Archive : Article / Volume 2, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5917/006
Congestive Heart Failure in Indian Elders
1Karnataka State Rural Development and Panchayat Raj University,Public Health Consultant, India.
Suresh Kishanrao
Suresh Kishanrao (2023), Congestive Heart Failure in Indian Elders, Clinical Cardiovascular Research. 2(1). DOI: 10.58489/2836-5917/006
© 2023 Suresh Kishanrao, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original work is properly cited.
- Received Date: 03-02-2023
- Accepted Date: 22-02-2023
- Published Date: 27-02-2023
ageing; cardiovascular diseases; geriatric; left ventricular ejection factor (LVEF); ischaemic (IHD) & rheumatic heart disease (RHD); years lost due to disability (YLDS)
Abstract
Congestive Heart Failure (CHF) is a common complex clinical syndrome that underlines the inability of the heart to perform its circulatory function with the desired efficiency due to structural and/or functional alterations. There is paucity of good and reliable data in India and many developing countries on heart failure. The management of heart failurehas evolved over the years with the advent of new drugs and devices.But there is a need to uneartha true and meaningful nationaldata on the risk factors,available treatment options,and challenges in management that could be addressed to take advantage of the recent advances.
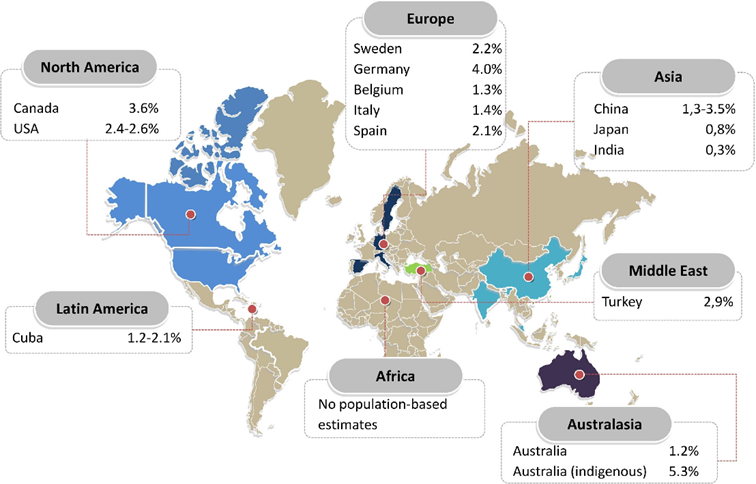
CHF is a disease of the âelderly,â frequently occurs in the setting of normal ejection fraction, and has a poor prognosis, regardless of the level of systolic function. The highest prevalence of CHF is reported among Indigenous Australian population (5.3%), Germany (4%) and Canada 3.6%, Turkey 2.9%, and USA 2.6% as compared to only 0.3% in Indian population. Overall, more than 5 persons aged 60 to 69 and 10 persons per 1,000 population after 65 years of age suffer from CHF. The incidence of CHF is equally frequent in men and women globally, but it is more amongelderly women in India comparedto elderly men. The burden of heart failure is increasing at an alarming rate worldwide as well as in India. CHF not only increases the risk of mortality, morbidity and worsens the patientâs quality of life, but also puts a huge burden on the overall healthcare system. We need to acknowledge the fact that diagnostic and therapeutic methods available are also underused in the community.
This review article is the result of witnessing the heart failure in 4 individuals in January 2023. Their symptomsand signs included Shortness of breath with routine activity like walking or household chores, fatigue, and weakness, Pedal oedema, rapid or irregular heartbeat, fluctuating Blood Pressure and Blood sugar levels, reduced ability to exercise and vomiting and aspirational pneumonia. The exponential rise in the incidence of uncontrolled hypertension and DM over the last couple of years has shaped the trajectory of HF development seen today. The key risk factors and causes of HF in our cases included hypertension (HT),â¯diabetes mellitus (DM);â¯chronic kidney disease (CKD). With the bestpossible management practices in cities likeBengaluru and Mysuru in Karnataka we could save only two of the 4 cases,both first-time hospitalized patients.
