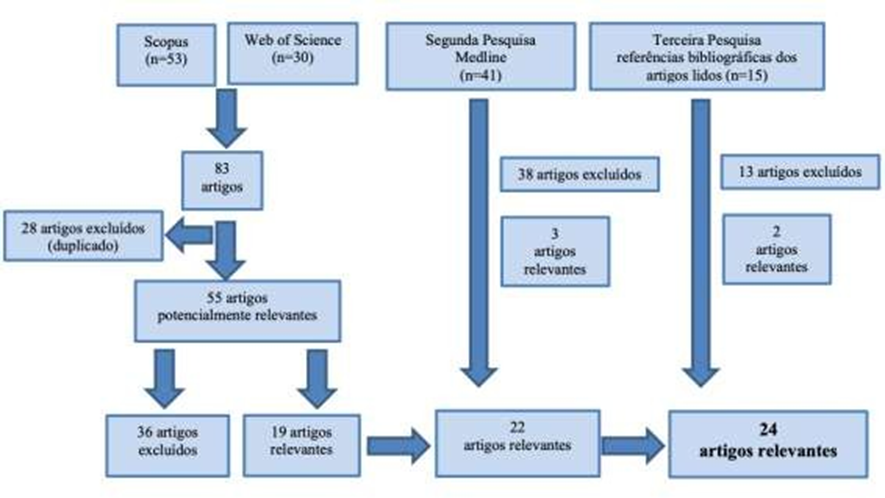
Analysis And Discussion of Results
As this research is a literature review, which aims to summarize information on the state of the art regarding the application of the BSC in Hospital Units, we sought to answer the nine guiding questions of the work (presented below).
To this end, a table was developed where it was possible to group all the information extracted from the 24 articles, so that, at a later stage, the results could be analysed and discussed. The bibliographic references of the analyzed articles can be found in Appendix 1.
Next, we will proceed to the analysis and discussion of the results obtained, in order to answer each of the questions posed.
Question 1: What are the characteristics of publications that report the application of the BSC in h
This first question aims to characterize the selected studies, in terms of: year and place of publication, type of study and study objectives.
The articles selected for this literature review were published between 1998 and 2020, in reputable newspapers and magazines in this area, namely: Journal of Modeling in Management, International Journal of Health Planning and Management, Shiraz & Medical Journal, Journal of International Medical Research, Journal of Strategy and Management, International Journal of Productivity and Performance Management, Expert Systems with Applications, International Journal of Health Care Quality Assurance, Journal of the Chinese Medical Association, Health Policy, Implementation Science, Cost Effectiveness and Resource Allocation, Health Care Manage Review, Total Quality Management, International Journal of Enterprise Network Management, Health Care Management Review, Journal of Health Care Finance, Journal of Pain and Symptom Management, Advances in Patient Safety: new directions and alternative approaches, Studies in Health Technology and Informatics, and Journal of Healthcare Management.
From the studies found, we found that the number of publications related to the use of this tool has increased in recent years. In the first decade of existence of the BSC (1992 to 2000) we found one publication, in the second decade of existence of this tool (from 2001 to 2010) we found 11 publications and then in the last 10 years (2011 to 2020) 13 publications were found. This increase may be associated with the combination of several factors, namely: publication of the book “The Execution Premium” by Kaplan and Norton in 2008, which contributed to the dissemination and recognition of the merits of this tool; greater concern with the level of performance in the health sector and growing appreciation around this tool.
The studies included in this review are mostly qualitative (12 qualitative studies, 5 quantitative studies and 7 mixed studies: qualitative and quantitative), and aimed to:
- performance evaluation through the implementation of the BSC (Martunis et al., 2020; Lin et al., 2013; Chen, Hou & Chang, 2012; Naranjo-Gil, 2009; Chang et al., 2008);
- compile a set of performance indicators for each of the four perspectives (Behrouzi & Ma'aram, 2019; Gao et al., 2018; Rabbani et al., 2010);
- describe the development and implementation of the first performance indicator in a hospital (El-Jardali et al., 2011);
- explore contextual perspectives in relation to the implementation of the BSC in a hospital (Rabbani et al., 2011);
- identify and rank a set of performance indicators that are reliable and relevant for private hospitals (Behrouzi & Ma'aram, 2019);
- analyze the relationship between key indicators (Rahimi et al., 2018; Yang & Tung, 2006);
- develop recommendations for policy creation and development in hospitals (Gao et al., 2018);
- analyze the cause-effect relationship between the process and the reported measures (Porporato, Tsasis, & Marin, 2017);
- explore how the BSC development process in a hospital department can be a key factor in developing a quality improvement strategy (Smith & Loonam, 2016; Schmidt et al., 2006);
- describe the process of creating the BSC for a hospital system (Pink et al., 2001);
- adapt the BSC to the public health sector (Koumpourus, 2013; Qudrat-Ullah, Chow & Goh, 2007);
- implement the application of the BSC in the health sector (Verzola et al., 2009);
- confirm the reliability and value of using the BSC to measure the performance of two hospitals in different countries (Chen et al., 2006).
Given the importance that the BSC can assume in improving the performance of a Hospital Unit, and, as our objective is to clarify the process of creation, definition and implementation of this tool by analyzing the objectives of these studies, it seems to us that its selection will have been the and will allow us to identify common points, facilitating elements, failures and difficulties experienced in the process of developing this tool.
Question 2: What is the motivation for using the BSC?
The motivations for applying the BSC in the health context can be varied and are influenced by the scope of institutions (public, private, public-private and social), as we have already mentioned in the course of this literature review. This variability of motivations is reflected in the studies selected in the present systematic review.
However, of the 24 studies selected, only 15 (Martunis et al., 2020; Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Gao et al., 2018; Porporato, Tsasis & Marin, 2017; Smith & Loonam, 2016; Koumpouros, 2013; Chen, Hou & Chang, 2012; El-Jardali et al., 2011; Rabbani et al., 2011; Verzola et al., 2009; Naranjo-Gil, 2009; Chen et al., 2006; Yang & Tung, 2006; Inamdar, Kaplan & Bower, 2002) refer to the motivation that led to the application of this tool (Table 4.1).
One of the most recent studies to document an application of the BSC in a hospital context is the study by Martunis et al. (2020), whose main motivation was improve the current and future state of health care provided by the analyzed hospital, as well as promote efforts to improve the hospital's benefits without neglecting its social function.
Although there are numerous studies on the application of performance measures in the health system, there was a lack of an effective method to help private hospitals to identify and classify their performance from the perspectives of the BSC. This was essentially the motivation behind the work of Behrouzi and Ma'aram (2019).
Table 4. 1 - Studies that refer to the motivation that led to the application of the BSC
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Porporato, Tsasis & Marin (2017) | Smith & Loonam (2016) | Koumpouros (2013) | Chen, Hou & Chang (2012) | El-Jardali et al., (2011) | Rabbani et al., (2011) | Verzola et al., (2009) | Naranjo-Gil (2009) | Chen et al., (2006) | Yang & Tung (2006) | Inamdar, Kaplan & Bower (2002) | ||
MOTIVATION TO USE THE BSC IN HOSPITAL INSTITUTIONS | Improve the care provided | X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
Promote efforts to improve the benefits of the Hospital | X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||
Develop a performance appraisal system | Public |
|
|
| X |
|
|
|
|
|
| X | X |
|
|
| |
Private |
| X |
|
|
|
|
|
|
| X |
|
|
|
|
| ||
Standardize evaluation and monitoring measures |
|
|
|
|
|
|
|
| X |
|
|
|
|
|
| ||
Increasing demands |
|
|
|
|
|
|
|
| X |
|
|
|
|
|
| ||
Definition of priority needs |
|
|
|
|
|
|
|
| X |
|
|
|
|
|
| ||
Deepenknowledge about | the relationship between perspectives and performance indicators |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |
factors that influence the hospital performance |
|
|
|
|
|
|
| X |
|
|
|
|
|
|
| ||
indicators that improve the hospital performance |
|
|
|
|
|
|
| X |
|
|
|
|
|
|
| ||
the motivation, experience and results obtained with the implementation of the BSC (executives' perspective) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
X | ||
Deepen empirical research on the application of the BSC in hospital context |
|
|
|
| X | X |
|
|
|
|
|
|
| X |
| ||
Discussion of a real case of application of the BSC in a hospital context |
|
|
|
|
|
| X |
|
|
|
|
|
|
|
| ||
Understand the differences between hospitals in different countries |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
| ||
Discuss the reliability and value of the BSC as a system of hospital performance measurement |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
| ||
Since 2005, the need for standardized and comparable measures for evaluation and monitoring has been raised by various stakeholders during policy meetings and development workshops. The increase in demand and definition of priority needs was the basis for the decision to develop and implement, by El-Jardali et al. (2011) Lebanon's first standard hospital indicators system.
Although the BSC is widely used in the health sector, there is limited knowledge of the relationship between perspectives and performance indicators, so the work of Rahimi et al. (2018) sought to deepen knowledge about these relationships.
Gao et al. (2018) had as their main motivation the development of a performance evaluation system for hospitals in the municipality of Guangxi, which can reflect the social and cultural context of the province.
The literature demonstrates several constraints in the application of the BSC in the area of health care; however, very few have been empirically tested. This need was the main motivation of Porporato, Tsasis and Marin (2017), in a first attempt to analyze some of these constraints, with data collected by a hospital that has been using the BSC for more than a decade.
Smith and Loonam (2016), considered that there was a lack of empirical research that discusses the implementation of the Balanced Scorecard, from the perspective of health care. Their study demonstrates the process of developing an effective BSC in the health sector.
The main motivation pointed out by Koumpouros (2013) is related to the discussion of the application of the BSC in healthcare in Greece. The article presents, for the first time, a real example of the application of the BSC in public health care systems in Greece.
The effect of the implementation of the BSC in the hospital organization has rarely been described, and the research carried out has mostly used qualitative data, which does not allow the verification of data captured from real cases. Through the use of experimental data, Chen, Hou and Chang (2012) hope to improve knowledge about the factors that positively influence hospital performance and the use of indicators that improve this performance.
The purpose of the study carried out by Rabbani et al. (2011), was the implementation of a modern management tool, the BSC, in a private academic hospital in Karacho, Pakistan. The main operational question was: “What are the contextual circumstances in which the BSC was implemented in four units of this hospital?". Considering the importance given to context in the Pettigrew and Wipp's Framework (PGF) and the influence of context on implementation process and contents, the PGF was selected, as a framework, to pose secondary questions related to the what, how and why of the implementation of the BSC.
At Ferrara University Hospital there was no balanced performance appraisal system. The objectives to be achieved within a year are defined for each department, and are economic and organizational. Thus, the overall performance of Operation Units was never evaluated, which was the main motivation of Verzola et al. (2009).
The study by Naranjo-Gil (2009) focuses on the use of the Balanced Scorecard by nurse managers in Spanish hospitals, because they are in a crucial position to lead the implementation of this tool, as a strategic performance evaluation system.
Helping to understand the differences between hospitals in two different countries was one of the motivations of Chen et al. (2006). Furthermore, the authors discuss the reliability and value of using the BSC to measure hospital performance internationally.
Yang and Tung (2006) pointed out as motivation the fact that no study has empirically verified the causality in the structure of the BSC in the health care industry.
The oldest publication to point out the motivation was that of Inamdar, Kaplan and Bower (2002), which refers to the existence of a gap in the literature, which describes, from the perspective of the executives who implemented the BSC in their organizations, the motivation, experience and results.
Due to the different motivations reported throughout the analyzed publications, it appears that this tool's potential is recognized as a driver for the improvement of care provided and as a system for evaluating and improving the performance of hospital institutions. It is also recognized that although in recent years there has been an increase in interest in the BSC, it is necessary to carry out more empirical studies and analyze the application of this tool, according to the different political and social contexts, thus allowing to deepen knowledge about this tool, define and standardize implementation, evaluation and monitoring procedures.
Question 3: What are the characteristics of the hospitals where the BSC was implemented?
Depending on the geographic location, as well as the sector where the hospital is located, this will be the way in which the BSC is implemented. That said, it is important to classify the hospitals involved in the selected studies, taking into account the sector to which they belong, as well as their geographic distribution and the level of implementation of the BSC within the Hospital Unit (Table 4.2).
Table 4. 2 - Characterization of hospitals and level of implementation
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Porporato, Tsasis & Marin (2017) | Smith & Loonam (2016) | Lin et al., (2013) | Koumpouros (2013) | Weiss & Downar (2013) | Chen, Hou & Chang (2012) | El-Jardali et al., (2011) | Rabbani et al., (2011) | Rabbani et al., (2010) | Verzola et al., (2009) | Naranjo-Gil (2009) | Chang et al., (2008) | Meliones et al., (2008) | Qudrat-Ullah, Chow & Goh (2007) | Chen et al., (2006) | Schmidt et al. (2006) | Yang & Tung (2006) | Inamdar, Kaplan & Bower (2002) | Pink et al., (2001) | Gordon et al. (1998) | |
FEATURESFROM HOSPITAL | Public sector | X |
| X | X | X |
|
| X |
| X |
|
|
| X | X |
|
| X | X | X | X |
|
| X |
Private sector |
| X |
|
|
|
|
|
|
|
|
| X | X |
|
|
|
X |
|
|
|
|
|
|
| |
Public sector-private |
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
| |
Social Sector |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
| |
Not specified |
|
|
|
|
| X | X |
| X |
|
|
|
|
|
|
|
|
|
|
|
| X | X |
| |
IMPLEMENTATION LEVEL | Global |
| X | X | X | X |
|
|
|
| X | X |
| X |
|
| X |
| X | X |
| X |
| X |
|
Specific |
|
|
|
|
| X |
|
|
|
|
| X |
|
|
|
|
|
|
| X |
|
|
| X | |
Other | X |
|
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |
Not specified / No applicable |
|
|
|
|
|
|
|
X |
X |
|
|
|
|
X |
X |
|
X |
|
|
|
|
X |
|
| |
COUNTRY | Indonesia | Malaysia | Iran | China | Canada | Ireland | China | Greece | Canada | Taiwan | Lebanon | Pakistan | Pakistan | Italy | Spain | Taiwan | United States | Malaysia | China and Japan | UK | Taiwan | Not specified | Canada | Canada | |
Analysing the data obtained, we conclude that most studies concern implementations of the BSC in public sector hospitals (13), which demonstrates that this tool, initially developed to support the management of private companies, has gained projection and importance. also, in the public sector. There are still four studies related to private hospitals that implemented this tool, a public-private hospital and a social sector hospital. There are six studies in which it is not possible to assess the sector of activity of the Hospital Unit.
With regard to geographic distribution, and taking into account the selected studies, we conclude that most studies focused on the application of the BSC in the hospital sector are located in Asia (China, Taiwan, Malaysia, Indonesia and Pakistan) and South America. North (Canada and United States). At the European level, only four studies were found (Spain, Greece, Italy and the United Kingdom). These results seem to indicate a lack of recognition, at the European level, regarding the advantages of applying this tool, contrary to what happens in Asia and North America.
