Archive : Article / Volume 3, Issue 2
- Research Article | DOI:
- https://doi.org/10.58489/2836-3558/020
Bipolar Disorder and Climatic Factors
1Consultant in psychiatry, Private clinic, 23 rue mongi slim 7050 Menzel bourguiba, Tunisia.
2Consultant in psychiatry, Centre hospitalier Hedi Chaker, psychiatry department A, route el ain km 0,5, 3029 Sfax, Tunisia.
Tarek Triki*
Tarek Triki, Rim Sellami, (2024). Bipolar Disorder and Climatic Factors. Psychiatry and Psychological Disorders. 3(2); DOI: 10.58489/2836-3558/020
© 2024 Tarek Triki, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 27-04-2024
- Accepted Date: 27-05-2024
- Published Date: 29-05-2024
Bipolar disorder, mania, depression, melatonin, season.
Abstract
Introduction: Climate change is a global phenomenon that affects various aspects of our lives, from the environment to our physical health. However, its impact on mental health, particularly on conditions like bipolar disorder, has gained increasing attention in recent years and several studies have suggested a correlation between seasonal changes and the nature of episodes during relapses.
Methods: This is a descriptive retrospective study of a sample of 100 Tunisian patients with bipolar disorder type I to investigate the influence of climatic factors on the evolutionary profile of bipolar disorder in order to determine the distribution of depressive and manic episodes based on the season of relapses. A pre-established form containing socio-demographic and clinical data was completed. All patients gave oral consent.
Results: The findings indicate a tendency for manic relapses during spring-summer and depressive episodes during autumn-winter. This observation is supported by the monthly distribution of relapses, showing a prevalence of manic relapses during warm months and depressive episodes during cold months. Over a period of ten years, the analysis of 230 thymic episodes confirms this trend, highlighting the prevalence of manic episodes during hot season and depressive episodes during cold season.
Discussion: Despite the limitations of this study, such as sample size, the results suggest a potential seasonal influence on the evolutionary profile of bipolar disorder type I. Our results are conform to literature.
Conclusion: Climate changes have been very marked in last years and their consequences on mental health are becoming increasingly known. Taking this into account could contribute to the development of a more appropriate and targeted care for patients suffering from psychiatric disorders, and in particular in the case of bipolar disorder.
Introduction
Seasons influence various biological pathways, including gene transcription and neurotransmitters [1,2]. As a result, seasonal change has an impact on a wide range of diseases, not only physical, but also mental diseases [3]. Indeed, it has an impact on mood and this has been the subject of several studies [4.5].
Some authors from the southern hemisphere have shown that blacks have a higher rate of manic symptoms compared to other ethnic groups [6]. Similarly, Douki et al. [7] had observed that the hospital incidence of manic episodes strictly matched photoperiod variations. In addition, the impact of climate on the evolution of bipolar disorder has been reported in several studies on populations in the northern hemisphere since the majority of studies indicated that hospitalizations for a manic episode peaked in spring season [8, 9].
In this regard, we have undertaken a descriptive retrospective study of a sample of 100 Tunisian patients with bipolar disorder type I to study the influence of climate factors on the evolutionary profile of this disorder by determining the distribution of depressive and manic episodes according to the season of relapse.
Materials and methods
Research Design
This is a retrospective study of patients who visited the private clinic between 1 January 2021 and 31 December 2023. All patients included in the study had a diagnosis of Bipolar I disorder according to DSM-5 criteria.
The criteria for non-inclusion of patients were the presence of major cognitive impairment or mental retardation, bipolar disorder evolution is less than 10 years, while excluding patients whose certain information could not be collected.
Instrument for Data Collection
Informed consent was obtained from all subjects enrolled.
Sociodemographic and clinical data including age, sex, marital status, professional status, thymic relapse were recorded for all patients.
Data Analysis
The data were analyzed by the Excel program.
Results
1/ Sociodemographic data
Our sample consisted of 52 males and 48 females, 57 of whom were single, 26 married, 8 divorced and 9 widows.
The average age of the sample was 40.8 years with a minimum age of 18 and a maximum age of 66. As regards professional status, the sample consisted of 54 working patients and 46 non-working.