Materials & Methods:
The third week of January2023 (17-25 January), the author had a misfortune being a witnessfor 3 women and one man between 64-85 years of ageâs hospitalized for CHF with an outcome of 50% of them succumbing to CHF. This manuscript is a review of available information on the websites of World Heart Federation 2020, WHO, Global burden of disease 2019 report, ICC - National Heart Failure Registry, Reports of the Best Charities that fight Heart Diseases in 2023 including American Heart Association, The Childrenâs Heart Foundation, British Heart Foundation, Mended Hearts, Women Heart, Needy heart Foundation Bangalore and published papers in Indiaas evidences.
Introduction
Congestive Heart Failure (CHF/CCF) is a common but complex and heterogenous syndrome and is a global health priority to achieve Universal Health Care (UHC) 2030. CHF underlines the inability of the heart to perform its circulatory function with the desiredefficiency due to structural and/or functional (systolic or diastolic) alterations [1]. In the absence of specific diagnostic criteria, left ventricular ejection fraction (LVEF) is generally considered as a clinicallyuseful phenotypic marker. This criterion is helpful in assessment and sensitive to therapy [2].
Currently, heart failure patients are categorized as a) havingheart failure with reduced (HFrEF;LVEF <40>
The burden of heart failure is increasing at an alarming rate worldwide including India. Heart failure not only increases the risk of mortality, morbidity and worsens the patient’s quality of life, but also puts a huge burden on the overall healthcare system. The management of heart failure has evolved over the years with the advent of new drugsand devices.
Magnitude of CVD & CHF Problems:
Total cardio-vascular diseases (CVD) case prevalence has nearly doubled from 271 million in 1990 to 523 million in 2019, and the number of CVD deaths steadily increased from 12.1 million in 1990, reaching 18.6 million in 2019. The global trends for disability-adjusted life years (DALYs) and years of life lost also increased significantly, and years lived with disability doubled from 17.7 million to 34.4 million over the same period [3]. The incidence of CVDs is equally frequent in men and women worldwide, but a systematic review and meta-analysis of the prevalence of cardiovascular diseases in the geriatric population in India from the year 2003 to 2019 revealed that there was a higher prevalence of cardiovascular diseases in the female geriatric population (40.9%) than the male geriatric population (38.0%) [3].
Overall CCF prevalence from community studies suggest a lowest rate of 0.3%, 0.8% and 1.2% in India, Japan and in Australia and Cuba respectively, while the highest prevalence was reported in Indigenous Australian population (5.3%), Germany (4%) and Canada 3.6%, Turkey 2.9%, and USA 2.6% [1]. CHF is a disease of the “elderly,” frequently occurs in the setting of normal ejection fraction, and has a poor prognosis, regardless of the level of systolic function. The current worldwide prevalence of HF is 8.52 per 1,000 inhabitants, responsible for nearly 10 (9.91) million years lost due to disability (YLDs) and 346.17 billion US $ expenditure [3]. More than 5 persons aged 60 to 69 per 1000 suffer CHF annually and this annual incidence approaches 10 per 1,000 population after 65 years of age.
The signs of a heart failure include- Shortness of breath with activity or when lying down, Fatigue and weakness, swelling in the legs, ankles, and fee, Rapid or irregular heartbeat, reduced ability to exercise, Persistent cough or wheezing with white or pink blood-tinged mucus and Swelling of the abdomen. There has been considerable interest in isolated diastolic dysfunction in recent years, as a substantial number of patients with CHF have normal systolic function.
Case Reports:
Case 1 Mrs. Ranade 85 yrs. This is a lady a known hypertensive and diabetic for last 20 years, but both conditions were reasonably well managed till 2021. Year 2022 saw her getting hospitalized on 3 occasions one for Fracture Femur, other two times for congestive heart failure. She lost her husband about three months ago due to CHF, Parkinsonism, BEP, CKD, bedridden for 4 weeks. After the death of her husband, she was more depressed and lost interest in life and became irregular in taking medicines. On 16 January 2023 she was admitted to a private Hospital in Mysuru with C/o discomfort in chest and difficulty in breathing. On admission BP was 150/68, Pulse was 100/minute and SpO2- 88. There was pitting oedema on feet and legs below knee. LVEF was 46%. An estimated glomerular filtration rate (eGFR) was 46 ml/min per 1.73 square meters for past 3 months. Serum Potassium 8.6, and Sodium (Na) 134mmol/litre. On 18th January 2023 morning she died of heart failure despite following standard protocol.