In the selected publications, the BSC was mostly applied at a global level (12), that is, to evaluate and manage the performance of the Hospital Unit as a whole, with only four of the studies reporting that the application of the BSC was limited to a service /department/sector of the Hospital Unit. There are still six publications that do not specify the level of analysis at which the BSC was applied.
Question 4: Who are the stakeholders in the design and implementation of the BSC?
The choice and selection of those involved in the process of designing and implementing the BSC assumes special relevance, as we have already mentioned throughout this research. There is a recognition in the literature that it is important for the success of the design and implementation process that the team responsible for it is defined by top management, and that it has three types of actors: leader, development team and team of specialists (Vitória, 2017; Santos, 2014)
With the analysis of the 24 publications, we found that there is no uniformity in the actors in this process. Although 10 studies do not specify which actors are involved in the design and implementation of the BSC, in the remaining 14, most actors are Managers and Directors (Table 4.3).
Table 4.3 – Stakeholders in the BSC design and implementation process (for studies where this is specified)
| Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Porporato, Tsasis & Marin (2017) | Smith & Loonam (2016) | Lin et al., (2013) | Koumpouros (2013) | El-Jardali, et al., (2011) | Rabbani et al., (2010) | Naranjo-Gil (2009) | Chang et al., (2008) | Inamdar, Kaplan & Bower (2002) | Pink et al., (2001) | Gordon et al., (1998) | ||
STAKEHOLDERS |
managers | Top Managers (includes Senior Administrator and executives) | X |
|
|
| X |
| X |
|
|
|
| X |
|
|
Hospital Managers |
|
|
|
|
| X |
|
|
|
|
|
|
|
| ||
Strategic Planning Managers |
|
|
| X |
|
|
|
|
|
|
|
|
|
| ||
Encoding Manager |
|
|
|
| X |
|
|
|
|
|
|
|
|
| ||
Managers without BSC experience |
|
|
|
|
|
|
|
|
|
|
|
|
| X | ||
Managers with BSC experience |
|
|
|
|
|
|
|
|
|
|
|
|
| X | ||
Unit Management Teams |
|
|
|
|
|
|
|
|
|
|
|
|
| X | ||
directors | Nursing Director |
|
|
|
|
|
|
|
|
|
| X |
|
|
| |
Medical Director |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Human resources director |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
CFO |
|
|
| X | X |
|
|
|
|
| X |
|
|
| ||
Medical Research Director |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Director of Operations |
|
|
|
|
|
|
|
|
|
| X |
|
| X | ||
Director of Information Systems |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Health professionals |
|
| X |
| X | X |
|
|
| X | X |
|
|
| ||
Other Professionals in Hospital Units | Administrative staff |
|
|
|
|
|
|
|
|
|
| X |
|
|
| |
Social service |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Financial Advisory Panel |
|
|
|
|
|
|
|
|
|
|
|
| X |
| ||
engineering department |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Church Elements |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
auditors |
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Panel of Experts (representatives of different areas) |
| X | X |
|
|
|
| X | X |
|
|
|
|
| ||
users |
|
| X |
|
|
|
|
|
|
|
|
|
|
| ||
Study Author and Scholars |
|
|
|
|
| X |
|
|
|
|
|
|
| X | ||
Deepening the analysis of the results obtained, it appears that only three studies have only management elements as actors, namely top managers. This may be a criticism to point out to these studies, because, according to the literature (eg Vitória, 2017), although the involvement and commitment of top managers is essential to achieve the intended results, it is equally important that there are other dynamic elements in the team and that contribute to the development and supervision of this process.
There is a study (Gao et al., 2018) that documents an implementation of the BSC that did not involve either management or management elements, but which had as added value the involvement of health professionals, a panel of experts in the different areas. areas, and user involvement. Considering that the involvement of users is crucial, given that their satisfaction represents the main mission of hospital units, this is undoubtedly a positive point to consider.
Assuming the results obtained through the analysis of the selected articles, we can conclude that the successful implementation of the BSC implies that from its the design and implementation process include the following elements: top management and management, health professionals, leading professionals from each sector where the BSC is intended to be implemented, a panel of experts in this tool, users and academics. Although it may seem that the team is large, each of the elements will play a crucial role in each phase. Top management, in a top-down methodology, will define the team, appoint the project leader and will be crucial, as a source of information, for the entire hospital community (Vitória, 2017; Santos, 2014; Collis & Rukstad, 2008; Kaplan & Norton, 1996). Management elements and reference professionals in the implementation sectors will be central to the collection and dissemination of information and the construction of implementation plans (Santos, 2014; Chang et al., 2008). The panel of experts and academics will be fundamental as team trainers and indispensable in the analysis and monitoring of the process (Rahimi et al., 2018; Santos, 2014; Lin et al., 2013). Finally, users can also play a prominent role in the team as representatives of the target audience and the mission of the Hospital Unit (Gao et al., 2018).
Question 5: Which perspectives and performance indicators are most frequently used in the applicatio
In order to understand the perspectives and indicators most commonly used in the application of the BSC, within the scope of hospital organizations, we sought to identify them in the different publications.
With regard to the perspectives used (Table 4.4), most studies
(13) uses only the original perspectives of the Kaplan and Norton model. However, some studies choose to partially modify the perspectives or add others, thus proving the flexibility of this tool. This modification may be closely related to the need to design assessment systems perfectly adjusted to the characteristics and specificities of each hospital, as is the case of the study by Chang et al. (2008), which is a hospital of a social nature, having been added a perspective called “Social Commitment”.
Although it is not found in Table 4.4, as it is not possible to identify which perspectives were used, it is important to refer to the study by Naranjo-Gil (2009). This study focuses on the investigation of the relationship between the characteristics of nurse managers and the two types of use of scorecards (interactive or diagnostic) and the consequent effect on the strategic performance of hospitals. This is an interesting study that helps to understand the scope of this tool.
Table 4. 4 - Perspectives used in the different articles analysed
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi, et al., (2018) | Gao et al., (2018) | Porporato, Tsasis & Marin (2017) | Smith & Loonam (2016) | Lin et al., (2013) | Koumpouros (2013) | Weiss & Downar (2013) | Chen, Hou & Chang (2012) | El-Jardali et al., (2011) | Rabbani et al., (2011) | Rabbani et al., (2010) | Verzola et al., (2009) | Chang et al., (2008) | Meliones et al., (2008) | Qudrat-Ullah, Chow & Goh (2007) | Chen et al., (2006) | Schmidt et al., (2006) | Yang & Tung (2006) | Pink et al., (2001) | Inamdar, Kaplan & Bower (2002) | Gordon, et al., (1998) | |
OUTLOOK | financial | X | X | X | X |
| X | X | X |
| X | X | X | X | X | X | X | X | X | X | X | X | X | X |
Customers | X | X | X | X |
| X | X | X |
|
|
|
|
| X | X | X |
| X | X | X |
| X | X | |
Law Suit internal | X | X | X | X |
| X | X | X |
|
|
| X | X | X | X |
|
| X | X | X |
| X | X | |
learning and Knowledge |
X |
X |
X |
X |
|
X |
X |
X |
|
|
|
|
X |
X |
X |
|
|
X |
X |
X |
|
X |
| |
Others |
|
|
|
| X |
|
|
| X | X | X | X |
|
| X | X | X |
|
|
| X |
| X | |
The way in which the different perspectives are organized, throughout the different publications, is also not watertight, and depends a lot on the nature of the Hospital Unit (public, private, public-private or social).
With regard to innovative elements in terms of perspectives, we found some studies that differed from traditional perspectives. Porporato, Tsasis and Marin (2017) focus on a single perspective, which they call “Best patient experience”. Weiss and Downar (2013) also focus on a single perspective, which they call “User-centered quality”. All other studies present more than one perspective, adding to traditional perspectives or replacing them with other elements. Chen, Hou and Chang (2012) use the financial perspective and add the perspectives “Admission performance”, “Administration” and “Quality of care”. Also, El-Jardali et al. (2011) use the financial perspective, but complement it with the “Clinical Use and Results” perspectives. “Integration of Systems and Human Resources” and “User Satisfaction”. In turn, Rabbani et al. (2011) use the Financial and Internal Processes perspective, but add the following perspectives “Human Resources” and “User Satisfaction”. Already, Chang et al. (2008) uses the four classical perspectives and add the perspective “Social Commitment”, while Qudrat-Ullah, Chow and Goh (2007) use the financial perspective and add three perspectives that they call “Better indicators”, “Faster indicators” and “Cheaper indicators”. Pink et al. (2001) also use the financial perspective, refer to the use of other perspectives, but do not specify them. In turn, Meliones et al. (2008) use the financial perspective and the Customer perspective and use two other perspectives “Work culture” and “Quality and Patient Safety”, while Gordon et al. (1998) use the Financial, Customers and Internal Processes perspectives and complement them with another perspective that they simply call “Innovation”. Once again, the importance of the financial perspective is notorious, being the one that is most present in the different studies (21 studies),
Regarding innovations, in terms of perspectives, we have two studies (Gao et al., 2018; Inamdar, Kaplan & Bower, 2002) in which different weights were assigned to each of the perspectives, which seems to be closely related to the strategic objectives of the Hospital Units where the study was developed.
With the data obtained, we can infer that the four perspectives originally created by Kaplan and Norton are suitable for the application of the BSC in the hospital sector,
although they may need to be slightly modified, given the complexity of the sector and the specificities of each of the organizations evaluated.
Moving on to the analysis of the performance indicators used for the different perspectives, they are identified in Tables 4.5; 4.6; 4.7; 4.8; 4.9 and 4.10. Pink et al. (2001) stresses the importance of being flexible in choosing indicators, as they must reflect critical performance problems and may change over time. This aspect of flexibility stands out in the reviewed literature. It should be noted that two studies do not mention indicators for the different perspectives, but rather, objectives to be achieved for each of the considered perspectives. These are the studies by Smith and Loonam (2016) and the study by Verzola et al. (2009).
Regarding the “Financial” perspective, as indicated in Table 4.4, of the 24 publications analyzed, 21 considered this perspective. The indicators used by each of the authors are explained in Table 4.5 (it should be noted that in thistable only studies that refer to the indicators used are included).
Table 4. 5 – Indicators from the Financial perspective (referring to the studies that included this perspective)
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Lin et al., (2013) | Koumpouros (2013) | Chen, Hou & Chang (2012) | El-Jardali et al., (2011) | Rabbani et al., (2011) | Rabbani et al., (2010) | Chang, et al., (2008) | Qudrat-Ullah, Chow & Goh (2007) | Chen et al., (2006) | Schmidt et al., (2006) | Yang & Tung (2006) | Pink et al., (2001) | Gordon et al., (1998) | |||
| INDICATORS | |||||||||||||||||||
FINANCIAL | value-for-money | X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| ||
Return on investment |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Asset turnover rate |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
cash flow |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Average profit per bed |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
debt ratio |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Return on equity |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Stock turnover rate |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
current ratio |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Income to total cost ratio |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
% hospital deductions |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Profitability and Expense |
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Ability to pay debts |
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Return per employee |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Turnover by capital (capital turnover) |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Low-cost administration |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Production and distribution at minimal cost |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Customer-focused purchasing processes at lowest possible cost |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Growth potential |
|
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
| |||
Occupation |
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
|
| |||
overtime |
|
|
|
|
|
|
| X |
|
|
|
|
| X |
|
|
| |||
cash flow |
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
|
| |||
Hospitalization Time |
|
|
|
|
|
|
|
| X | X |
|
|
|
|
|
|
| |||
daily census |
|
|
|
|
|
|
|
| X | X |
|
|
|
|
|
|
| |||
Low-cost outpatient referral fee |
|
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
| |||
Number of referrals for hospitalization |
|
|
|
|
|
|
|
| X |
|
|
|
|
|
|
|
| |||
market share |
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
| |||
Customer retention rate |
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
| |||
Customer loyalty rate |
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
| |||
Asset turnover |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
| |||
Return on Assets (ROA) |
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
| |||
Current Ratio |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| |||
Inventory days |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| |||
| corporate services |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| ||
| Hours of nursing care in % by total nurses interned |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| ||
| working capital |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| ||
| Productivity |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X | ||
| Financial balance |
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Costs and expenses | Agency costs |
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Training costs |
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
| |||
Average cost per case |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X | |||
equipment expenses |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| |||
Unit cost performance |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| |||
Change of costs by case |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
| |||
Personnel expenses as a % of total revenue from customers |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
| |||
Material costs as a % of total revenue from customers |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
| |||
Average costs charged |
|
|
|
|
|
|
|
| X | X |
|
|
|
|
|
|
| |||
Controllable costs |
|
|
|
|
|
| X |
|
|
|
|
|
|
|
|
|
| |||
Medication and material cost |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Daily cost per user |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
% of personnel costs of total costs |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Average expenses per bed per day |
|
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Margin | Operating profit margin |
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
|
| ||
Total Margin |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| X |
| |||
Profit margin |
|
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
| |||
Net Income/Financial Contribution Margin |
|
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
| |||
net profit margin |
| X |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| |||
Margins |
|
|
|
| X |
|
|
|
|
|
|
|
|
|
|
|
| |||
Operating net margin |
|
|
|
|
|
|
|
| X | X |
|
|
|
|
|
|
| |||
Revenue | Revenue (in millions) |
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
|
| ||
Revenue from services not covered by The National Health Insurance (NHI) |
|
|
|
|
|
|
|
|
|
| X |
|
|
|
|
|
| |||
Analyzing Table 4.5, one can see the importance that this perspective assumes in the different sectors (public, private, public-private and social), due to the high number of indicators used in different studies. However, the most used are the indicators related to costs and expenses, used in 9 of the 21 studies that used this perspective (Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Chen, Hou & Chang, 2012; Rabbani et al., 2011; Rabbani et al., 2010; Chen et al., 2006; Schmidt et al., 2006; Pink et al., 2001; Gordon et al., 1998). As an example of the indicators referring to costs and expenses, we have “training costs”, “average cost per case”, “average costs charged”, “material costs as a % of total revenue from clients”, “medication and material costs””, “Personnel Costs % of Total Costs”, “Personnel Expenses as a % of Total Customer Revenues” and “Equipment Expenses”. Still within the group of the most used indicators, indicators related to the “margin” used in eight studies are included (Behrouzi & Ma'aram, 2019; Lin et al., 2013; Rabbani et al., 2011; Rabbani et al., 2010; Qudrat-Ullah, Chow & Goh, 2007; Chen et al., 2006; Yang & Tung, 2006; Pink et al., 2001). Within the indicators related to the margin, we can refer to “operating profit margin”; “total margin”; “profit margin” and “net operating margin”.
There are other indicators within this perspective, which, although not used so often, are equally important, namely indicators related to the “level of income” (Chang et al., 2008); “average profit per bed” (Behrouzi & Ma'aram, 2019); “return in equity” (Behrouzi & Ma'aram, 2019); “ability to pay debts” (Gao et al., 2018); “return per employee” (Lin et al., 2013); “cash-flow” (El-Jardali et al., 2011); “asset turnover” (Chen et al., 2006); “return on assets” (Yang & Tung, 2006); “productivity” (Gordon et al., 1998) and “financial balance” (Schmidt et al., 2006).
