Archive : Article / Volume 1, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-8649/001
Dental Infections and Risk for Brain Abscess: A Literature Review
1.College of Medicine, Florida State University, Tallahassee, FL 32304, USA.
2.College of Medicine, University of Florida, Gainesville, FL 32611, USA.
3.Department of Neurosurgery, University of Florida, Gainesville, FL 32601, USA.
Brandon Lucke-Wold
Greggory D. B., II, M. A. Llerena, D. J. Gorelov, M. T. Alkaelani, J. R. Goeckeritz, and B. Lucke-Wold, (2022). Dental Infections and Risk for Brain Abscess: A Literature Review. Journal of Dental and Oral Care. 1(1). DOI: 10.58489/2836-8649/001.
© 2022 B. Lucke-Wold, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 26-10-2022
- Accepted Date: 07-11-2022
- Published Date: 19-12-2022
brain abscess; dental; infection; oral flora; immunocompromised; needle aspiration; surgical excision; antibiotics; congenital heart defects
Abstract
Dental work is commonly accepted as a low-risk procedure but has been associated with serious brain abscesses. Bacteria from the oral cavity can spread to the brain and cause life-threatening infections. In this literature review, the focus was placed on the relevant causative bacteria, surgical procedures, and correlated medical conditions revolving around brain abscesses following dental work. This paper is written from a neurological surgery perspective, using information collected from several case studies, case reviews, and other related published manuscripts. Several risk factors have been identified to predispose oral cavity bacterial infection to cause brain abscess: dental work done in the upper molars; right-to-left shunts in the heart; and poor dental hygiene. If the bacterium of the abscess is correctly identified, there is a greater effectiveness of treatment, but prolonging antibiotic and/or surgical treatment increases morbidity.
Introduction
Numerous bacterial strains populate the natural flora of the oral cavity, with certain strains capable of spreading to the brain following odonatological procedures [1]. Specifically, it was discovered that dental plaque can contain about 350 different possible bacterium types [2]. Odonatological bacterial infection spreading to cause a brain abscess is a very unlikely outcome of dental work, yet the sheer number of dental procedures done every year elicits a clear indication that understanding the etiology of this unique occurrence is worth consideration. Incidence of brain abscess in developed countries is 0.3-0.9 per 100,000 habitants with mortality between 17% and 37% [3]. Although the treatment of brain abscesses has well established treatment protocols, the understanding behind what factors predispose patients to odontogenic infections to become brain abscesses is lacking [4]. This literature review covers current published work regarding brain abscess causing bacteria arising from the oral cavity. The breadth of this manuscript focuses on the causative organisms, surgical evacuations, predisposing factors, and subsequent medical management of bacterial brain abscesses.
Methods
Pre-defined search terms were used to search PubMed from inception to 17 September 2022. 193 results showed with “Brain abscess oral,” then 64 results showed with “Brain abscess dental infection.” The search terms included ("Brain abscess"[Mesh]) AND "Dental infection”. Included in the study were all original, peer-reviewed studies that reported on the development of brain abscess due to dental infection. All published manuscripts before 2003 were excluded from our review, allowing focus on modern treatment. Abstracts and studies not easily translated into the English language were excluded from the study. This included a title and abstract screening, followed by a full-text review and subsequent data extraction step, narrowing the pool of studies to 43. All articles used had free full article access, allowing simple reference material for subsequent reader reference analysis.
Data extraction was done via Microsoft Excel®, and included information on study design, causative organism, predisposing factors, proposed treatment approach, surgical evacuation, and subsequent medical management. Then the articles were cited in order of use in the most logical pattern of literature review progression.