2/ Monthly thymic relapse distribution:
In our study, we have divided the thymic episodes according to the season of occurrence: the spring-summer season (I) and the autumn-winter season (II).
a/ Monthly distribution of the last thymic relapse:
Regarding recent thymic relapses, manic episodes occurred significantly more frequently during the spring-summer season (mania I) than during the autumn-winter season (mania II) (52 versus 10; p<0>
Similarly, we found more depressive episodes that occurred during the autumn-winter season (depression II) than during the spring-summer season (Depression I) (31 versus 7; p<0>
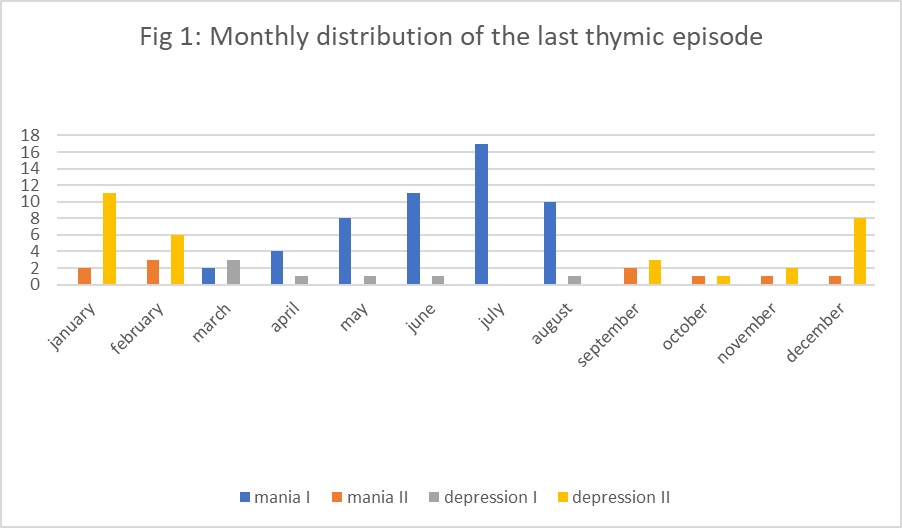
Fig 1 shows the monthly distribution of the last thymic episode
b/ Monthly distribution of thymic relapses over the last ten years:
During the last ten years, we have recorded 230 thymic episodes with the following distribution: Mania I=101 versus Mania II=40; and depression II=61 versus depression I=28.
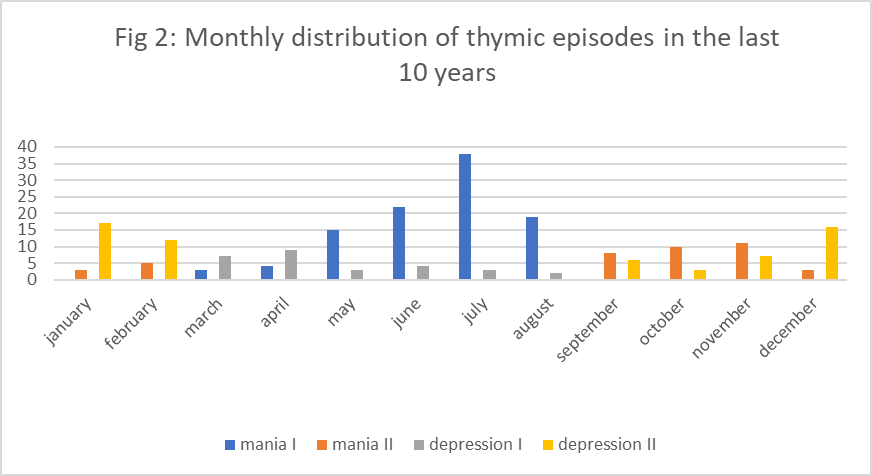
Fig 2 illustrates the predominance of manic episodes during the hot spring-summer period of the year as opposed to depressive episodes that are predominant during the cold autumn-winter period with low temperatures (respectively; p<0>
Discussion
Our study showed that manic relapses occurred more frequently during the spring-summer period, as opposed to depressive relapse that is more common during the autumn-winter period.
Our results were consistent with those of Faedda et al. [10] which determined 2 seasonal patterns:
• Type A: depression in autumn-winter + mania and hypomania in spring-summer
• Type B: depression in spring-summer + mania and hypomania in autumn-winter
According to them, pattern A is more common in bipolar patients, and they found two monthly peaks of manic and depressive episodes in April and September, respectively. Similarly, Szabo et al. [11] and Myers et al. [12] reported a recrudescence of manic episodes in spring and summer. Also, in Australia, Mullder et al. [13] identified manic peaks in summer and spring.
For depression, Rihmer et al. [14] recorded a peak in winter and Silverstone et a. [15] saw a peaking in autumn.
With regard to affective disorders (major depression, type I and type II bipolar disorder), several authors have found that manic and hypomanic episodes typically peak in spring/summer with a minor peaks in autumn, while depressive episodes peak during winter and mixed episodes reach their peaks in early spring or mid/end summer [9, 16].