It is important to point out that all indicators are important, however, it is necessary to understand the reality of the institution on which you are working and what is its mission and vision.
Regarding the customer perspective, from the analysis of the different articles, it was possible to identify the indicators transcribed to Table 4.6.
From this perspective, the most used indicator is “user satisfaction rate”, having been identified in nine of the analyzed studies (Martunis et al., 2020; Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Gao et al., 2018; Koumpouros, 2013; Chen et al., 2006; Yang & Tung, 2006; Gordon et al., 1998). Still regarding the rate of satisfaction, the study by Chang et al., (2008) also uses this indicator, but in a disaggregated way, in order to capture the “user satisfaction rate with hospitalization”, the “user satisfaction rate with the outpatient clinic” and the “user satisfaction rate with the emergency department”. The same happens with Lin et al., (2013) who use this indicator to capture the “user satisfaction rate with the operating team”.
Table 4. 6 – Indicators from the Customer perspective (referring to studies that included this perspective)
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Lin et al., (2013) | Koumpouros (2013) | Chang et al., (2008) | Chen et al., (2006) | Yang & Tung (2006) | Gordon et al., (1998) | ||
| INDICATORS | |||||||||||
Customers |
satisfaction rate | of users | X | X | X | X |
| X |
| X | X | X |
of users with hospitalization |
|
|
|
|
|
| X |
|
|
| ||
of users with the outpatient clinic |
|
|
|
|
|
| X |
|
|
| ||
of users with the emergency department |
|
|
|
|
|
| X |
|
|
| ||
of users with the operating team |
|
|
|
| X |
|
|
|
|
| ||
Number/rate of user complaints |
| X | X |
| X |
|
|
|
|
| ||
Waiting time | Medium |
| X |
|
| X |
|
|
|
| X | |
for outpatient |
|
|
|
|
|
|
| X |
|
| ||
User retention rate |
| X |
|
|
|
|
|
|
|
| ||
Average length of stay |
| X |
|
|
|
|
|
|
|
| ||
% of postoperative infections |
| X |
|
| X |
|
|
|
|
| ||
Mortality rate |
| X |
|
|
|
|
|
|
|
| ||
% of new users |
| X |
|
|
|
|
|
|
|
| ||
User growth rate |
|
|
|
|
|
|
|
|
|
| ||
% Of transfers to other hospitals |
| X |
|
|
|
|
|
|
|
| ||
Charge with medical expenses |
|
|
| X |
|
|
|
|
|
| ||
social expenses |
|
|
| X |
|
|
|
|
|
| ||
Facilities for family and visitors |
|
| X |
|
|
|
|
|
|
| ||
Duration of Surgery |
|
|
|
| X |
|
|
|
|
| ||
Post-operative recovery time |
|
|
|
| X |
|
|
|
|
| ||
Ability to provide timely services to users |
|
|
|
| X |
|
|
|
|
| ||
Ability to respond to user questions |
|
|
|
| X |
|
|
|
|
| ||
Provision of sufficient and accurate information |
|
|
|
| X |
|
|
|
|
| ||
Case mix index |
|
|
|
|
|
| X |
|
|
| ||
Market share |
|
|
|
|
|
|
|
| X |
| ||
number of cancellations |
|
|
|
|
|
|
|
|
| X | ||
Next, the most used indicators in this perspective are the “number/complaint rate from users”, mentioned in three studies (Behrouzi & Ma'aram, 2019;
Rahimi et al., 2018; Lin et al., 2013). Also used three times is the indicator “average waiting time” (Behrouzi & Ma'aram, 2019; Lin et al., 2013; Gordon et al., 1998).
Analyzing Table 4.6 and taking into account the number of indicators considered, we found that there are two studies (Behrouzi & Ma'aram, 2019; Lin et al., 2013) who gave special importance to this perspective, as they included a considerable number of indicators that allowed them to assess the perspective of customers, thus revealing a great concern for customers.
There are still other studies that are not explained in the previous table, but that also address this perspective. Smith and Loonam (2016) and Verzola et al., (2009), use this perspective, but do not refer to indicators, they only mention objectives to be achieved. Meliones et al., (2008) and Inamdar, Kaplan and Bower (2002) refer to using this perspective, but do not specify indicators. Schmidt et al., (2006) focus on the customers' perspective, but adjusted to their reality. It will therefore be analyzed at a later stage.
Although not all studies use this perspective, or at least do not use it in the traditional way, as developed by Kaplan and Norton, its importance and the concern that exists around it can be seen, since the scope of the mission of the hospital units depends on their clients and how they perceive it.
From the “Internal Processes” perspective, the indicators and processes that best assess the efficiency of health organizations in achieving goals related to increasing patient satisfaction and reducing costs are identified (Freitas, 2015). Of the 24 articles analyzed, 16 of them use the “Internal Processes” perspective (Martunis et al., 2020; Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Gao et al., 2018; Smith & Loonam, 2016; Lin et al., 2013; Koumpouros, 2013; Rabbani et al., 2011; Rabbani et al., 2010; Verzola et al., 2009; Chang et al., 2008; Chen et al., 2006; Schmidt et al., 2006; Yang & Tung, 2006; Inamdar, Kaplan & Bower, 2002; Gordon et al., 1998). Of these, and as with some of the perspectives discussed above, there are three studies that do not define indicators (Smith & Loonam, 2016; Verzola et al., 2009; Inamdar, Kaplan & Bower, 2002) and a study (Schmidt et al., 2006) which states that it adapted this perspective to the reality of its objectives/context, thus being analyzed at a later stage.
Table 4. 7 – Indicators from the Internal Processes perspective (referring to the studies that included this perspective)
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Lin et al., (2013) | Koumpouros (2013) | Rabbani et al., (2011) | Rabbani et al., (2010) | Chang et al., (2008) | Chen et al., (2006) | Yang & Tung (2006) | Gordon et al., (1998) | |||
| INDICATORS | ||||||||||||||
INTERNAL PROCESSES |
Time | average length of stay |
| X | X |
|
|
|
|
|
|
|
|
| |
average length of stay in the emergency department |
|
| X |
|
|
|
|
|
|
|
|
| |||
waiting in the emergency |
|
| X |
|
|
|
|
|
|
|
|
| |||
in the correction of faults |
|
|
|
| X |
|
|
|
|
|
|
| |||
| length of stay of cirrhotic patients with spontaneous bacterial peritonitis (in |
|
|
|
|
|
| X |
|
|
|
|
| ||
| patient stay with GI bleed |
|
|
|
|
|
| X |
|
|
|
|
| ||
lab response |
|
|
|
|
|
| X | X |
|
|
|
| |||
Return to the emergency in less than 48 hours |
|
|
|
|
|
| X |
|
|
|
|
| |||
Patients admitted to the emergency department in less than 4.5 hours |
|
|
|
|
|
| X |
|
|
|
|
| |||
Patients discharged within 2 hours of admission |
|
|
|
|
|
| X |
|
|
|
|
| |||
lab response time up to 2 hours |
|
|
|
|
|
| X |
|
|
|
|
| |||
Timely discharge of patients with GI patients |
|
|
|
|
|
| X |
|
|
|
|
| |||
Delay between requesting and obtaining antibiotic appointments (hours) |
|
|
|
|
|
|
|
| X |
|
|
| |||
% Of users admitted to the ICU of the emergency department in less than 3 hours |
|
|
|
|
|
|
|
| X |
|
|
| |||
| % Of patients admitted to an emergency department ward in less than 4 hours |
|
|
|
|
|
|
|
| X |
|
|
| ||
| of stay |
|
|
|
|
|
|
|
|
| X | X | X | ||
until treatment |
|
|
|
|
|
|
|
|
|
|
| X | |||
Give me an answer |
|
|
|
|
|
|
|
|
|
|
| X | |||
Satisfaction | of students with teaching |
|
|
|
|
|
| X |
|
|
|
|
| ||
with knowledge and skills of interns |
|
|
|
|
|
| X |
|
|
|
|
| |||
Professional Satisfaction Index |
| X |
|
|
|
|
|
|
| X |
|
| |||
High with satisfaction with the care provided |
|
| X |
|
|
|
|
|
|
|
|
| |||
incidents | medical error rate |
| X | X |
|
|
|
|
|
|
|
|
| ||
Hospital infection rate |
|
| X |
|
|
| X | X |
|
|
|
| |||
Incidents with reaction to blood transfusions |
|
|
|
|
|
| X | X |
|
|
|
| |||
Needle stick injuries |
|
|
|
|
|
| X | X |
|
|
|
| |||
Number of adverse events |
|
|
|
|
|
| X |
|
|
|
|
| |||
Compliance with safety and infection control procedures |
|
|
|
|
|
| X |
|
|
|
|
| |||
Rate of medical accidents leading to court cases |
|
|
|
|
|
|
|
|
| X |
|
| |||
Complication rate |
|
|
|
|
|
|
|
|
|
|
| X | |||
fault response |
|
|
|
| X |
|
|
|
|
|
|
| |||
Professionals | Professional retention rate |
| X |
|
|
|
|
|
|
|
|
|
| ||
Professional absenteeism rate |
| X |
|
|
|
|
|
|
|
|
|
| |||
Professional turnover |
|
|
|
|
|
|
|
|
| X |
|
| |||
Occupation | bed occupancy |
| X | X |
|
|
|
|
|
| X | X |
| ||
Bed availability index |
| X |
|
|
|
|
|
|
|
|
|
| |||
Bed turnover rate |
|
| X |
|
|
|
|
|
|
|
|
| |||
Number of beds per nurse |
|
|
|
|
|
|
|
|
|
| X |
| |||
Increase/decrease in hospitalization days | X |
|
|
|
|
|
|
|
|
|
|
| |||
Increase/decrease in outpatient days | X |
|
|
|
|
|
|
|
|
|
|
| |||
Mortality rate |
|
| X |
|
|
|
|
|
| X |
|
| |||
% of canceled surgeries |
|
| X |
|
|
|
|
|
|
|
|
| |||
quality of work |
|
|
| X |
|
|
|
|
|
|
|
| |||
work efficiency |
|
|
| X |
|
|
|
|
|
|
|
| |||
Continuous process of improving skills/capacity |
|
|
|
| X |
|
|
|
|
|
|
| |||
Skills\capacity standardization process |
|
|
|
| X |
|
|
|
|
|
|
| |||
Management capacity regulation |
|
|
|
| X |
|
|
|
|
|
|
| |||
Internal and external communication |
|
|
|
| X |
|
|
|
|
|
|
| |||
Efficient production, distribution and logistics |
|
|
|
| X |
|
|
|
|
|
|
| |||
effective information systems |
|
|
|
| X |
|
|
|
|
|
|
| |||
Coordination capacity |
|
|
|
| X |
|
|
|
|
|
|
| |||
Improve resource exploitation |
|
|
|
|
| X |
|
|
|
|
|
| |||
Rate of rejected radiographic film Radiology |
|
|
|
|
|
| X | X |
|
|
|
| |||
Unplanned hospitalization after outpatient procedure |
|
|
|
|
|
| X | X |
|
|
|
| |||
Cross-match rate for transfusion |
|
|
|
|
|
| X | X |
|
|
|
| |||
Appropriate patient management |
|
|
|
|
|
| X |
|
|
|
|
| |||
Appropriate number of medications per diagnosis |
|
|
|
|
|
| X |
|
|
|
|
| |||
Publications & Research Results |
|
|
|
|
|
| X |
|
|
|
|
| |||
Number of discharges against medical opinion |
|
|
|
|
|
| X |
|
|
|
|
| |||
Compliance with clinical guidelines (consultants' credentials, sedation, and privacy maintenance) |
|
|
|
|
|
| X |
|
|
|
|
| |||
Hospital mortality rate |
|
|
|
|
|
| X |
|
|
|
|
| |||
Outpatient clinic per year per doctor |
|
|
|
|
|
|
|
|
| X |
|
| |||
Emergencies per year per physician |
|
|
|
|
|
|
|
|
| X |
|
| |||
Users admitted to hospital per year by physician |
|
|
|
|
|
|
|
|
| X |
|
| |||
net mortality rate |
|
|
|
|
|
|
|
|
|
| X |
| |||
After analyzing the indicators found in the different publications, it appears that there are a large number of indicators in this perspective (Table 4.7). However, it is possible to group some of them into five categories, as they are the ones that most relate to and contribute to increased customer satisfaction and cost reduction. As such, we built five groups of indicators, which we called “time”, highlighting “average length of stay” (Behrouzi & Ma'aram, 2019; Rahimi et al., 2018), “length of stay” (Chen et al., 2018). al., 2006; Yang & Tung, 2006; Gordon et al., 1998) and “waiting time in the emergency room” (Rahimi et al., 2018); “Satisfaction” and where we have, as an example of indicators, “professional satisfaction index” (Behrouzi & Ma'aram, 2019; Chen et al., 2006) and “discharge with satisfaction with the care provided” (Rahimi et al., 2018); “Incidents” and in this group we have gathered all indicators that may be related to critical incidents and failures, such as “medical error rate” (Behrouzi & Ma'aram, 2019; Rahimi et al., 2018), “incidents with the reaction to blood transfusions”, “number of adverse events” (Rabbani et al., 2011; Rabbani et al., 2010) and “complication rate” (Gordon et al., 1998); “Professionals” and in this category we include all indicators that are related to the teams, namely, “retention rate” and “professional absenteeism rate” (Behrouzi & Ma'aram, 2019), as well as “professional turnover” (Chen et al., 2006). It is curious to use the indicator “professional satisfaction index” (Behrouzi & Ma'aram, 2019; Chen et al., 2006), as it usually appears in the learning and knowledge perspective. One of the reasons can be linked to the attempt to capture productivity.
Finally, the last category elaborated was called “Occupation” and, as an example of key indicators, we have “occupancy of beds” (Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Chen et al., 2006).; Yang & Tung 2006) and the “bed availability index” (Behrouzi & Ma'aram, 2019).
In addition to the indicators included in the five previous categories, there are many others (as can be seen in Table 4.7) that are part of this perspective and are equally important, since, depending on the reality of each Hospital Unit, it will identify which are the critical processes with a view to achievement of its objectives and then it will define which indicators are most appropriate to achieve its mission, whether it is more profit-oriented or user satisfaction.
It is always important to see this perspective as a piece of a puzzle, which has a previous perspective behind it and will “pave the way” to the next perspective.
The “Learning and Knowledge” perspective is the one that serves as the basis for achieving the objectives of the other perspectives. In a context that is constantly changing, such as that of health, this perspective is particularly important, as it allows for the growth and learning of teams so that they can carry out processes efficiently and effectively, contributing to user satisfaction and sustainability. organizations' finances.
Of the 24 studies analyzed, 14 focus on this perspective (see Table 4.4) and 10 define indicators (see Table 4.8; Martunis et al., 2020; Behrouzi & Ma'aram, 2019; Rahimi et al., 2018; Gao et al., 2019; Rahimi et al., 2018; Gao et al. al., 2018; Lin et al., 2013; Koumpouros, 2013; Chang et al., 2008; Chen et al., 2006; Yang & Tung, 2006; Gordon et al., 1998). The remaining four studies, Smith and Loonam (2016) and Verzola et al. (2009) do not define indicators; Rabbani et al. (2010) and Schmidt et al. (2006) mention this perspective, but adapt it to their reality, so they will be analyzed later.