Case 2. Mrs Ahalyabai 82 years: A known diabetic for 20 years and Hypertensive for last 7 years and Osteo- arthritis for last 4 years restricting her mobility. She had lost her husband 10 years ago due to complications of diabetes after the amputation of left lower limb and had reconciled well. She was admitted to the hospital for a week 6 months ago (mid-2022) for Viral fever and Pneumonia and recovered. Family had fixed a marriage of one of her granddaughters for 26 January 2023. On 18 January 2023 late night around 2200 hrs, as she complained of hunger was fed with 2 Masala dosa’s by the family. Within few hours she vomited 2-3 times, family assuming it to be indigestion gave some home remedies (‘Pitta Dosha’ in Indian system of Medicine is treated by Amla effervescent tablets). As the condition did not improve on 19th January she was hospitalized in a private hospital. On admission her heart rate was 60 per minute and respiratory rate was 14/minute, SpO2- 85% Chest Xray revealed aspirational pneumonia that led to Cardio-renal failure. As she was on beta blockers and Diuretic (Lasix), they were withdrawn but her CHF worsened, and she died around 0930 of 25th January 2023.
Case 3. Mrs Kalavathy 64 yrs.: Another known diabetic patient for over 20 years, that was well managed and Hypertensive for 6 years, under treatment with Bet blockers. She also suffered from osteoarthritis with Pain in Knees, ankles, over year now restricting her exercise routine and was taking NSAID on and off effecting her kidney functioning. She complained of pedal oedema, tiredness and fatigue since a month due to which her daily walking and other social activities got affected. She was put on Lasix a diuretic, that reduced pedal oedema but the weakness and fatigue worsened after a, URI attack (viral flue) in the third week of January 2023. On 23 January 2023 in the current episode she complained of breathlessness, discomfort in the chest, and vomiting. That compelled the family to admit her to a private hospital. On admission she was in an ICU on Oxygen and IV fluid therapy under the care of a cardiologist for 36 hrs and then shifted to a ward. On admission BP was Temperaature-98.20 C, BP= 140/70, Pulse was 50/minute, Respiratory rate- 12/minutes and SpO2- 95%. Bilateral basal Crepitations were heard, CNS was normal. There was bilateral pitting oedema on feet and below knee. ECG showed Sinus Bradycardia, Eco- showed good LV function that led to making a diagnosis of Heart Failure with preserved EF (HFpEF). Blood test indicated hyperkalaemia. In view of bradycardia Atenolol and Ramipril were stopped and treated with diuretics. While the BP and Pulse got stabilized the need for Oxygen supplementation continued for another 24 hrs. She was discharged on 26 January 23 after 3 days of hospitalization prescribing i) Ecospirin AV 75/10 1 tablet in the night, ii) Tab Concor 1.25 mg (Beta blocker- to treat hypertension & stabilize heart rhythm) one tablet in the morning, iii) Tab Dytor 10 mg (a diuretic) One tablet in the morning, iv) Tab Dapanorm 10 mg (SGLT2) on in the afternoon and to continue other anti-diabetes drugs.
Case 4 Chidambar: This is a male patient of 70 years husband of the case no 3. He too is a known diabetic and hypertensive for last 10 years, both conditions poorly managed for last one year. He has been having episodes of vomiting followed by Ketoacidosis twice since January 2023. On 1 February his fasting Blood sugar was 339mg/DL. BP was 177/76 mm Hg. There was a pedal oedema, relieved by diuretics every time. He had left sided hemiparesis and urinary incontinence following stroke one year ago. He is bedridden and depressed most of the days refusing to be disciplined. His LVEF was 50% on 31 December 2022 and continues to be the same.
Discussions
Heart failure, popularly known as congestive heart /cardiac failure (CCF/CHF), occurs when the heart muscle doesn't pump blood as well as it should. When this happens, blood often backs up and fluid can build up in the lungs, causing shortness of breath. There are two types of heart failure i) Left-sided heart failure where the left ventricle of the heart does not pump enough blood around the body ii) Right-sided heart failure: Here the right ventricle of the heart is too weak to pump enough blood to the lungs.