In fact, DOUKI et al. [17], by studying a bipolar population recruited at the psychiatric hospital, demonstrated that the incidence of mania follows and is consistent with monthly changes in temperature and length of the photoperiod.
In this context, Cho et al. found that there is hypersensitivity of circadian rhythms to light in patients with seasonal depressive disorder and bipolar disorder, as well as in individuals at risk of developing bipolar disturbance compared to healthy control subjects [18].
Some studies have suggested a correlation between seasonal changes and bipolar episodes onset. Bauer et al. [19] found that people with bipolar disorder may have a seasonal pattern in the occurrence of manic or depressive episodes. As a result, sunlight, temperature and length of the day can influence circadian rhythms, potentially triggering mood swings in sensitive individuals [19].
In addition, rising temperatures due to global warming and increased frequency of extreme weather events can contribute to increased anxiety and agitation in people with bipolar disorder. In fact, Hayes et al. [20] pointed out that exposure to extreme heat could aggravate the symptoms of mania and increase the risk of hospitalization in people with bipolar disorder [20].
Actually, people with bipolar disorder can be vulnerable to the psychological impact of climate-related events. Indeed, Obradovich et al. [21] have demonstrated an association between exposure to climate disasters and increased hospitalizations for mood disorders, including bipolar disorder.
This finding could be explained by the results of Nathan et al. [22]. They compared three groups of patients: one group of bipolar patients, a group of patients with seasonal affective disorder, and a last group with major depressive disorder. Hypersensitivity to light as a result of suppression of melatonin secretion was noted in patients with bipolar and seasonal affective disorder; whereas patients with major depressive disorder did not have this hypersensibility. Other authors have shown that bipolar euthymic patients also don’t have this hypersensitivity to light [23].
Such a role of melatonin has been advanced by other researchers by suggesting that the luminosity and increased hours of sunlight (photoperiode) lead to a “suppression” of melotonin and the increase of mania levels [24]. Similarly, Nürnberger et al. [25] have invoked a possible melatoninergic dysfunction. Light therapy and melatonin could therefore be promising in the treatment of manic episode [26] and seasonal depression [27].
In a recent paper, Zhang and Volkow highlighted the important role of the dopamine (DA) and serotonin (5-HT) systems in seasonal fluctuations in psychiatric symptoms, and that beyond these two neurotransmitters, the seasonal patterns of other neuro-transmitter and neuropeptide systems remain to be studied in humans [28].
Conclusion
The interaction between climate change and bipolar disorder is probably multifactorial, complex and requires further exploration. Understanding the impact of climate on mental health, especially for vulnerable populations such as those with bipolar disorder, is essential for developing targeted interventions and support systems. As the global community faces the consequences of climate change, addressing mental health implications is becoming increasingly important for a comprehensive approach to well-being.
References
- Dopico, X. C., Evangelou, M., Ferreira, R. C., Guo, H., Pekalski, M. L., Smyth, D. J., & Todd, J. A. (2015). Widespread seasonal gene expression reveals annual differences in human immunity and physiology. Nature communications, 6(1), 7000.
- Aumann, T. D., Raabus, M., Tomas, D., Prijanto, A., Churilov, L., Spitzer, N. C., & Horne, M. K. (2016). Differences in number of midbrain dopamine neurons associated with summer and winter photoperiods in humans. PloS one, 11(7), e0158847.
- Razzaque, M. S. (2018). Sunlight exposure: Do health benefits outweigh harm? The Journal of steroid biochemistry and molecular biology, 175, 44-48.
- Patten SB, Williams JVA, Lavorato DH, Wang JL, Bulloch AGM. Major depression prevalence increases with latitude in Canada. Can J Psychiatry. 2017;62:62–66.
- Coimbra, D. G., e Silva, A. C. P., de Sousa-Rodrigues, C. F., Barbosa, F. T., de Siqueira Figueredo, D., Santos, J. L. A., ... & de Andrade, T. G. (2016). Do suicide attempts occur more frequently in the spring too? A systematic review and rhythmic analysis. Journal of affective disorders, 196, 125-137.
- Kirov, G., & Murray, R. M. (1999). Ethnic differences in the presentation of bipolar affective disorder. European psychiatry, 14(4), 199-204.
- Douki, S., Ben Zineb, S., & Nacef, F. (2005). Le trouble bipolaire dans les pays du Sud. L'Encéphale (Paris), 31(4).