Analyzing Table 4.8, we conclude that the indicators related to training and education are the most discussed in this perspective, which consolidates what was said at the beginning of the paragraph, that is, that training is the basis for the success of teams.
Among the indicators related to training and research, we can mention some that deserve to be highlighted, namely “training and education frequency” (Martunis et al., 2020); “% of trained professionals” (Behrouzi & Ma'aram, 2019); “average training time for professionals” (Behrouzi & Ma'aram, 2019); “per capita training expenditure” (Rahimi et al., 2018); “expenditure on medical research” (Chen et al., 2006); “number of published articles” (Lin et al., 2013; Chang et al., 2008; Chen et al., 2006).
Another indicator worth mentioning, which was used in three studies (Martunis et al., 2020; Rahimi et al., 2018; Lin et al., 2013), is “the satisfaction rate of professionals”. The importance of this indicator is easily understood, as it represents a fundamental element in the search for the success of an institution. It would also be important to analyze this indicator simultaneously with the indicator “turnover of staff”, as is done in the study by Rahimi et al. (2018), as it would facilitate the understanding between the degree of satisfaction and the turnover of teams.
Table 4. 8 – Indicators of the Learning and Knowledge perspective (referring to the studies that included this perspective)
| Martunis et al., (2020) | Behrouzi & Ma'aram (2019) | Rahimi et al., (2018) | Gao et al., (2018) | Lin et al., (2013) |
Koumpouros (2013) | Chang et al., (2008) | Chen et al., (2006) |
Yang & Tung (2006) | Gordon et al., (1998) | ||
| INDICATORS | |||||||||||
LEARNING AND KNOWLEDGE | Professional satisfaction rate | X |
| X |
| X |
|
|
|
|
| |
Training and Research | Frequency of training and education | X |
|
|
|
|
|
|
|
|
| |
% of trained professionals |
| X |
|
|
|
|
|
|
|
| ||
% of training hours for culture training |
| X |
|
|
|
|
|
|
|
| ||
Average training time of professionals |
| X |
|
|
|
|
|
|
|
| ||
Expenditure on training per capita |
|
| X |
|
|
|
|
|
|
| ||
advanced studies |
|
|
| X |
|
|
|
|
|
| ||
Number of seminars on a topic and search results |
|
|
|
| X |
|
|
|
|
| ||
Number of published articles |
|
|
|
| X |
|
|
|
|
| ||
Training of professionals and management knowledge |
|
|
|
| X |
|
|
|
|
| ||
Medical research expenses |
|
|
|
|
|
|
| X |
|
| ||
Scientific articles written in English per year (written by Health professionals) |
|
|
|
|
|
|
| X |
|
| ||
Clinical studies in patients |
|
|
|
|
|
|
|
|
| X | ||
Number of research projects |
|
|
|
|
|
| X |
|
|
| ||
Number of SCI articles |
|
|
|
|
|
| X |
|
|
| ||
Qualification |
|
|
|
|
| X |
|
|
|
| ||
Investment in Technology | % of the budget allocated to the purchase of technology |
| X |
|
|
|
|
|
|
|
| |
% of the budget allocated to information technologies |
| X |
|
|
|
|
|
|
|
| ||
Ability to apply computerized systems |
|
|
|
| X |
|
|
|
|
| ||
Organizational environment | Employee absenteeism rate |
|
| X |
|
|
|
|
|
|
| |
staff turnover |
|
| X |
|
|
|
|
|
|
| ||
Internal communication |
|
|
|
| X |
|
|
|
|
| ||
Employ and retain competent personnel |
|
|
|
| X |
|
|
|
|
| ||
Team work |
|
|
|
| X |
|
|
|
|
| ||
staff structure |
|
|
| X |
|
|
|
|
|
| ||
outpatient activity |
|
|
|
|
|
|
| X |
|
| ||
Formulation of the mission and vision |
|
|
|
|
|
|
|
| X |
| ||
Implementation of strategic analysis |
|
|
|
|
|
|
|
| X |
| ||
Management by objectives |
|
|
|
|
|
|
|
| X |
| ||
market comparison |
|
|
|
|
|
|
|
| X |
| ||
learning organization |
|
|
|
|
|
|
|
| X |
| ||
BSC |
|
|
|
|
|
|
|
| X |
| ||
ISO certification |
|
|
|
|
|
|
|
| X |
| ||
Participation in the TQIP |
|
|
|
|
|
|
|
| X |
| ||
Admission day procedures |
|
|
|
|
|
|
|
|
| X | ||
Goals focused on patient care |
|
|
|
|
|
|
|
|
| X | ||
Number of research projects |
|
|
|
|
|
| X |
|
|
| ||
Once again, we mention that all indicators assume their importance and that this will always depend on the organization's focus and the direction taken by the stakeholders in the BSC implementation process.
In addition to the four traditional perspectives, through which the BSC became known, there are authors who chose to build new perspectives (Table 4.9 and 4.10), in order to better satisfy the objectives of their studies. In Table 4.9, we present the indicators related to specific perspectives in the health area and, in Table 4.10 we present the indicators referring to other perspectives
Table 4. 9 - Indicators related to specific perspectives in the health area
| Martunis et al., (2020) |
Weiss & Downar (2013) |
Chen, Hou & Chang (2012) |
El-Jardali et al., (2011) |
Rabbani et al., (2011) |
Rabbani et al., (2010) |
Qudrat-Ullah, Chow & Goh (2007) |
Pink et al., (2001) | ||
| INDICATORS | |||||||||
Best Patient Experience | User recommendation rate | X |
|
|
|
|
|
|
| |
Mortality rate | X |
|
|
|
|
|
|
| ||
infection rate | X |
|
|
|
|
|
|
| ||
Waiting time | X |
|
|
|
|
|
|
| ||
Standby Time ED P4R(?) | X |
|
|
|
|
|
|
| ||
Transition and Continuity | X |
|
|
|
|
|
|
| ||
Alternate level of care (ALC) | X |
|
|
|
|
|
|
| ||
Days over the province 50% lite (LOS) | X |
|
|
|
|
|
|
| ||
hand hygiene | X |
|
|
|
|
|
|
| ||
Critical Incidents | X |
|
|
|
|
|
|
| ||
admission performance | Average length of stay |
|
| X |
|
|
|
|
| |
Occupancy rate (%) |
|
| X |
|
|
|
|
| ||
Bed turnover rate |
|
| X |
|
|
|
|
| ||
quality of care | Infection rate (%) |
|
| X |
|
|
|
|
| |
Rate of unscheduled readmissions (%) |
|
| X |
|
|
|
|
| ||
Hospital accident rate (%) |
|
| X |
|
|
|
|
| ||
Useclinic and results | Mortality inpatients |
|
|
| X |
|
|
|
| |
Readmission for the same diagnosis |
|
|
| X |
|
|
| X | ||
Repeated surgical procedures |
|
|
| X |
|
|
|
| ||
patient falls |
|
|
| X |
|
|
|
| ||
medical errors |
|
|
| X |
|
|
|
| ||
Cesarean |
|
|
| X |
|
|
|
| ||
medication errors |
|
|
| X |
|
|
|
| ||
length of stay |
|
|
| X |
|
|
| X | ||
complications |
|
|
|
|
|
|
| X | ||
% of surgeries/day |
|
|
|
|
|
|
| X | ||
Used diagnostic technology |
|
|
|
|
|
|
| X | ||
User satisfaction | User satisfaction |
|
|
| X |
|
|
|
| |
Satisfaction with the medical team |
|
|
|
| X | X |
| X | ||
Satisfaction with the nursing team |
|
|
|
| X | X |
| X | ||
Complaints from users |
|
|
|
| X | X |
|
| ||
Proportion of users who would recommend the hospital to others |
|
|
|
| X | X |
|
| ||
global quality |
|
|
|
|
|
|
| X | ||
Quality Process |
|
|
|
|
|
|
| X | ||
Results |
|
|
|
|
|
|
| X | ||
Satisfaction with Support Services |
|
|
|
|
|
|
| X | ||
Satisfaction with Cleaning Services |
|
|
|
|
|
|
| X | ||
Satisfaction with assisting staff in patient care |
|
|
|
|
|
|
| X | ||
better indicators | Clinical re-intervention rate |
|
|
|
|
|
| X |
| |
phone access |
|
|
|
|
|
| X |
| ||
Service access |
|
|
|
|
|
| X |
| ||
Time to schedule a specialty appointment |
|
|
|
|
|
| X |
| ||
User-centric quality |
Safety | Clostridium difficile infection rate |
| X |
|
|
|
|
|
|
Pneumonia with ventilator use |
| X |
|
|
|
|
|
| ||
hand hygiene |
| X |
|
|
|
|
|
| ||
Infection at the puncture site |
| X |
|
|
|
|
|
| ||
pressure ulcer |
| X |
|
|
|
|
|
| ||
falls |
| X |
|
|
|
|
|
| ||
Efficiency | Standard hospital mortality ratio |
| X |
|
|
|
|
|
| |
Readmissions |
| X |
|
|
|
|
|
| ||
Alternative Care Level |
| X |
|
|
|
|
|
| ||
total margin |
| X |
|
|
|
|
|
| ||
Access | Emergency waiting time |
| X |
|
|
|
|
|
| |
Satisfaction | Willingness to recommend hospital services after the high |
| X |
|
|
|
|
|
| |
Regarding perspectives directly related to the health sector, these were found in eight of the analyzed publications (Martunis et al., 2020; Chen, Hou & Chang, 2012; El-Jardali et al., 2011, Rabbani et al., 2011; Rabbani et al., 2010; Qudrat-Ullah, Chow & Goh, 2007; Pink et al., 2001, Weiss & Downar, 2013).
As shown in Table 4.9, these perspectives were given the names “Best Patient Experience”, “Admission performance”, “Quality of care”, “Clinical use and results”, “User satisfaction”, “Better indicators” and “Quality centered on the user” include, above all, indicators that are related to users and the quality of care provided, fundamental aspects for any health organization to achieve success and high levels of performance.
With regard to other perspectives (see Table 4.10), these were developed in seven studies (Chen, Hou & Chang, 2012; El-Jardali et al., 2011, Rabbani et al., 2011; Rabbani et al., 2010; Qudrat-Ullah, Chow & Goh, 2007; Pink et al., 2001, Schmidt et al., 2006) and were dubbed “Administration”, “Integration Systems and Human Resources”, “Human Resources”, “Faster indicators”, “Cheaper indicators”, “Clinical Risk”, “Modernization” and “Workforce”. Analyzing the indicators used in each of these “new” perspectives, it is easy to see that, contrary to the indicators found in Table 4.9, these are not directly related to the user, but to all back-office work and professionals. Making a parallel with traditional perspectives, while the perspectives mentioned in Table 4.9 are close to the Customers perspective, those presented in Table 4.10 are more related to the remaining perspectives (Financial, Internal Processes and Learning and Knowledge). We understand, therefore, that it may be an attempt to innovate and adapt the BSC to the new reality that is experienced within health organizations.
According to Rahimi et al. (2018) the “Internal Processes” perspective is the one that assumes the central role in terms of perspectives, being the one that most interrelates with the others; the “Learning and Knowledge” perspective is the one that most influences the others, while the “Customers” perspective is the one that receives the greatest influence from the others. In turn, and according to the same authors, the “Financial” perspective is neither the “main effect factor” nor the “main cause”, nor does it have a central role. In terms of indicators, these authors concluded that the one that assumes a central role is the indicator “occupancy of beds”; the indicator “clinical errors” is the one that most affects the other indicators, while the most affected is “% of user satisfaction”.
Table 4. 10 - Indicators referring to other perspectives
|
Chen, Hou & Chang (2012) |
El-Jardali et al., (2011) |
Rabbani et al., (2011) |
Rabbani et al., (2010) |
Qudrat-Ullah, Chow & Goh (2007) |
Schmidt et al., (2006) |
Pink et al., (2001) | |
| INDICATORS | |||||||
Management |
% of complete medical records |
X |
|
|
|
|
|
|
Rate of prompt consultation (%) |
X |
|
|
|
|
|
| |
Integration Systems and Human Resources | surgical infections |
| X |
|
|
|
|
|
Needle or sharp injuries |
| X |
|
|
|
|
| |
personal turnover |
| X |
|
|
|
|
| |
Personal satisfaction |
| X |
|
|
|
|
| |
Waiting time from ER to bed assignment |
| X |
|
|
|
|
| |
ER waiting time |
| X |
|
|
|
|
| |
absence of staff |
| X |
|
|
|
|
| |
Staff sick leave fee |
| X |
|
|
|
|
| |
% of transfers to another hospital |
| X |
|
|
|
|
| |
Clinical Information Technology |
|
|
|
|
|
| X | |
Collection, dissemination and clinical benchmarking |
|
|
|
|
|
| X | |
Intensity of use of information |
|
|
|
|
|
| X | |
Development and use of clinical pathways |
|
|
|
|
|
| X | |
care coordination |
|
|
|
|
|
| X | |
community integration |
|
|
|
|
|
| X | |
Strategy to manage users in LAC |
|
|
|
|
|
| X | |
Human Resources | job satisfaction |
|
| X | X |
|
|
|
Satisfaction with colleagues |
|
| X | X |
|
|
| |
Satisfaction with the facilities |
|
| X | X |
|
|
| |
Satisfaction with the organization |
|
| X | X |
|
|
| |
Satisfaction with Supervisors |
|
| X | X |
|
|
| |
Faster indicators | Total turnover time |
|
|
|
| X |
|
|
Total Turnaround time |
|
|
|
| X |
|
| |
External referral rate of patients |
|
|
|
| X |
|
| |
Cheaper Indicators |
Average amount of expense |
|
|
|
|
X |
|
|
Average length of stay |
|
|
|
|
X |
|
| |
Clinical Risk | Results (Health of nation outcome scales, Royal College of Psychiatrists) |
|
|
|
|
| X |
|
Average 3-year suicide rate for mentally ill and high |
|
|
|
|
| X |
| |
% of complaints where response within 20 days |
|
|
|
|
| X |
| |
falls |
|
|
|
|
| X |
| |
modernization | Assertive disclosure of the number of cases by the team |
|
|
|
|
| X |
|
Service users who have received crisis resolution services |
|
|
|
|
| X |
| |
Number of cases with early intervention |
|
|
|
|
| X |
| |
Service users who waited >21 weeks for a first appointment (consultant |
|
|
|
|
| X |
| |
Service users whose transfer to adult service care is delayed |
|
|
|
|
| X |
| |
Service users whose transfer to geriatric service care is delayed |
|
|
|
|
| X |
| |
Occupancy of beds in the hospitalization of adults, without discharge to the home |
|
|
|
|
| X |
| |
Occupancy of beds in geriatric hospitalization, without discharge home |
|
|
|
|
| X |
| |
Placements outside the area |
|
|
|
|
| X |
| |
Caregivers with an active care plan |
|
|
|
|
| X |
| |
Workforce | Sick leave |
|
|
|
|
| X |
|
overtime |
|
|
|
|
| X |
| |
turnover |
|
|
|
|
| X |
| |
% of staff trained |
|
|
|
|
| X |
| |
Gao et al., (2018) report that the indicator system developed demonstrated good validity and reliability; that the first level indicators show the following order: Financial > Internal Processes > Customers > Learning and Knowledge, with the financial perspective being the first to be considered; in the correlation between the Internal Processes, Customers and Financial perspectives, it is the first that has greater weight, due to the need to guarantee quality in health services. It can thus be seen that the Customers perspective is affected by the Internal Processes perspective. In this study, the perspective that proved to be less relevant is the Learning and Knowledge perspective, perhaps because the focus of the hospitals covered by the study is more directed to practical work, rather than scientific research or teaching.