Epidemiology:
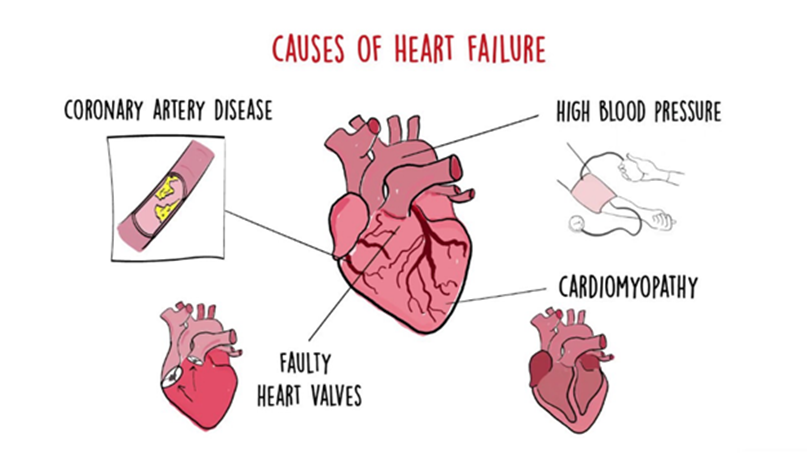
The burden is rapidly increasing, and it is projected that by 2030, the number of HF patients would rise by 25%. The prevalence of HF increases with age, as by 55 years of age, the lifetime risk of HF is 33% and 28.5% for men and women, respectively. The key risk factors and causes of HF include ischemic heart disease (IHD); diabetes mellitus (DM); atrial fibrillation (AF); chronic kidney disease (CKD); valvular heart disease (VHD). From the public health lens one need to consider i) individual CVD risk factors like obesity, hypertension, diabetes, sedentary life, smoking, alcohol consumption and diets leading to hyperlipaemia. ii) emerging risk factors like Amyloidosis, genetic profile of multi-omics iii) multiple-morbidities like Asthma, TB, COPD, musculoskeletal diseases, Cancers etc. iv) Community factors like walking & Gym facilities, neighbourhood safety, poverty, housing, and employment v) health systemic access issues like rural vs urban, gender, caste, advanced diagnostic and therapeutic support vi) Public policies regarding structural issues - food security and vii) Socio-behavioural practices - self efficacy, social isolation, health literacy, childhood experiences, and family structure.

The exponential rise in the incidence of uncontrolled hypertension and DM over the last couple of years has shaped the trajectory of HF development seen today. The overall incidence is likely to increase in the future owing to the Aging population, rising coronary artery disease (CAD) prevalence, epidemic rise of key risk factors such as hypertension and DM, Persistence of Rheumatic and untreated congenital heart disease, rising burden of lung and chronic kidney diseases [4].
Currently available India data indicates that the mortality rate is ∼50% at 5 years from the initial diagnosis of HF. It is a leading cause of hospitalization, representing 1–5% of total hospital admissions. About 2–17% of HF patients admitted to hospital die in the hospital. Patients who survive have a high rate of rehospitalization and poor Quality of Life Despite improvements in medical care over the years, the prognosis of patients with HF remains poor, the survival rate is worse than in those with breast, bowel, or prostate cancers [3,4].
While the prevalence of HF with preserved ejection fraction (HFpEF) is ∼50% (range: 22–73%) of the total HF burden in the Western population, in India it accounts for 25%. [4], indicating that in Indian clinical practice, HFrEF is predominantly observed. The other key observations are Indian patients present with HF at a younger age than those in the West as observed the mean age in the THFR, Medanta Registry and the INTER-CHF (Indian subset) study was 61.2, 58.9 and 56 years, respectively, as compared to 72.4 years in the ADHERE Registry of the USA. The male to female ratio is also different in India (70:30 as per the THFR and 83:17 in the Medanta Registry) compared to USA and Africa (almost 50:50). This may partly reflect that, in India, more males seek healthcare than the females unlike the West.