- Geoffroy, P. A., Bellivier, F., Scott, J., & Etain, B. (2014). Seasonality and bipolar disorder: a systematic review, from admission rates to seasonality of symptoms. Journal of Affective Disorders, 168, 210-223.
- Rosenthal, S. J., Josephs, T., Kovtun, O., & McCarty, R. (2020). Seasonal effects on bipolar disorder: a closer look. Neuroscience & Biobehavioral Reviews, 115, 199-219.
- Faedda GL, Tondo L, Teicher MH, Baldessarini RJ, Gelbard HA, Floris GF. Seasonal mood disorders. Patterns of seasonal recurrence in mania and depression. Arch Gen Psychiatry 1993; 50: 17-23.
- Szabo, C. P., & Blanche, M. T. (1995). Seasonal variation in mood disorder presentation: further evidence of this phenomenon in a South African sample. Journal of affective disorders, 33(4), 209-214.
- Myers, D. H., & Davies, P. (1978). The seasonal incidence of mania and its relationship to climatic variables. Psychological Medicine, 8(3), 433-440.
- Mulder, R. T., Cosgriff, J. P., Smith, A. M., & Joyce, P. R. (1990). Seasonality of mania in New Zealand. Australian & New Zealand Journal of Psychiatry, 24(2), 187-190.
- Rihmer, Z. (1980). Season of birth and season of hospital admission in bipolar depressed female patients. Psychiatry Research, 3(3), 247-251.
- Silverstone, T., Romans, S., Hunt, N., & McPherson, H. (1995). Is there a seasonal pattern of relapse in bipolar affective disorders? A dual northern and southern hemisphere cohort study. The British Journal of Psychiatry, 167(1), 58-60.
- Partonen, T., & Lönnqvist, J. (1998). Seasonal affective disorder. The Lancet, 352(9137), 1369-1374.
- Douki S, Ben Zineb S, Taktak MJ. (1997) Cultural aspects of bipolar disorder. Unpublished data. WPA Regional meeting, Beirut,
- Cho, C. H., Moon, J. H., Yoon, H. K., Kang, S. G., Geum, D., Son, G. H., ... & Lee, H. J. (2016). Molecular circadian rhythm shift due to bright light exposure before bedtime is related to subthreshold bipolarity. Scientific reports, 6(1), 31846.
- Bauer, M., Glenn, T., Alda, M., Andreassen, O. A., Angelopoulos, E., Ardau, R., ... & Whybrow, P. C. (2019). Association between solar insolation and a history of suicide attempts in bipolar I disorder. Journal of psychiatric research, 113, 1-9.
- Hooshangi, M. H., Nikookar, S., Ghane, S., Nouri, A., & Hossein, M. G. A review of pharmaco epidemiology research in the mental health field.
- Obradovich, N., Migliorini, R., & Paulus, M. P. (2018). Changes in perceived stress and psychiatric symptoms across temperature and weather among patients with bipolar disorder. Journal of Affective Disorders, 227, 172-179.
- Nathan, P. J., Burrows, G. D., & Norman, T. R. (1999). Melatonin sensitivity to dim white light in affectivedisorders. Neuropsychopharmacology,21(3),408-413.
- Whalley, L. J., Perini, T., Shering, A., & Bennie, J. (1991). Melatonin response to bright light in recovered, drug-free, bipolar patients. Psychiatry research, 38(1), 13-19.
- Medici, C. R., Vestergaard, C. H., Hadzi-Pavlovic, D., Munk-Jørgensen, P., & Parker, G. (2016). Seasonal variations in hospital admissions for mania: Examining for associations with weather variables over time. Journal of affective disorders, 205, 81-86.
- Nurnberger, J. I., Adkins, S., Lahiri, D. K., Mayeda, A., Hu, K., Lewy, A., ... & Davis-Singh, D. (2000). Melatonin suppression by light in euthymic bipolar and unipolar patients. Archives of general psychiatry, 57(6), 572-579.
- McGowan, N. M., Kim, D. S., de Andres Crespo, M., Bisdounis, L., Kyle, S. D., & Saunders, K. E. (2022). Hypnotic and melatonin/melatonin-receptor agonist treatment in bipolar disorder: a systematic review and meta-analysis. CNS drugs, 36(4), 345-363.
- Terman, J. S., Terman, M., Lo, E. S., & Cooper, T. B. (2001). Circadian time of morning light administration and therapeutic response in winter depression. Archives of general psychiatry,58(1), 69-75.
- Zhang R and Volkow ND (2023) Seasonality of brain function: Role in psychiatric disorders. Translational Psychiatry 13, 65.