Yang and Tung (2006) reinforce that the BSC reflects causal relationships between the four perspectives. The results obtained support the hypothesis that organizational learning has a positive influence on quality, quality has a positive influence on profit, efficiency has a positive influence on market share and profit. However, the results obtained did not support the hypothesis that user satisfaction has a positive influence on market share, nor that market share has a positive influence on profit. The results obtained in the Learning and Knowledge and Internal Processes perspectives showed a direct effect on the financial indicators. They also found that, with the implementation of this tool, the medical quality affected the efficiency, a low net mortality in 2001 resulted in a significantly higher return on assets (ROA) in 2002, a significantly higher load factor led to greater market share the following year. As such, efficiency had a positive influence on financial performance. User satisfaction is significantly associated with profit, but there is a negative relationship between customer satisfaction and market share, no relationship was found between market share and profit.
Although there is no uniformity in terms of the relevance of perspectives, once again the importance that the financial perspective assumes, as well as the Learning and Knowledge perspective, is perceptible. It should be noted that the perspectives establish cause and effect relationships among themselves, where a good foundation will be an essential pillar for the achievement of the Hospital Unit's mission.
Question 6: What are the facilitating factors in the design and implementation of the BSC?
Since the BSC is a tool that contributes to the improvement of the performance of health organizations, where all elements of the organization must understand/realize their role in achieving this objective, it is important to understand which elements are considered as facilitators of this process in the analysed publications.
Of the 24 studies, only seven refer to facilitating elements. It is these studies that we discuss next.
Koumpouros (2013) points out, as facilitating elements for the design and implementation of the BSC, the constant flow of information and the participation of a group of customers, as a support element for the project. This author also mentions that constant communication and information are the key to the success of this process, because they increase familiarity with it, as resistance decreases and confidence in its success increases.
In the study carried out by Rabbani et al. (2010), they state that the design of the BSC was possible because most of the necessary prerequisites for a successful design and implementation (leadership, strategic plans and viable information systems) were already being used, and the readiness for the use of the BSC had already been evaluated previously. This seems to be a good principle to assume in the design and implementation of this tool, that is, ensuring that these three requirements are met, because as these authors mention, it will facilitate the process of development and implementation of the same. Also, Rabbani et al. (2011), mention that the support of the organization in terms of financial and non-financial benefits, previous experience with Quality Care initiatives,
Following on from the facilitating elements, Smith and Loonam (2016) leave some recommendations of which we highlight the following: formal support from top management, existence of an educational plan and a communication process that includes all the staff, the importance of standardization of procedures, the teams involved must include staff at all levels, so that all department employees are involved in at least one initiative.
In turn, Pink et al. (2001), stresses that data quality must be guaranteed; data must be presented carefully and in an understandable format; advisory committees should include hospital researchers, managers and clinicians; build links with the data; carefully consider the disclosure of information and variations in the way in which resources are allocated.
Also mentioned as facilitating elements are the participation of the members of the Board of Directors in the BSC executive team, the implementation of the scorecard at the organizational level in the most relevant departments, and the open presentation of results (Chang et al., 2008).
In the study carried out by Chen et al. (2006), he points out as facilitating elements of the BSC implementation process, the selection of Key Performance Indicator (KPI's) suitable for the hospitals involved in the study.
Looking at the elements pointed out as facilitators in the different publications, it is clear that open communication, the dissemination of results and the involvement of top managers, contribute to the success in the design and implementation of this tool. The acceptance of the BSC by the different employees depends on their level of knowledge regarding the organization's strategic plan, as well as their involvement with the organizational objectives. Top management and its involvement in the process play a fundamental role in the dissemination of the strategic plan, as the perception by other employees of this situation facilitates the acceptance of this tool, as well as facilitating strategic alignment.
According to the different publications analysed, it can be concluded that the involvement of leaders is important not only in financial terms, but also in non-financial terms, as it encourages teams and facilitates the dissemination of results, thus contributing to for increased motivation that will lead to success.
Question 7: What are the results obtained with the implementation of the BSC?
To answer this question, we chose to look for information throughout the publications regarding three points: main conclusions, benefits, and less positive aspects resulting from the study/implementation of the BSC.
Although not all studies refer to the benefits obtained with the study/implementation of the BSC, most refer to the advantages associated with the use of indicators. For Behrouzi and Ma'aram (2019) the great advantage in the design and implementation of the BSC was that the literature review, which preceded this exercise, allowed the identification of a set of commonly used indicators, helping health care managers to identify the indicators most appropriate for their hospitals. Chen, Hou and Chang (2012), point out as a benefit the fact that the “red light warning system” associated with the BSC serves as an alert regarding the indicators that present the worst performances. It can be said that one of the benefits is to contribute to the improvement of performance,
Koumpouros (2013) concludes that the implementation of the BSC is encouraging, even one year after its implementation. According to the author, with the application of this tool, the hospital completed structural and electromechanical projects that had been in progress for almost ten years. The results support the idea that the adoption of management control systems is not only a function of a rational decision-making process and institutional pressures, but also depends on the characteristics of decision-makers. With the development of their study Chen, Hou and Chang (2012) conclude that this tool is appropriate for financial and administrative control in a hospital environment, where improvement depends on constant attention, while having a direct benefit on admission performance. For El-Jardali et al.
In summary, and still with regard to the benefits obtained with the implementation of the BSC, reported throughout the publications, we can point out the following:
- allows the implementation of new recommendations to hospitals (Gao et al.,
2018);
- offers an opportunity to aggregate the business strategy to the objectives assigned to each operating unit. In this way, the strategy can be communicated to all levels of the organization (Verzola et al., 2009), and the allocation of resources can reflect the strategic objectives (Verzola et al., 2009; Inamdar, Kaplan & Bower, 2002);
- it makes it easier to explain cause-effect relationships to clinicians, staff and users (Verzola et al., 2009);
- facilitates communication between different professionals, making it possible to reach a consensus on strategic priorities (Verzola et al., 2009);
- helps clarify strategy among managers (Verzola et al., 2009; Inamdar, Kaplan & Bower, 2002), and facilitates organizational alignment (Chang et al., 2008);
- it increases management credibility, making top management and other managers responsible (Chang et al., 2008; Inamdar, Kaplan & Bower, 2002);
- through the strategic map's cause-effect relationship, it can help managers balance short-term financial goals and long-term investments (Chang et al., 2008);
- through the four perspectives of the BSC, executives have a structure for decision making (Inamdar, Kaplan & Bower, 2002);
- defines priorities to identify, rationalize and align initiatives (Inamdar, Kaplan & Bower, 2002);
- supports greater responsibility, especially when linked to managers' incentive plans (Inamdar, Kaplan & Bower, 2002);
- provides continuous learning and improvement (Chang et al., 2008; Inamdar, Kaplan & Bower, 2002);
- allows telling the story of the organization’s strategy (Inamdar, Kaplan & Bower, 2002);
- it guides its implementation, offering a timeline and forward-looking indicators, and cause-effect relationships that capture the complexity and interrelationships of the strategy (Inamdar, Kaplan & Bower, 2002);
- the indicator system development process helps management teams to define relevant strategic objectives (Gordon et al., 1998);
- facilitates a common understanding of unit objectives (Gordon et al., 1998).
From the above, it is clear that there is a clear identification of the benefits that the implementation of this tool can bring to the performance of an organization, thus improving its effectiveness and efficiency. On the other hand, when we look for fewer positive aspects resulting from the implementation of the BSC, only one of the publications mentions negative aspects, which, in our opinion, can be easily circumvented, they are: work overload and absence of information systems capable of to respond to the BSC effectively (Verzola et al., 2009). As a way of circumventing these obstacles, it is important that, when implementing this tool, there is a correct allocation of human resources, the information systems are adequate and there is a good internal communication system.
In the following paragraphs, we will present the main conclusions reached in the different studies.
For Verzola et al. (2009) the BSC is an ideal point of contact between the financial and clinical dimensions of administration, they point out that the rapid diffusion of the BSC among the main international for-profit and non-profit organizations is proof of its great potential, and that this project can be viewed as a preparatory phase in the strategic analysis of a subsequent business plan.
Naranjo-Gil (2009) with his study concludes that younger nurses with more positions use the BSC in a more interactive way, contrary to older nurses with fewer positions, who only use this tool of diagnostic form; most nurse managers use non-financial indicators; the use of the BSC facilitates nurse managers to achieve strategic performance based on costs, as well as strategic objectives focused on quality and flexibility.
According to the results obtained by Chang et al. (2008), the implementation of the BSC led to an increase in revenue, user satisfaction, an increase in the number of visits from disadvantaged groups, an increase in the number of clients admitted to intensive care units in less than three hours, coming directly from the emergency department. , decreased waiting time for antibiotic prescription consultation and increased number of scientific publications and research projects. These authors also refer that the comprehensive process of implementing the BSC is an excellent strategic and performance system, and that, in turn, the gradual process, from the beginning of the BSC at the hospital level to the subsequent implementation of the BSC at the department, increased understanding of this tool by different professionals,
Another of the conclusions to be highlighted is mentioned by Qudrat-Ullah, Chow & Goh (2007), who emphasize that using the qualitative structure of the BSC, they identified the need for decision systems that are sufficiently robust to incorporate better knowledge of the external environment in the internal hospital processes and to develop broader knowledge of organizational performance by identifying areas that have not received as much attention (particularly procedures and methods to improve feedback and learning in various dimensions).
The study by Chen et al. (2006) raises the question that although this tool can bring significant benefits to the organization, its success may also depend on cultural aspects. These authors addressed the implementation of the BSC in hospitals in China and Japan, however one of the countries presents better results than the other.
Although the different studies refer to the implementation of the BSC in the health sector, they all had different objectives, however, it is clear that all of them reveal the fact that the BSC is a tool that helps to improve performance. hospital, either individually or complemented with other management tools.
Summarizing the information collected in the answer to this question, it is noticeable that one of the great advantages of the design and implementation of the BSC is to contribute to the improvement of the performance of Hospital Units. As an example of this, we highlight the results obtained by Meliones et al. (2008), where they report that with the implementation of the BSC, and when compared to the previous year, there is a reduction in morbidity, a decrease in readmissions from 7% to 4%, a decrease in infection rates from 3% to 1 %, a decrease in length of stay of 0.6 days, the team achieved a flow of users of 26% improvement in discharge times and 10% improvement in the Pediatric Intensive Care Unit; an increase in contributory margin by 240% and an improvement in net margin that went from losses of $4.7 million per year in 2004, to a total of $7.
Question 8: What are the difficulties and/or limitations of implementing the BSC?
From the analysis of publications, there are several difficulties and/or limitations mentioned by the authors of the studies (see Table 4.11). Of all of them, the one that is repeated in the largest number of studies is the difficulty in accessing information, namely access to targets, initiatives and strategic plans. It then presents a greater number of references, the lack of collaboration with researchers, whether this lack of collaboration on the part of Top Management, or on the part of health professionals, which is felt at the level of approval, availability and commitment. towards the BSC implementation process. The commitment of organizational leaders is fundamental, both in terms of access to information and internal communication within the institution, thus facilitating
Table 4. 11 - Difficulties and/or Limitations to BSC Implementation
| Behrouzi & Ma'aram (2019) | Gao et al., (2018) | Koumpouros (2013) | El-Jardali et al., (2011) | Rabbani et al., (2011) | Rabbani et al., (2010) | Verzola et al., (2009) | Meliones et al., (2008) | Chen et al., (2006) | Yang & Tung (2006) | Inamdar, Kaplan & Bower (2002) | Pink et al., (2001) | Gordon et al., (1998) | ||
Difficulties and/or Limitations | Access to information | X |
|
|
|
| X | X |
| X |
|
|
| X | |
Low collaboration with investigators (approval, availability and commitment) | X |
|
|
|
|
|
|
|
|
| X |
| X | ||
limited human resources |
|
|
| X | X |
|
|
|
|
|
|
|
| ||
Large number of indicators can lead to difficulties in implementing performance evaluation systems in terms of cost and efficiency |
|
X |
|
|
|
|
|
|
|
|
|
|
| ||
Resistance to change |
|
| X |
|
|
|
|
|
|
|
|
|
| ||
not believe in success |
|
| X |
|
|
|
|
|
|
|
|
|
| ||
Amount of clinical work |
|
|
|
| X |
|
|
|
|
|
|
|
| ||
Difficulty choosing or defining reference standards |
|
|
|
|
|
| X |
|
|
|
|
|
| ||
Selection of effective KPI's |
|
|
|
|
|
|
|
| X |
|
|
|
| ||
Data | Data obtained through questionnaires self-administered |
|
|
|
|
|
|
|
|
| X |
|
|
| |
Absence of data that assess the depth of implementation |
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Time interval between data collection clinical and financial and the collection of the remaining data |
|
|
|
|
|
|
|
|
|
|
|
X |
| ||
Obtain and interpret data in a timely and cost-effective manner |
|
|
|
|
|
|
|
|
| X |
|
|
| ||
Lack of in-depth analysis of data outcome |
|
|
|
|
| X |
|
|
|
|
|
|
| ||
Difficulty in developing initiatives aimed at the institutions' objectives based on the strategic plan. |
|
|
|
|
|
|
| X |
|
|
|
|
| ||
Difficulty removing confounders |
|
|
|
|
|
|
| X |
|
|
|
|
| ||
Extend the BSC to the entire organization |
|
|
|
|
|
|
|
|
|
| X |
|
| ||
Keep the BSC simple and use it for learning |
|
|
|
|
|
|
|
|
|
| X |
|
| ||
Lack of knowledge about BSC and Management |
|
| X |
|
|
|
|
|
|
|
|
|
| ||
Quality | Absence of a quality culture in hospitals |
|
|
| X |
|
|
|
|
|
|
|
|
| |
Absence of a quality department in the hospitals |
|
|
| X |
|
|
|
|
|
|
|
|
| ||
Physician resistance to performance measurement and reporting |
|
|
| X |
|
|
|
|
|
|
|
| X | ||
Lack of competent personnel in the measurement and interpretation of data |
|
|
| X |
|
|
|
|
|
|
|
|
| ||
Lack of national performance management initiatives to provide benchmarking |
|
|
|
| X |
|
|
|
|
|
|
|
| ||
Inability of leadership to communicate a clear BSC agenda |
|
|
|
| X |
|
|
|
|
|
|
|
| ||
Poorly defined staff roles in BSC implementation. |
|
|
|
| X |
|
|
|
|
|
|
|
| ||
The scarcity of human resources is also mentioned in two publications (El-Jardali et al., 2011; Rabbani et al., 2011) as a difficulty/limitation to the design and implementation of this tool. It can be seen that excess work (Rabbani et al., 2011), as a result of limited human resources, makes collaboration in this process difficult (El-Jardali et al., 2011; Gordon et al., 1998).