Microbial Infection, Identification, and Proposed treatment
Odontogenic infections, procedures, and trauma have been linked with the development of brain abscesses in unique instances [5,6]. Infection of the upper molars and surrounding gingiva has been correlated to a high risk of developing brain abscess - see Figure 1 [7]. The natural oral flora is the most common cause of subsequent brain infections, specifically Streptococcus species and mixed anaerobes (such as Anaerococcus prevotii) [3,4] . Streptococcus intermedius causes approximately 50-80% of bacterial brain abscesses; along with placing immunocompromised patients at higher risk for thalamic abscesses [8–10]. Streptococcus viridans have been demonstrated to cause brain abscess in patients with infected pulp [11]. One descriptive and comparative metagenomic study showed how there was a 65.5% overlap between microorganism species of empyemas and brain abscesses, with Streptococcus intermedius, Fusobacterium nucleatum and Aggregatibacter aphrophilus being the most common pathogens [12]. Additionally, an immunocompromised status is a predisposing factor for developing brain-related infections [8,11,13].
Odontogenic brain abscesses from oral origin have been reported in neonatal and pediatric cases. In addition to those above, common pathogens affecting neonates include bacteria from the Proteus, Citrobacter, and Enterobacter genuses. In children with compromised immune systems the most common agents predisposing brain abscess development are from the Nocardia spp., Mycoplasma tuberculosis, Eikenella corrodens, and certain fungi species [11,14]. In addition, Streptococcus viridans and Prevotella spp. have been associated with the development of brain abscesses in neonatal and pediatric patients with pre-existing or congenital cardiovascular defects such as patent foramen ovale (PFO) [15].
Other organisms associated with periodontal disease, dental caries, and poor oral condition that can lead to brain abscess in adults include Bacteroides, Actinomyces meyeri, Porphyromonas gingivalis, Pseudomonas aeruginosa, Fusobacterium, Aggregatibacter actinomycetemcomitans, Prevotella spp., and Mycoplasma salivarium - see Table 1 [3,11,15–21]. Some case studies have described unsuspecting diseases such as group-A streptococcal pharyngitis leading to brain abscess that could be prevented by diagnoses and therapy of Streptococcus pyogenes infection [22]. These bacteria highlight the wide spectrum of microorganisms that can play a role in the advent of a brain abscess.
Brain abscess can be challenging to diagnose on clinical symptoms alone as its presentation could be due to other etiologies. Common presentations include headaches, fever, altered mental status, decreased consciousness, seizures, cerebellar involvement, as well as the constellation of abdominal pain, nausea, vomiting, and diarrhea [6,16,23]. The characteristic triad of headache, fever, and focalization only occurs in 20-30% of cases [14].
Computed Tomography (CT) is the preferred scanning method, although sometimes Magnetic Resonance Imaging (MRI) is used to give more detailed images [11]. Although treatment can be started without the isolation of the specific pathogen causing the brain abscess, having an identified microbial pathogen can help identify the best treatment for the patient [7]. Gram staining, culture, and histopathology are the preferred methods for accurately identifying the pathogen [8,9,11,16,23,24]. In addition, the use of matrix-assisted laser desorption/ionization time-of-flight (MALDI-TOF) technology has led to the rapid identification of microorganisms. MALDI-TOF tech uses computerized scans analyzed through computer algorithms to rapidly identify bacteria [23].
Additionally, bacterial brain abscesses from oral cavity bacteria can occur following intracranial surgical procedures. In cases of trauma related to procedures or surgeries to the brain, Staphylococcus aureus is the most common pathogen amongst post-surgical brain abscesses. The second most likely bacteria for post-surgical abscesses are Streptococci spp. and Enterobacteriaceae spp. genuses of bacteria [11]. The risk of surgical procedures within the skull includes the possibility of introducing other pathogens, which may respond to different antibiotic treatments and require alternative subsequent management. Thus, the neurosurgical drainage approach is only added to the antibiotic treatment when there is sufficient size of tumor to use more than antibiotics, due to the risk the procedure itself can present [12,25].
Surgical Evacuation, Alternative Treatments, and Subsequent Management
Once identified on CT or MRI treatment of brain abscesses follow a well-established methodology as seen in Figure 2 [25]. Though ordering of steps may vary on a case-by-case basis, major considerations include when antibiotic treatment is given, medication choice accounting for patient allergies, and the number of neurosurgeries (drainage) needed for the patient [25].