Criteria for the diagnosis of HFpEF (Heart failure per Ejection Factor): There are different criteria to diagnose CHF. 1. Framingham criteria, widely used and well-validated uses Major and minor signs and symptoms but has Poor sensitivity, especially for early heart failure but Chest X-ray if used has High specificity. 2. 2016 ESC criteria: incorporate signs and symptoms with objective measures of cardiac dysfunction, Natriuretic peptides as they are easy to measure and widely available though many patients with proven HFpEF may have normal natriuretic peptide levels. This is coupled with Echocardiography or other cardiac imaging. EF and diastolic dysfunction as measurement variability of echocardiographic parameters is high. 3. Gothenburg criteria: Uses Symptoms and rales that are easy to apply in primary health care settings and rule out Atrial fibrillation on ECG 4. Boston criteria: Uses signs and symptoms, but heavily relies on dyspnoea, which may be absent in the elderly & Chest X-ray (Adapted from Pfeffer et al). The clinicians in India use i) Symptoms and signs of HF, ii) Normal or near normal LV systolic function and iii) LA volume ≥34 mL/m2, iv) Elevated natriuretic peptides, i.e., BNP >35 pg/mL and/or NT-pro-BNP >125 pg/m along with v) Corroborative evidence such as elevated pulmonary systolic pressure, reduced 6-minute walk-time and increase in mitral E/e’ on modest exercise.
(Notes: HF = heart failure; LV = left ventricular; LA = left atrial; BNP = brain natriuretic peptide; NT-pro-BNP = N-terminal pro-BNP; E/e’ = ratio between early mitral inflow velocity and mitral annular early diastolic velocity)
Aetiology of CHF in India: Though IHD is the most common ethology both in the USA and India, RHD also contributes (accounts for 8% of the burden in the THFR and 5% in the Medanta Registry) in India but not in the USA. The prevalence of risk factors also differs between India and the West. E.g., DM is much more prevalent among Indians than those in the West as per the THFR data. The prognosis of HF in Indian patients appears to be worse than those in the West. The in-hospital mortality observed in the THFR (8.4%) was almost double compared to that reported in the ADHERE registry (4%) of the USA. The INTER-CHF study also showed that the 1-year mortality of HF is high in India around 37%. [2,5]
For clinical and prognosis monitoring the CHF is classified using 3 criteria of i) LVEF ii) Time course and iii) Severity of symptoms as shown in the diagram below
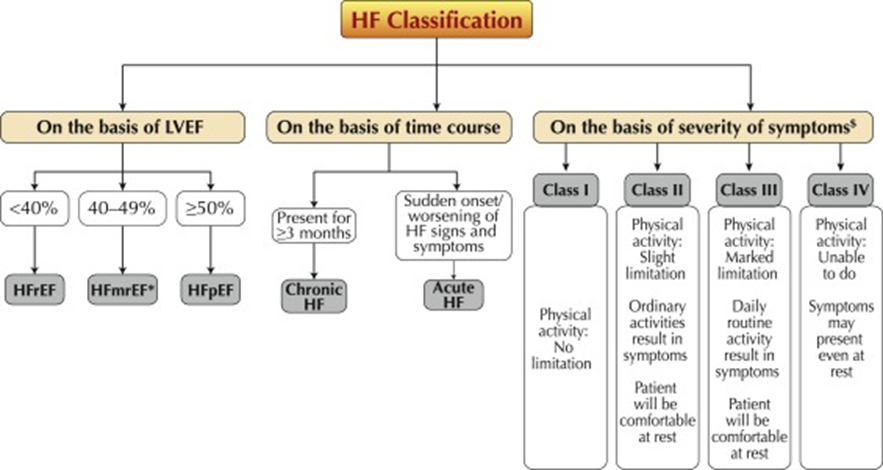
Heart Failures are also classified by clinicians as 1) Stable HF: When a HF patient on treatment does not exhibit any major change in the symptoms and signs of HF for at least one month. 2)Decompensated HF: When the condition of a “chronic” previously “stable” HF patient deteriorates suddenly or slowly, it is referred to as “decompensated”.3) New-onset: A patient with new-onset HF may present with symptoms in an acute or subacute (gradual) fashion. 4) Advanced HF: It refers to patients with severe cardiac dysfunction, recurrent decompensation, and severe symptoms despite optimal standard medical therapy [6].