Pink et al. (2001) argue that it is important to guarantee the quality of the data and that they must be presented carefully and in an understandable format, as such, and to highlight this aspect, we considered it pertinent to group the different difficulties/limitations that are related to the data, which included the following difficulties/limitations: the way of obtaining data (Yang & Tung, 2006), lack of data that assess the depth of implementation of new management activities, human capital, and information in the Learning and Knowledge perspective (Yang & Tung, 2006), the timing to collect the data (Pink et al., 2001; Inamdar, Kaplan & Bower, 2002) and lack of in-depth analysis of the outcome of the data (Rabbani et al., 2010). Inamdar, Kaplan and Bower (2002), and Pink et al., (2001),
As an example of other difficulties/limitations pointed out, we have the high number of indicators (Gao et al., 2018), resistance to change (Koumpouros, 2013), which is closely associated with the lack of knowledge about BSC and Management (Koumpouros, 2013), o not believing in success, nor in the benefits that the implementation of this tool can bring (Koumpouros, 2013), absence of a quality culture (El-Jardali et al., 2011), poorly defined roles (Rabbani et al., 2011), lack of initiatives that allow comparisons between different hospitals (Rabbani et al., 2011), inability of leaders to communicate a clear agenda (Rabbani et al., 2011), adequate selection of KPIs (Chen et al., 2006), the difficulty of extending the BSC to all departments of the organization (Inamdar, Kaplan & Bower, 2002),the difficulty in removing confounding factors (Meliones et al., 2008), and the difficulty in keeping the BSC simple and using it as a learning element (Inamdar, Kaplan & Bower, 2002).
Of all the difficulties/limitations pointed out, there are three that we would like to reflect on in more detail: adequate selection of indicators, resistance to change and the lack of top-down communication.
Regarding the selection of indicators, as stated by Kaplan and Norton (2000), it is important not to present too many indicators, and those selected should focus on complementing the strategy. In other words, it is important that the indicators are not too many, and that they represent exactly what we want from them.
The resistance of health professionals is often related to a lack of knowledge about this tool, which can be overcome with the use of training and clarification sessions. Many of the difficulties/limitations felt could disappear, only with recourse to training and the existence of BSC experts in the implementation teams.
Another point that, in our opinion, deserves to be highlighted is the lack of top-down communication. If organizations had a good internal communication system, many of the aforementioned obstacles would disappear. Understanding the difficulties and limitations felt by other authors will be a step towards success.
It is important to identify the difficulties/limitations felt so that, in future investigations, they can be circumvented, thus avoiding the failure of this tool. Many of them can be solved with the promotion of training on this tool and on the successful results that can be achieved, when properly implemented. Experts in the BSC should be part of the work team, who play a fundamental role throughout the process in overcoming some difficulties felt, namely, in the reorientation and adequacy of the focus, as well as in the clarification of any doubts that may arise.
Question 9: What opportunities are there for future investigations in this area?
After analyzing the publications and collecting information about the BSC implementation process, it also seemed important to identify opportunities for future investigations, left as suggestions by the authors of these publications and our own reflection on the implementation of this tool in Hospital Units.
Throughout the 24 publications, we can highlight the following as suggestions for future investigations/studies:
- Cover more BSC elements as targets and initiatives (Behrouzi & Ma'aram, 2019);
- Apply this tool to other hospitals, to different types of hospitals (eg pediatric hospitals, maternity hospitals, etc.) (Gao et al., 2018), and within hospitals, to different hospital departments (Gao et al., 2018; Koumpouros, 2013);
- Comparing the BSC with performance evaluation methods such as the
- Comprehsive Index Methodand the Rank Sum Ratio Method (Gao et al., 2018);
- Develop and run empirical tests together with other tools present in the academic literature (Porporato, Tsasis & Marin, 2017);
- Conduct a longitudinal study to assess whether the BSC is an effective tool in supporting an execution strategy in healthcare (Smith & Loonam, 2016);
- Generalize the results to other hospitals and public sectors (Lin et al.,
- 2013);
- Carry out a comparative assessment between the different hospitals that are using the BSC to identify possible influences on the results obtained (El-Jardali et al., 2011);
- Track contexts over a longer period of time, to assess the impact of PGF or alternative strategy change frameworks on various organizations, with the construction of a theoretical explanation (Rabbani et al., 2011);
- Test the application of the BSC following a bottom-up strategy, ie, start by customizing the BSC for individual use in clinical departments and then implementing the system at an executive level (Rabbani et al., 2010);
- Analyze whether the use of objective versus subjective performance measures contributes to management attitudes, such as fairness, clarity of objectives and equity in the organization (Naranjo-Gil, 2009);
- Analyze whether the balance between internal and external constituents of the organization affects equity (Naranjo-Gil, 2009).
- Test causal relationships between different perspectives (Yang & Tung, 2006; Pink et al., 2001).
Based on the reflection made during this process, it seems to us that an interesting research opportunity is to explore opportunities to complement the BSC using other management tools. There are already reports that this complementarity can contribute to the construction of more effective BSC. Rabbani et al. (2010), for example, found that the Delphi process used in the design of the BSC allows, successfully incorporating the perspectives of health professionals and experts in the development of the BSC, a pragmatic interpretation of existing data, which facilitates the design of a scorecard with comprehensive indicators in multiple dimensions. Also, Rahimi et al. (2018), when discussing the possibility of helping the design and implementation of the BSC with the use of other methods, verified that the use of the DEMATEL method (Decision Making Trial and Evaluation Laboratory) can prove useful to establish relationships between key indicators. Other authors who propose the complementarity of the BSC with other tools are Lin et al. (2013), who suggest the integration of “fuzzy linguistics” with the BSC, in order to evaluate the performance of the Operating Room. This method has the advantage that performance indicators can be clearly identified and expressed quantitatively. Also, Schmidt et al. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. can prove useful to establish relationships between key indicators. Other authors who propose the complementarity of the BSC with other tools are Lin et al. (2013), who suggest the integration of “fuzzy linguistics” with the BSC, in order to evaluate the performance of the Operating Room. This method has the advantage that performance indicators can be clearly identified and expressed quantitatively. Also, Schmidt et al. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. can prove useful to establish relationships between key indicators. Other authors who propose the complementarity of the BSC with other tools are Lin et al. (2013), who suggest the integration of “fuzzy linguistics” with the BSC, in order to evaluate the performance of the Operating Room. This method has the advantage that performance indicators can be clearly identified and expressed quantitatively. Also, Schmidt et al. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. (2013), who suggest the integration of “fuzzy linguistics” with the BSC, in order to evaluate the performance of the Operating Room. This method has the advantage that performance indicators can be clearly identified and expressed quantitatively. Also, Schmidt et al. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. (2013), who suggest the integration of “fuzzy linguistics” with the BSC, in order to evaluate the performance of the Operating Room. This method has the advantage that performance indicators can be clearly identified and expressed quantitatively. Also, Schmidt et al. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process. (2006) turned to the BSC to develop an operational tool that includes strategic mapping, decision trees and RADAR logic. Together with the BSC, the RADAR logic proved to be a new opportunity to establish a structured action process.
Another model that can be explored is simulation, based on the existing qualitative framework. Once developed and calibrated for hospital-specific data, management can explore the impact of various strategies in order to optimize the hospital's existing but limited resources (Qudrat-Ullah, Chow & Goh, 2007).
Although the BSC has been the subject of greater research and investment in the health sector, it is clear from the suggestions left that there is still a long way to go, with a view to making this tool easier to implement. Only with standardized parameters can comparisons be made to assess the effectiveness of this tool in different contexts. The synthesis of this set of suggestions collected from the different publications analyzed, it comes, on the one hand, to prove the need for investment in this area, and, on the other hand, to offer some suggestions for future investigations in order to deepen the knowledge about this tool.
References
- Ahn, H. (2001) Applying the Balanced Scorecard Concept: An experience report. Long Range Planning, 34(4): 441-461.
- Al-Kaabi, S., Chehab, M. & Selim, N. (2019) The Balanced Scorecard as a Performance Management Tool in the Healthcare Sector – The Case of the Medical Commission Department at the Ministry of Public Health, Qatar. Cureus 11(7): e5262. DOI 10.7759/cureus.5262.
- Alvarez, L., Soler, A., Guiñón, L., & Mira, A. (2019). A Balanced Scorecard for assessing a strategic plan in a clinical laboratory. Biochemia medica: Biochemia medica, 29(2): 1-8.
- Alves, M. (2016) Balanced Scorecard for the general emergency service. Unpublished Master's Thesis, Instituto Superior de Contabilidade e Administração de Lisboa.
- Andrews, K. (1980) The Concept of Corporate Strategy. Pennsylvania, Third Edition. Aryani, Y., & Setiawan, D. (2020) Balanced Scorecard: Is It Beneficial Enough? THE Literature Review. Asian Journal of Accounting Perspectives, 13(1): 65-84.
- Atkinson, H. (2006) Strategy implementation: a role for the Balanced Scorecard? Management Decision, 44 (10): 1441-1460.
- Ba-abaad, K. (2009) Review of the literature of Balanced Scorecard and Performance measurement: the case of healthcare organizations. Business e-Builletin, 1(1): 33-47.
- Banza, E. (2013) Construction of a Balanced Scorecard for a strategic management of Centro Hospitalar Cova da Beira: Changing the management model to change the hospital. Unpublished Master's Dissertation, University of Beira Interior: Social and Human Sciences.
- Baraldi, S. (2002) The Balanced Scorecard in hospitals: performance measurement as a driver of change — a case study. In: Epstein, M. and Manzoni, J. (Ed.). Performance measurement and management control: a compendium of research. Oxford: Elsevier Science.
- Barbosa, C. & Perez, G. (2016) Implementation of the Balanced Scorecard in a Family Business in the Service Sector: A Case Study. Accounting Vista & Magazine, 27(1): 1-24.
- Barboza, L. (2011) The Balanced Use of Balanced Indicators, paper presented at the VII National Congress of Excellence in Management, August 12-14, 3013, Rio de Janeiro.
- Barcellos, P. (2002) Business Strategy in Schmidt, P. (org.) Controllership: adding value to the company. Porto Alegre, Bookman.
- Beer, M. & Eisenstat, R. (2000) The silent killers of strategy implementation and learning. Sloan Management Review, 41(4): 29-40.
- Behrouzi, F. & Ma'aram, A. (2019) Identification and ranking of specific Balanced Scorecard performance measures for hospitals: A case study of private hospitals in the Klang Valley area, Malaysia. The International Journal of Health Planning and Management 34 (4), 1364–1376.https://doi.org/10.1002/hpm.2799.
- Bittar, O. (2001) Indicators of quality and quantity in health. Journal of Health Administration, São Paulo, 3(12): 21-28.
- Bourguignon, A., Malleret, V. & Norreklit, H. (2004) The American Balanced Scorecard vs. the French Tableau de bord: the ideological dimension management. Accounting Research, 15(2): 107-134.
- Caldeira, J. (2010) Implementation of the Balanced Scorecard in the State: managing strategic performance to create public value. Coimbra, Almedina.
- Calhau, A. (2009) Design of a Balanced Scorecard system for the Traumatology Service of Hospital Garcia de Orta. Unpublished Master's Thesis, Institute of Accounting and Administration of Lisbon.
- Carvalho, F., Dias, L. & Prochnik, V. (2005) The Use of the Balanced Scorecard in hospitals: The Case of Hospital Nove de Julho, paper presented at the IX International Congress on Costs, “Cost Management in the Era of Knowledge Management”, 28-30 November, Florianópolis.
- Caudle, S. (2008) The Balanced Scorecard: A Strategic Tool in Implementing Homeland Security Strategies. Homeland Security Affairs, 4 (3): 1-17.
- Chang, W., Tung, Y., Huang, C. & Yang, M. (2008) Performance improvement after implementing the Balanced Scorecard: A large hospital's experience in Taiwan. Total Quality Management & Business Excellence, 19(11): 1143 –1154. https://doi.org/10.1080/14783360802323560.
- Chavan, M. (2009) The Balanced Scorecard: a new challenge. Journal of Management Development, 28(5): 393–406.
- Chen, H., Hou, Y. & Chang, R. (2012) Application of the Balanced Scorecard to an academic medical center in Taiwan: the effect of warning systems on improvement of hospital performance. Journal of the Chinese Medical Association, 75(10): 530–535. https://doi.org/10.1016/j.jcma.2012.07.007.
- Chen, X., Yamauchi, K., Kato, K., Nishimura, A. & Ito, K. (2006) Using the Balanced Scorecard to measure Chinese and Japanese hospital performance. International Journal of Health Care Quality Assurance, 19(4): 339–350. https://doi.org/10.1108/09526860610671391.
- Chow, C.,Ganulin, D.,Teknika, O.,Haddad, K.&Williamson J. (1998) The Balanced Scorecard: A Potent Tool for Energizing and Focusing Healthcare Organization Management. Journal of Healthcare Management, 43(3): 263-279.
- Collis, D. & Rukstad, M. (2008) Can you say what your strategy is? Harvard Business Review, 86(4): 82-90.
- Collins, J. & Porras, J. (1996) Building Your Company's Vision. Harvard Business Review, 74(5): 65-77.
- Corral, A. & Urieta, C. (2001) Nuevas Herramientas de Gestión Pública: El Quadro de Mando Integral. Madrid, Ortega Ediciones Gráficas.
- Cruz, I. (2005) The Balanced Scorecard and the Management of Hospital Organizations, paper presented at the XV Jornadas Hispano-Lusas de Gestión Científica, 2-4 February, Seville: 441-446.
- Cruz, L.; Geada, F. & Silva, T. (2012) Value Balanced Scorecard: a tool to achieve excellence. Lisbon, Sílabo Editions.
- Dias, V. (2014) Analysis of the implementation of the Balanced Scorecard tool in an EPE hospital. Master's thesis, ISCTE-IUL, Lisbon. Available at www:http://hdl.handle.net/10071/8603 (accessed October 10, 2019).
- Donato, H. & Donato, M. (2019) Stages in conducting a systematic review, Acta Médica Portuguesa, 32(3): 227-235.
- El-Jardali, F., Saleh, S., Ataya, N. & Jamal, D. (2011) Design, implementation and scaling up of the Balanced Scorecard for hospitals in Lebanon: Policy coherence and application lessons for low- and middle-income countries. Health Policy, 103(2-3): 305–314.https://doi.org/10.1016/j.healthpol.2011.05.006.
- Epstein, M. & Manzoni, J. (1998) Implementing corporate strategy: from Tableaux de Bord to Balanced Scorecards. European Management Journal, 16(2): 190-203.