For brain abscesses greater than 1 cm in size, treatment first consists of draining the abscess, either by needle aspiration or surgical excision, and then administering broad-spectrum antimicrobial therapy [1,26]. However, effective treatment of brain abscesses relies on identifying the underlying bacteria causing the abscess [4,19]. Correct identification the bacteria allows for the use of the most effective antibiotic, thereby minimizing drug resistance. Brain abscesses smaller than 1 cm in size, are treated using antibiotics without the need for surgical resection [27-28].
Abscess drainage being part of the neurosurgical treatment has demonstrated benefits on its own [11,28]. Surgical excision and neurosurgical aspiration of the brain abscess is helpful as it can prevent the infection from spreading to nearby tissue and help identify the type of bacteria causing the abscess [4,29]. Furthermore, the earlier the causative agent is identified, the more effective the treatment will be in reducing mortality rates and improving the overall prognosis [30]. Stereotactic-guided aspiration is the most common procedure for draining a singular abscess larger than 1cm in diameter and is performed by drilling a burr hole for fluid drainage of the brain abscess. Whereas, total surgical resection by craniotomy is a procedure reserved for larger, multi-lobulated abscesses with severe intracranial hypertension [19].
Upon consistent inspection of the abscess site, any indications of bacterial growth or site inflammation is treated with antibiotics post-surgery [18,25]. If the underlying cause cannot be identified, brain abscesses should be treated empirically with Ceftriaxone 2 g twice daily, Vancomycin 1 g three times daily, and Metronidazole 500 mg four times daily [1,31]. Alternative broad-spectrum IV antibiotics include Ampicillin with Sulbactam or oral Amoxicillin with Clavulanate [8,13,16,28]. Treatment may also include Amphotericin B to cover possible fungal pathogens, rifampin for resistant microbes, metronidazole as an additional antibiotic, and corticotherapy to reduce inflammation [24]. Multiple surgical treatments may be required if upon repeat MRI inspection the abscess is shown attempting to reform or if more abscesses arise [32].
Antimicrobial therapy is determined post-surgery, after the abscess and tissue specimens extracted are analyzed by a microbiology department and antibiotic susceptibility tests are carried out [4,30]. Once the antibiotic therapy is started, imaging studies (i.e. MRI or CT specific) focusing on changes in the size of the lesion, edema and mass effect should be performed weekly to evaluate the effectiveness of the antimicrobial therapy [14,19]. Using appropriate antibiotic therapy, the abscess should decrease in size within 1-4 weeks however the radiological resolution could take up to 16 weeks. Until abscess and overall infection has fully resolved multiple rounds of antibiotics and surgeries may be required, potentially retaining the patient for months of hospital stay. Typically, antibiotics are given for six to eight weeks following correct bacterial identification of the brain abscess [33]. Additional nosocomial diseases are prevented via personal protective equipment and possible visitation restrictions, especially with immunocompromised patients [4,8,11,22,34].
Discussion
Brain abscesses typically occur in the frontotemporal, frontal-parietal, parietal, and cerebellar-occipital lobe areas of the brain - see Figure 3 [35]. This is most likely attributed to the middle meningeal artery transportation of the bacteria to the brain being the most likely route of bacterial flow, with posterior communicating artery being the less likely alternate route of travel. Along with the frontal and temporal lobes being physically closer to the nasopharynx and oral cavity.
Brain abscess due to dental infections may be predisposed in certain patients with preexisting conditions such as right-to-left shunts that can be seen in a PFO, thoracic venous anomalies, Ebstein’s anomaly, and venosus atrial septal defects [12,34,36-37]. Dental procedures, such as dental scaling, done to these vulnerable patients can increase the risk of a brain abscess due to veno-arterial seeding.
Odontogenic brain abscesses may include extra intermediate steps as the bacteria spreads from the oral cavity, such as sinusitis. Bacterial and fungal sinusitis can lead to orbital, intracranial, and osseous extra-sinus complications with odontogenic sinusitis being the most prevalent cause of operative extra-sinus infectious complications [38]. Patients at risk for extra-sinus spread have bony wall defects and may increase the likelihood of brain abscess. Odontomas that obstruct sinus drainage can lead to a potential brain abscess [39]. More can be understood about this possible oral cavity infection to brain abscess through sinusitis in alternative studies such as in Douglas et al, 2022.