CVDs & CHFs Situation in India: The overall prevalence of CVDs in the Indian geriatric population as determined in 6586 male and 8164 female subjects from 32 studies, revealed that the prevalence of CVDs in elderly males was 38.0% (95%CI: 33.0%-43.0%) and in elderly females was 40.9% (95%CI: 35.5%-46.2%) [5].
Congestive Heart failure is the commonest cardiac cause for hospitalization with 1% of the general population being affected annually, which adds up to between 8–10 million patients. The 1% average in the general population looks different when only the 65-79 age group is considered where heart failure related hospitalization is 5-10%. In elderly above 80 years of age such hospitalization is even higher at 10-20%. Coronary artery disease (CAD), diabetes, hypertension, valvular heart diseases and primary muscle diseases are the leading causes for heart failure. Rheumatic heart disease is still a common cause of heart failure in Indians. In CADs The disease results from the build-up of fatty deposits in the arteries, which reduces blood flow and can lead to heart attack. Obesity is an additional risk factor [4,5,6].
Hospital-based studies from Trivandrum and All India Institute of Medical Sciences (AIIMS) suggest that rheumatic heart disease (RHD) and coronary artery disease (CAD) are both major causes of heart failure in India. The Trivandrum HF registry of 1205 admissions for HF (834 men, 69%). The mean age was 61.2 years. The most common aetiology of HF was ischemic heart disease (72%). HF with preserved ejection fraction (HFpEF) constituted 26%. In another community-based study from AIIMS, 10,163 adults of six villages in Northern India were screened, and cases of dyspnoea were identified. The prevalence of HF in this rural community was estimated to be 1.2/1000. Two-thirds of the patients had HFpEF and all of them had uncontrolled hypertension (HTN). In another study of 1985 patients from North India the mean age was 49.2 years that is much younger, compared to South Indian patients and still younger than patients of Western India. In the in-hospital group, RHD (52%) was the most common cause followed by ischemic heart disease (17%). RHD (37.1%) was the most common aetiology followed by CAD (33.4%) in a tertiary hospital cohort. One reason for the higher rates of RHD could be due to the referral bias of patients from the low socioeconomic sector to public sector hospitals where the study was conducted [4].
Actions being taken in India:
There is paucity of good and reliable data in India on heart failure in the country. A true and meaningful national data identifying the risk factors, available treatment options, and challenges in management could be addressed is the need of the time. The correlation between the improvements that have been made in the treatment of coronary artery disease, and the incidence of heart failure is intriguingly counter intuitive. Heart failure has increased rather than decreased and needs careful investigation.
The Indian College of Cardiology (ICC) - National Heart Failure Registry (A registry for acute decompensated heart failure patients in India) was formally registered on August 28, 2019 and cases enrolled since September 01, 2019, onwards. Between August 01, 2018, to August 31, 2020, twenty-two (22) Centre's from 12 states were enrolled and 5279 patients were enrolled in an effort to get a national profile [4].

Way Forwards:
A study monitoring progress of live cases over a period along with data storage and analysis is the need of the time and may reveal the causes. It needs to include the incidence, aetiology, diagnosis, and treatment patterns encompassing a population diverse in geography, age, gender, and socio-economic class. It is important to study the incidence of co-morbid risk factors like, diabetes, hypertension, and dyslipidaemia. This must be achieved in phases.
References
- Global epidemiology and future trends of heart failure, Giuseppe Lippi et.al (June 2020).
- Epidemiology of heart failure, Amy Groenewegen et.al.
- Global Burden of Cardiovascular Diseases and Risk Factors: Gregory A. et.al (1990–2019).
- ICC - National Heart Failure Registry, Current Situation.
- Gender prevalence of cardiovascular diseases in the geriatric population of India: A meta-analysis, Nanda H, et.al, 8(1): 15-26 [DOI: 10.13105/wjma. v8.i1.15].
- Management protocols for chronic heart failure in India, S. Mishra et.al (January–February 2018), Indian Heart Journal, Volume 70, Issue 1, Pages 105-127.