- Ferreira, J. (2012) The Balanced Scorecard in performance evaluation: application in Bosch Security Systems. Unpublished Master's Thesis, Instituto Universitário de Lisboa. Available at www:http://hdl.handle.net/10071/4634 (accessed June 10, 2019).
- Freire, A. (1997) Strategy: Success in Portugal. Lisbon, Editorial Verbo.
- Freitas, C. (2015) Application of the Balanced Scorecard methodology to a cardiology service of a public hospital. Unpublished Master's Thesis, Faculty of Economics, Porto. Available inhttps://comum.rcaap.pt/ (accessed on June 04, 2019).
- Gallon, A., Nascimento, S., Ensslin, S., Ensslin, L. & Dutra, A. (2008) Mapping of management tools for performance evaluation disseminated in engineering research. Revista R&D in Production Engineering, 7: 53-72.
- Gao, H., Chen, H., Feng, J., Qin, X., Wang, X., Liang, S., Zhao, J. & Feng, Q. (2018) Balanced Scorecard-Based Performance Evaluation of Chinese County Hospitals in Underdeveloped Areas. Journal of International Medical Research 46(5): 1947–1962. https://doi.org/10.1177/0300060518757606.
- García, B. (2007) The Use of Information for Management by Clinicians. Un Estudio en los Hospitales Públicos Españoles, paper presented at the XIV AECA Congress, “Company and Society: Responding to Change”, 19-21 September,Valencia.
- Gordon, D., Chapman, R., Kunov, H., Dolan, A. & Carter, M. (1998) Hospital Management Decision Support: A Balanced Scorecard approach. Studies in Health Technology and Informatics, 52: 453-456.
- Grant, R. (2013) Contemporary Strategy Analysis. Chichester, John Wiley & Sons. Griffith, J. (1994) Reengineering Health Care: Management Systems for Survivors. Hospital & Health Services Administration, 39(4): 451-470.
- Harris, J., Quatman, C., Manring, M., Siston, R. & Flanigan, D. (2014) How to write a systematic review. The American Journal of Sports Medicine, 42: 2761-2768.
- Higgins, J. & Green, S. (2011) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration, Available at www.cochrane-handbook.org.(accessed February 29, 2020).
- Hitt, A., Ireland, R. & Hoskisson R. (2009) Strategic Management Concepts & Cases. Competitiveness and Globalization. South-Western Cengage Learning.
- Hoque, Z. (2014) 20 Years of Studies on the Balanced Scorecard: Trends, Accomplishments, Gaps and Opportunities for Future Research. The British Accounting Review, 46(1): 33-59. https://doi.org/10.1016/j.bar.2013.10.003.
- Inamdar N., Kaplan, R. & Bower, M. (2002) Applying the Balanced Scorecard in healthcare provider organizations. Journal Healthcare Management, 47(3): 179-195.
- Ittner, C. & Larcker, D. (1998) Innovations in performance measurement: Trends and research implications. Journal of Management Accounting Research, 10(2): 205-238.
- Jabbour, C. (2013) Environmental training in organisations: From a literature review to a framework for future research. Resources, Conservation and Recycling, 74: 144-155.
- Joyce L. (2003) Performance Management in the Health Service, paper presented at the QMW public safety seminar, Dublin, 11 September 2003.
- Jordan, H., Neves, J. & Rodrigues, J. (2011) Management Control. Lisbon, Publishing Areas.
- Kallás, D. & Coutinho, A. (2005) Strategy Management: experiences and lessons from Brazilian companies. Rio de Janeiro, Elsevier.
- Kallás, D. & Ribeiro, F. (2008) Balanced Scorecard (BSC) – General Concepts. Available in: http://kcd.com.br/arquivos/3bsc_conceitos_gerais_2008.pdf (accessed October 15, 2019).
- Kanji, G., & Sá, P. (2002) Kanji's Business Scorecard. Total Quality Management, 13(1): 13-27.
- Kaplan, R. (2010) Conceptual Foundations of the Balanced Scorecard. Harvard Business School Publishing Corporation: 1-36.
- Kaplan, R. & Norton, D. (2009) Execution Award. Effectively implement your business strategy and strengthen your competitive advantage. Lisbon, Actual Editor.
- Kaplan, R. & Norton, D. (2008) Mastering the Management System. Harvard Business Review: 63-77.
- Kaplan, R. & Norton, D. (2006) Alignment: Using the Balanced Scorecard to Create Corporate Synergies. Rio de Janeiro, Campus.
- Kaplan, R. & Norton D. (2004) Strategy Maps: Converting Intangible Assets into Tangible Outcomes. Boston, Harvard Business Scholl Press.
- Kaplan, R. & Norton, D. (2001) The strategy focused organization: how Balanced Scorecard companies thrive in the new business environment. Boston, Harvard Business Scholl Press.
- Kaplan, R. & Norton, D. (2000) Having trouble with your strategy? Then map it. Harvard Business Review, 78(5): 167-176.
- Kaplan, R. & Norton, D. (1997) Strategy in Action: Balanced Scorecard. Rio de Janeiro, Campus.
- Kaplan, R. & Norton, D. (1996) Translating strategy into action – the BSC. Boston, Harvard Business School Press.
- Kaplan, R. & Norton, D. (1993) Putting the Balanced Scorecard to work. Harvard Business Review, 71(5): 134-142.
- Kaplan, R. & Norton, D. (1992) The Balanced Scorecard: Measures that drive performance. Harvard Business Review, 70(1): 172-180.
- Koumpouros, Y. (2013) Balanced scorecard: application in the General Panarcadian Hospital of Tripolis, Greece. International Journal of Health Care Quality Assurance, 26(4): 286–307. https://doi.org/10.1108/09526861311319546.
- Lin, Q., Liu, L., Liu, H. & Wang, D. (2013) Integrating hierarchical Balanced Scorecard with fuzzy linguistics for evaluating operating room performance in hospitals. expert
- Lindlbauer I., Jonas S., & Vera W. (2016) Change in Technical Effecienscy After Quality Managemen Certification: A DEA Approach Using Difference-in-Difference Estimation with Genetic Matching in the Hospital Industru. European Journal of Operation Research, 250: 1026-1036.
- Lipe, M. & Salterio, S. (2000) The Balanced Scorecard: Judgmental Effects of Common and Unique Performance Measures. The Accounting Review, 75: 283-298. https://doi.org/10.2308/accr.2000.75.3.283 (accessed October 23, 2019).
- Lueg, R. (2015) Success Factors in Balanced Scorecard Implementations – A Literature review. Management Revue,
- Lueg, R., & Julner, P. (2014) How are Strategy Maps Linked to Strategic and Organizational Change? A Review of the Empirical Literature on the Balanced Scorecard. Corporate Ownership & Control, 11(4): 439-446.
- Lueg, R., & Silva, A. (2013) When One Size Does Not Fit All: A Literature Review on the Modifications of the Balanced Scorecard. Problems and Perspectives in Management, 11(3): 86-94.
- Macedo, N. (2014) The Balanced Scorecard as an instrument for implementing internal contractualization: the case of CHTS surgical services. Hospital Management, April: 4-9.
- Madaleno, J. (2015) A proposal to systematize performance indicators in the hospital area. Master's Thesis, Fluminense Federal University, Niterói.
- Madsen, D., & Stenheim, T. (2015) The Balanced Scorecard: A Review of Five Research Areas. American Journal of Management, 15(2): 24-41.
- Maia, J. Oliveira, G. & Martins, R. (2008) The role of performance measurement in the strategic process: an attempt at theoretical synthesis. Revista Eletrônica Sistemas & Gestão, 3(2): 129-146, May-Aug.
- Malina, M. & Selto, F. (2001) Communicating and controlling strategy: an empirical study of the effectiveness of the Balanced Scorecard. Journal of Management Accounting Research, 13: 47-90.
- Manica, J. (2009) Descriptive study of strategic performance indicators in companies based in the Autonomous Region of Madeira. Master's Dissertation: University of Lisbon, Higher Institute of Economics and Management.
- Martins, N. (2015) Balanced Scorecard in a social economy organization. Master's Dissertation, University of Lisbon, Higher Institute of Economics and Management.
- Martunis, A., Dalimunthe, R., Amalia, K., Juanita, J., Syahputra, H., Adam, M. & Masyudi, M., (2020) Adaptation of the Balanced Scorecard model to measure performance of the departments at Dr Zainoel Abidin Regional General Hospital, Banda Aceh. Journal of Modeling in Management. https://doi.org/10.1108/JM2-09-2018-0149.
- Marçal, C. (2008) The evaluation of business performance: the next step to the implementation of the management system. Master's Thesis, Brazilian School of Public and Business Administration, Fundação Getúlio Vargas, Rio de Janeiro.
- Massingham, R.; Massingham, P. & Dumay, J. (2018) Improving integrated reporting: A new learning and growth perspective for the Balanced Scorecard. Journal of Intellectual Capital, 20: 60–82.
- Matos, L. (2006) The use of the Balanced Scorecard to monitor the performance of a hospital. Unpublished Master's Thesis, University of Minho, Braga.
- Matos, L. & Ramos, I. (2009) The Balanced Scorecard in hospitals. Lisbon, Sílabo Editions.
- Meliones J, Alton M, Mericle J, Ballard R, Cesari J, Frush K & Mistry K (2008) 10-Year Experience Integrating Strategic Performance Improvement Initiatives: Can the Balanced Scorecard, Six Sigma®, and Team Training All Thrive in a Single Hospital? Advances in Patient Safety: New Directions and Alternative Approaches, 8(3): 148-153.
- Meliones, J. (2000) Saving Money, Saving Lives. Harvard Business Review, 78 (6), 57- 67. Available at web of science (accessed September 18, 2019).
- Mintzberg, H. (1994) The Rise and Fall of Strategic Planning. Englewood Cliffs, Prentice Hall.
- Mooraj, S., Oyon, D. & Hostettler, D. (1999) The Balanced Scorecard: a Necessary Good or an Unnecessary Evil? European Management Journal, 17(5): 481-491, October.
- Naranjo-Gil, D. (2009) Strategic performance in hospitals: the use of the Balanced Scorecard by nurse managers. Health Care Management Review, 34(2), 161-170. doi: 10.1097/HMR.0b013e31819e8fd0.
- Neely, A., Gregory, M. & Platts, K. (1995) Performance measurement system design - a literature review and research agenda. International Journal of Operations & Production Management, 15(4): 80-116.
- Nicholson, J., McCrillis, A. & Williams, J. (2017) Collaboration challenges in systematic reviews: a survey of health sciences librarians. Journal of the Medical Library Association, 105: 385-393.
- Niven, P. (2005) Driving Focus and Alignment with the Balanced Scorecard. Why Organizations Need a Balanced Scorecard. The Journal for Quality & Participation, 32(3): 1-25.
- Niven, P. (2003) Balanced Scorecard Step-By-Step: for government and nonprofit agencies. New Jersey, John Wiley & Sons, Inc.
- Niven, P. (2002) Balanced Scorecard - Step by Step - Maximizing Performance and Maintaining Results. New York, John Wiley & Sons, Inc.
- Norreklit, H. (2003) The Balanced Scorecard: What is the score? A rhetorical analysis of the Balanced Scorecard. Accounting, Organizations and Society, 28(6): 591-619.
- Norreklit, H. (2000) The Balanced Scorecard – a critical analysis of some of its assumptions. Management Accounting Research, 11: 65-88.
- Ojah, H., Malik, Y., & Ali, A (2019) The Use of the Balanced Scorecard in Improving Health Performance-The Study of the Health Sector in Iraq. International Journal of Multidisciplinary Research and Publications, 2(5), 24-30.
- Oliveira, D. (2006) Strategic Planning: Concepts, Methodology and Practices. Sao Paulo, Atlas.
- Oliveira, A., Costa, B. & Cameira, R. (2007) Proposal for the design of a process-oriented performance measurement system: application in an operational support service provider, communication resented at XIV SIMPEP - Engineering Symposium production, November. Organization for Economic Cooperation and Development (2015) Review of health care quality: Portugal raising standards. Paris, OECD Publishing.
- Oyewo, B., Oyedokun, G., and Azuh, A. (2019) The Use of Multi-Perspective Strategic Performance Measures by Manufacturing Firms: Benefits, Determinants and Challenges. DLSU Business & Economics Review, 29(1): 115-130.
- Padoveze, C. (2007) Strategic and Operational Controllership. Salvador, Cengage Learning Editions.
- Paré, G., Trudel, M., Jaana, M. & Kitsiou, S. (2015) Synthesizing information systems knowledge: A typology of literature reviews. Information and Management, 52(2): 183–199.
- Penha, R. & Costa, J. (2012) Findings on the construction of strategic maps: a case study in the third sector. GEPROS - Production, Operations and Systems Management, 7(3): 41-56, July-September.
- Pereira, G. (2005) Balanced Scorecard in hospitals. Master's Thesis, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil.
- Petrou. S., Kwon, J. & Madan, J. (2018) A practical guide to conducting a systematic review and meta-analysis of health state utility values. Pharmacoeconomics, 36: 1043-1061.
- Petticrew, M. & Roberts, H. (2006) Systematic reviews in the social sciences: a practical guide. United Kingdom, Blackwell Publishing Ltd.
- Pink, G., McKillop, I., Schraa, E. & Preyra, C. (2001) Creating a Balanced Scorecard for a hospital system. Journal of healthcare finance, 27(3), 1-20.
- Pinto, F. (2013) Use of the Balanced Scorecard in Times of Recessive Economy. Magazine of the Order of Certified Accountants, 159: 55-64.
- Pinto F. (2009) Balanced Scorecard - Aligning Changes, Strategy and Performance in Public Services. Lisbon, Sílabo Editions.
- Porporato, M., Tsasis, P. & Marin, L. (2017) Do hospital's Balanced Scorecard measures reflect cause-effect relationships? International Journal of Productivity and Performance Management, 66(3): 338–361. https://doi.org/10.1108/IJPPM-02-2015-0029.
- Prazeres, R., Lopes, L. & Meira, J. (2013) Balanced Scorecard (BSC): An analysis of the Profile of its Applications in the Annals of ANPCONT, ENANPAD and USP. Revista de Contabilidade da UFBA, 7(2): 52-65, May-August.
- Prieto, V., Carvalho, M. & Fischmann, A. (2009) Comparative analysis of strategic alignment models. Production Journal, 19(2): 317-331.
- Qudrat-Ullah, H., Chow, C. & Goh, M. (2007) Towards a dynamic Balanced Scorecard approach: the case of Changi General Hospital in Singapore. International Journal of Enterprise network Management, 1(3): 230-237. https://doi.org/10.1504/IJENM.2007.012756.
- Quesado, P., Guzmán, B. & Rodrigues, L. (2018) Advantages and contributions in the Balanced Scorecard implementation. Intangible Capital, vol. 14(1): 186-201.
- Quesado, P., & Macedo, N. (2010) The Balanced Scorecard in the Emergency Department of a Corporate Public Hospital: Case Study. XIV Encuentro AECA, 42d. Coimbra. Available inhttp://www.aeca1.org/ (accessed September 13, 2019).