Dental work primarily focuses on dental extractions and dealing with teeth root infections, but there are additional odontogenic problems that can cause bacterial brain abscesses [20]. Oral carcinoma, as an example, can contribute to brain abscess in certain circumstances. One retrospective study showed how carbon-ion radiotherapy for major salivary gland carcinoma had an associated late toxicity that led to a rare case of a grade 3 brain abscess [40].
Possible pre-clinical prevention includes maintaining excellent oral hygiene, screening for congenital heart defects leading to right-to-left shunting, prompt treatment of dental infections, and treatment of sinusitis. Dentists have an integral role in the proper diagnosis of oral cavity infections that could spread to the brain. These diagnoses can often be made with radiographic films in dental offices, which allows early prevention and treatment of brain abscesses [5]. During regular dental cleanings and regular X-ray scans at dental offices, keen awareness of oral infections can prevent their spread. Antibiotic prophylaxis may be considered for patients that have several periodontal treatments, and extraction of teeth to prevent inflammation may be needed as seen in one unsuspecting healthy individual that presented with a brain abscess [41].
Patients that present with a brain abscess with an unknown source should obtain a transthoracic echocardiography in order to rule out a congenital heart defect of a right-to-left shunt cause, even with elderly patients [34]. An atypical, proposed treatment for brain abscesses is hyperbaric oxygen therapy due to its helpful physiological effects and better outcomes [42]. Hyperbaric oxygen therapy should only be considered after first-line treatment is exhausted and the patient is determined to be in stable condition [42].
Early diagnosis and appropriate treatment of brain abscesses is one area that needs improvement, since delaying treatment negatively affects patient outcome [43]. Brain abscesses due to odontogenic origin typically show nonspecific symptoms, therefore these types of cases are usually delayed in diagnosis and management [2]. One study reported a change in patient mortality from 40% to 10% when the brain abscess is identified and treated in a timely manner [33]. Misdiagnosis is a concern that can delay treatment. Patients with dental infections should be treated promptly and aggressively to prevent the potential risk of complications such as a brain abscess. Patients should be counseled on keeping good oral hygiene, recognizing symptoms, and having good communication between physicians and dental specialists. Future care for the patients in recovery from a brain abscess is individualized by a case-by-case basis with options including various antibiotic therapy duration, antiepileptics, surgery to fix congenital heart defects, and dental treatment. Advancements in imaging and the advancement of novel antibiotics are helping reduce poor complications and mortality from brain abscesses; from a 40-60% mortality rate in the pre-CT era to a 0-10% mortality rate currently [43].
Conclusion
Several bacteria were identified as sources of brain abscesses over a variety of cases. The treatment protocols of surgery and medication usage are largely dependent on the specific bacteria cultured out of the abscess, using MRIs to check how the bacteria react to treatment. Congenital heart defects (like PFO), immunocompromised condition, and dental work in the upper molars were associated with brain abscess formation. Correctly identifying the bacteria of the brain abscess is correlated with a more effective antibiotic and/or surgical treatment. Though an uncommon complication, odontogenic bacteria spread following dental work to form brain abscesses, is a real and well published relationship. The communication of dental and medical professionals assists in early detection of this possible outcome of dental work, possibly lowering brain abscess occurrence.
Obtaining cause-and-effect relationships between brain abscesses and odontogenic bacteria is the major limiting factor in this study. Even in murine models, the rare occurrence of brain abscesses would make cause-and-effect relationships difficult to prove. Limitations of X-rays in dental offices limit the detection of brain abscesses without CT or MRI examination, restricting early detection of brain abscesses. Possible protocol implementation of giving head CT scans for hospital patients with odontogenic infections may be warranted for brain abscess detection. More reporting of odontogenic-origin brain abscesses is warranted for future possible systematic reviews and meta-analysis studies.