- Quintella, O. (2004) The Balanced Scorecard as a Tool for Developing a Performance Measurement System: An Implementation Proposal. Master's Thesis, Fluminense Federal University, Niterói.
- Rabbani F, Jafri S, Abbas F, Shah M, Azam S, Shaikh B, Brommels M & Tomson G. (2010) Designing a Balanced Scorecard for a tertiary care hospital in Pakistan: a modified Delphi group exercise. The International Journal of Health Planning and Management, 25(1): 74–90. https://doi.org/10.1002/hpm.1004.
- Rahimi, H., Bahmaei, J., Shojaei, P., Kavosi, Z. & Khavasi, M. (2018) Developing a Strategy Map to Improve Public Hospitals Performance with Balanced Scorecard and DEMATEL Approach. Shiraz E-Medical Journal in Press, 19(7). https://doi.org/10.5812/semj.64056.
- Ribeiro, C. (2008) Management control in health facilities: the Balance Scorecard. OCD, 100: 61–66.
- Rompho, N. (2011) Why the Balanced Scorecard fails in SME's: a case study. International Journal of Business and Management, 6(11): 39-46.
- Rua, O. e Silva, T. (2016) Contribution of the Balanced Scorecard to the Strategic Management of Corporate Public Hospital Units: A Case Study. Portuguese Journal of Finance, Management and Accounting, 2(4): 100-136. Available in http://u3isjournal.isvouga.pt/index.php/PJFMA.
- Russo, J. (2015) Balanced Scorecard for SMEs and Small and Medium-Sized Institutions. Lisbon, Lidel.
- Sampaio, R. & Mancini, M. (2006) Systematic review studies: a guide for a judicious synthesis of scientific evidence. Brazilian Journal of Physiotherapy, 11(1): 83-89.
- Sanchez, K., Stadnick, K. & Erdmann, R. (2002) Balanced Scorecard: A Managerial Innovation Tool in Hospital Organization Management, paper presented at the XXII Technological Innovation Management Symposium, November 6-8, Salvador da Bahia Brazil.
- Santos, L. (2014) Balanced scorecard: contributions to implementation in Local Administration. Master's Thesis, Higher Institute of Education and Sciences, Lisbon.
- Santos, A. (2008) Strategic management: concepts, models and instruments. Lisbon, Escolar Editora.
- Santos, A. (2006) Balanced Scorecard in Portugal: Vision, Strategy and Enthusiasm. Cascais, Publisher Parchment.
- Schmidt, S., Bateman, I., Breinlinger, J. & Smith, P. (2006) A management approach that drives actions strategically: Balanced scorecard in a mental health trust case study. International Journal of Health Care Quality Assurance, 19(2): 119–135. https://doi.org/10.1108/09526860610651663.
- Senge, P. (2010) The Fifth Discipline: the art and practice of the learning organization. Rio de Janeiro, Best Seller.
- Serrano, V. (2017) Balanced scorecard for children's mental health: proposal for the pediatric psychiatry specialty at Hospital Dona Estefânia. Master's Thesis, National School of Public Health, Lisbon.
- Silva, I. (2012) Strategic management: Balanced Scorecard for a hospital entity. Master's Dissertation, Polytechnic Institute of Porto, Porto.
- Silva, J. & Nunes J. (2007) The Balanced Scorecard in Strategic Management: Case of a Public Hospital, paper presented at the II Health Management Seminar, 18-19 May, University of Beira Interior, Covilhã.
- Silva, B. & Prochnik, V. (2005) Seven Challenges for the Implementation of Balanced Scorecard in Hospitals, paper presented at the 3rd Conference on Performance Measurement and Management Control, 22-23 September, Nice.
- Smith, R., (2007) Business Process Management and the Balanced scorecard: using processes as strategic drivers. New Jersey, John Wiley and Sons.
- Smith, M. & Loonam, J. (2016) Exploring strategic execution: A case study on the use of the Balanced Scorecard within an Irish hospital. Journal of Strategy and Management, 9(4): 406–428. https://doi.org/10.1108/JSMA-11-2015-0094.
- Sousa, J. (2016) Balanced Scorecard proposal for Guarda's local health unit. Master's Thesis, University of Lisbon. Higher Institute of Economics and Management.
- Sousa, M. & Rodrigues, L. (2002) The Balanced Scorecard: a strategic management tool for the 21st century. Porto, King of Books.
- Skrinjar, R., Bosilj-Vuksic, V. & Stemberger, M. (2008) The impact of business process orientation on financial and non-financial performance.Business Process Management Journal, 14 (5): 738-754.
- Tachizawa, T. & Rezende, W. (2000) Business Strategy. Trends and Challenges: A focus on the Brazilian reality. Sao Paulo, Makron Books.
- Tarigan, S., & Bachtiar, A. (2019) A review of the Balanced Scorecard implementation in health organization. Proceedings of the International Conference on Applied Science and Health, 4: 942-949.
- Tuan, T. (2020) The Impact of Balanced Scorecard on Performance: The Case of Vietnamese Commercial Banks. The Journal of Asian Finance, Economics and Business (JAFEB), 7(1): 71-79.
- Uttley, L. & Montgomery, P. (2017) The influence of the team in conducting a systematic review. Systematic Reviews, 6(1):149.
- Verzola, A., Bentivegna, R., Carandina, G., Trevisani, L., Gregorio, P. & Mandini, A. (2009) Multidimensional evaluation of performance: experimental application of the Balanced Scorecard in Ferrara university hospital. Cost Effectiveness and Resource Allocation, 7(1): 7-15. https://doi.org/10.1186/1478-7547-7-15.
- Vieira, E. (2008) Characteristics of Organizational Performance Measurement: a descriptive study in hospitals in the State of Rio Grande do Norte. Master's Thesis, Federal University of Rio Grande do Norte.
- Vitória, F. (2017) Balanced Scorecard: A literature review (2000 – 2017). Postgraduate Project, University of Brasilia.
- Walker, K. & Dunn, L. (2006) Improving hospital performance and productivity with the Balanced Scorecard. Academy of Health Care Management Journal, (2): 85-110.
- Ward. R., Usher-Smith, J. & Griffin, S. (2019) How to produce a systematic review. InnovAiT, 12(3): 155-157.
- Weiss, A. & Downar, J. (2013) Ontario Hospitals Are Not Using Palliative Care Performance Indicators in Their Balanced Scorecards. Journal of Pain and Symptom
- Werner, M. & Xu, F. (2012) Executing Strategy with the Balanced Scorecard. International Journal of Financial Research, 3(1): 88-94.
- Wright, R; Brand, R; Dunn, W. & Spindler, K. (2007) How to write a systematic review. Clinical Orthopedics and Related Research, 455: 23-9.
- Xiao, Y. & Watson, M. (2017) Guidance on Conducting a Systematic Literature Review. Journal of Planning Education and Research, 1-20.
- Yang, M. & Tung, Y. (2006) Using Path Analysis to Examine Causal Relationships Among Balanced Scorecard Performance Indicators for General Hospitals: The Case of a Public Hospital System in Taiwan. Healthcare management review, 31(4): 280-288. IT HURTS:10.1097/00004010-200610000-00003.
- Zelman, W., Pink, G. and Matthias, C. (2003) Use of the Balanced Scorecard in Health Care. Journal of Health Care Finance, 29 (4): 1-16.
- Zhou, P., Zhou, P., Yüksel, S., Dinçer, H., & Uluer, G. (2020) Balanced Scorecard- Based Evaluation of Sustainable Energy Investment Projects with IT2 Fuzzy Hybrid Decision Making Approach. Energies, 13(1): 82.
- Behrouzi, F. & Ma'aram, A. (2019) Identification and ranking of specific Balanced Scorecard performance measures for hospitals: A case study of private hospitals in the Klang Valley area, Malaysia. The International Journal of Health Planning and Management 34 (4), 1364–1376. https://doi.org/10.1002/hpm.2799.
- Chang, W., Tung, Y., Huang, C. & Yang, M. (2008) Performance improvement after implementing the Balanced Scorecard: A large hospital's experience in Taiwan. Total Quality Management & Business Excellence, 19(11): 1143–1154. https://doi.org/10.1080/14783360802323560.
- Chen, H., Hou, Y. & Chang, R. (2012) Application of the Balanced Scorecard to an academic medical center in Taiwan: the effect of warning systems on improvement of hospital performance. Journal of the Chinese Medical Association, 75(10): 530–535. https://doi.org/10.1016/j.jcma.2012.07.007.
- Chen, X., Yamauchi, K., Kato, K., Nishimura, A. & Ito, K. (2006) Using the Balanced Scorecard to measure Chinese and Japanese hospital performance. International Journal of Health Care Quality Assurance, 19(4): 339–350. https://doi.org/10.1108/09526860610671391.
- El-Jardali, F., Saleh, S., Ataya, N. & Jamal, D. (2011) Design, implementation and scaling up of the Balanced Scorecard for hospitals in Lebanon: Policy coherence and application lessons for low- and middle-income countries. Health Policy, 103(2-3): 305–314. https://doi.org/10.1016/j.healthpol.2011.05.006.
- Gao, H., Chen, H., Feng, J., Qin, X., Wang, X., Liang, S., Zhao, J. & Feng, Q. (2018) Balanced Scorecard-Based Performance Evaluation of Chinese County Hospitals in Underdeveloped Areas. Journal of International Medical Research 46(5): 1947–1962. https://doi.org/10.1177/0300060518757606.
- Gordon, D., Chapman, R., Kunov, H., Dolan, A. & Carter, M. (1998) Hospital Management Decision Support: A Balanced Scorecard approach. Studies in Health Technology and Informatics, 52: 453-456.
- Inamdar N., Kaplan, R. & Bower, M. (2002) Applying the Balanced Scorecard in healthcare provider organizations. Journal Healthcare Management, 47(3): 179-195.
- Koumpouros, Y. (2013) Balanced Scorecard: application in the General Panarcadian Hospital of Tripolis, Greece. International Journal of Health Care Quality Assurance, 26(4): 286–307.https://doi.org/10.1108/09526861311319546.
- Lin, Q., Liu, L., Liu, H. & Wang, D. (2013) Integrating hierarchical Balanced Scorecard with fuzzy linguistics for evaluating operating room performance in hospitals. expert
- Martunis, A., Dalimunthe, R., Amalia, K., Juanita, J., Syahputra, H., Adam, M. & Masyudi, M., (2020) Adaptation of the Balanced Scorecard model to measure performance of the departments at Dr Zainoel Abidin Regional General Hospital, Banda Aceh. Journal of Modeling in Management. https://doi.org/10.1108/JM2-09-2018-0149.
- Meliones J, Alton M, Mericle J, Ballard R, Cesari J, Frush K & Mistry K (2008) 10-Year Experience Integrating Strategic Performance Improvement Initiatives: Can the Balanced Scorecard, Six Sigma®, and Team Training All Thrive in a Single Hospital? Advances in Patient Safety: New Directions and Alternative Approaches, 8(3): 148-153.
- Naranjo-Gil, D. (2009) Strategic performance in hospitals: the use of the Balanced Scorecard by nurse managers. Health Care Management Review, 34(2), 161-170. doi: 10.1097/HMR.0b013e31819e8fd0.
- Pink, G., McKillop, I., Schraa, E. & Preyra, C. (2001) Creating a Balanced Scorecard for a hospital system. Journal of healthcare finance, 27(3), 1-20.
- Porporato, M., Tsasis, P. & Marin, L. (2017) Do hospital's Balanced Scorecard measures reflect cause-effect relationships? International Journal of Productivity and Performance Management, 66(3): 338–361. https://doi.org/10.1108/IJPPM-02-2015-0029.
- Qudrat-Ullah, H., Chow, C. & Goh, M. (2007) Towards a dynamic Balanced Scorecard approach: the case of Changi General Hospital in Singapore. International Journal of
- Rabbani F, Jafri S, Abbas F, Shah M, Azam S, Shaikh B, Brommels M & Tomson G. (2010) Designing a Balanced Scorecard for a tertiary care hospital in Pakistan: a modified Delphi group exercise. The International Journal of Health Planning and Management, 25(1): 74–90. https://doi.org/10.1002/hpm.1004.
- Rahimi, H., Bahmaei, J., Shojaei, P., Kavosi, Z. & Khavasi, M. (2018) Developing a Strategy Map to Improve Public Hospitals Performance with Balanced Scorecard and DEMATEL Approach. Shiraz E-Medical Journal in Press, 19(7). https://doi.org/10.5812/semj.64056.
- Schmidt, S., Bateman, I., Breinlinger, J. & Smith, P. (2006) A management approach that drives actions strategically: Balanced scorecard in a mental health trust case study. International Journal of Health Care Quality Assurance, 19(2): 119–135. https://doi.org/10.1108/09526860610651663.
- Smith, M. & Loonam, J. (2016) Exploring strategic execution: A case study on the use of the Balanced Scorecard within an Irish hospital. Journal of Strategy and Management, 9(4): 406–428. https://doi.org/10.1108/JSMA-11-2015-0094.
- Verzola, A., Bentivegna, R., Carandina, G., Trevisani, L., Gregorio, P. & Mandini, A. (2009) Multidimensional evaluation of performance: experimental application of the Balanced Scorecard in Ferrara university hospital. Cost Effectiveness and Resource Allocation, 7(1): 7-15. https://doi.org/10.1186/1478-7547-7-15.
- Weiss, A. & Downar, J. (2013) Ontario Hospitals Are Not Using Palliative Care Performance Indicators in Their Balanced Scorecards. Journal of Pain and Sympto Management 46(2), e1–e5. https://doi.org/10.1016/j.jpainsymman.2013.03.006.
- Yang, M. & Tung, Y. (2006) Using Path Analysis to Examine Causal Relationships Among Balanced Scorecard Performance Indicators for General Hospitals: The Case of a Public Hospital System in Taiwan. Healthcare management review, 31(4): 280-288. IT HURTS: 10.1097/00004010-200610000-00003
Quick links
- Abstract
- Conclusion
- Investigation Limitations
- Research Suggestions
- Introduction
- The Balanced Scorecard
- Fundamental Elements of the Balanced Scorecard
- Mission, Vision, Values and Strategy
- Objectives, Indicators, Goals and Initiatives
- Cause-Effect Relationships and Strategic Map
- prospects
- BSC in the Health Sector
- Benefits and Difficulties in Applying the BSC Applied to Health Organizations
- Methodology
- Systematic Review of Literature
- Main steps of the systematic review of the literature on the application of the BSC in Hospital Unit
- General Objective and Research Questions
- descriptors
- Search sources
- Selection of articles
- Question 1: What are the characteristics of publications that report the application of the BSC in h
- Question 2: What is the motivation for using the BSC?
- Question 3: What are the characteristics of the hospitals where the BSC was implemented?
- Question 4: Who are the stakeholders in the design and implementation of the BSC?
- Question 5: Which perspectives and performance indicators are most frequently used in the applicatio
- Question 6: What are the facilitating factors in the design and implementation of the BSC?
- Question 7: What are the results obtained with the implementation of the BSC?
- Question 8: What are the difficulties and/or limitations of implementing the BSC?
- Question 9: What opportunities are there for future investigations in this area?
- References