Table and Figures
Findings | Source | |
Streptococcus spp. & mixed anaerobes like Anaerococcus prevotii | Normal flora and common cause of brain abscess | Sasmanto et al. 2022 [3,4] |
Sreptococcus intermedius | Most common brain abscess forming bacteria | Basyuni et al. 2015 [8-10] |
Streptococcus viridans | Correlated with infected pulps leading to brain abscess | AlHarmi et al. 2018 [11] |
Staphylococcus aureus | Most common cause of post-surgical brain abscesses | |
Streptococcus viridans | Associated with brain abscesses in neonatal patients with congenital cardiovascular defects | Akimoto et al. 2018 [15] |
Prevotella | ||
Eikenella corrodens | Predisposing agents to brain abscesses in immunocompromised pediatric patients | Valdes-de la Torre et al. 2017 [11,14] |
Mycobaterium tuberculosis | ||
Nocardia | ||
Actinomyces meyeri | Other organisms documented to cause brain abscess in adults | Kichenbrand et al. 2020; Funakoshi et al. 2020 [3,11,15-20] |
Aggregatibacter actinomycetemcomitans | ||
Fusobacterium | ||
Mycomplasma salivarium | ||
Peptostreptococcus | ||
Porphyromonas gingivalis | ||
Pseudomonas aeruginosa | ||
Streptococcus pyogenes |
Table 1. Summary of brain abscess causing organisms and cited papers.
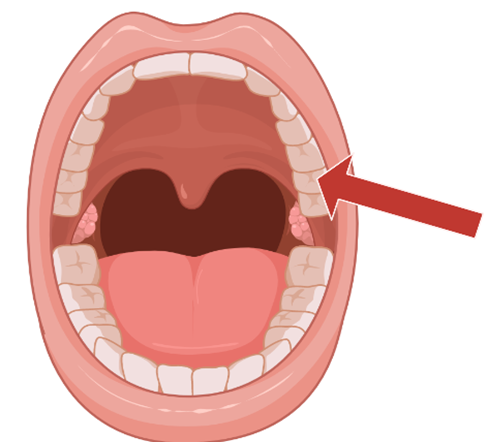
Figure 1: shown below is a visual depiction of the upper molar area of the mouth, where dental work is most highly correlated with odontogenic bacterial brain abscesses [7].
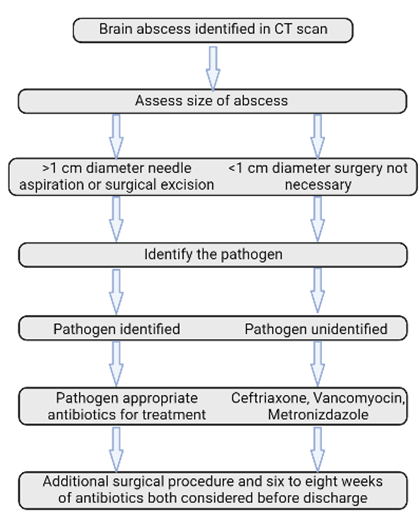
Figure 2: This is a flowchart of the Surgical Evacuation section of this literature review. Shown are the steps of brain abscess treatment following the discovery of the Brain abscess (via CT scan). First the abscess size is taken into consideration, then the pathogen is attempted to be identified, then antibiotics and possible additional surgeries are considered.
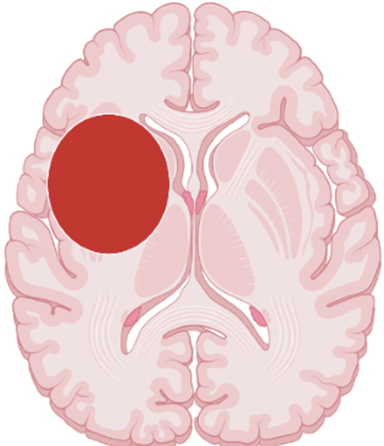
Figure 3: Shows the most common area for a frontotemporal brain abscess to occur [35]. The red circle on the coronal view of this brain image denotes where the frontal, parietal, and temporal lobes intersect as a common place abscess form.
References
- Burgos-Larraín, L.F.; Vázquez-Portela, Á.; Cobo-Vázquez, C.M.; Sáez-Alcaide, L.M.; Sánchez-Labrador, L.; Meniz-García, C. (2022), Brain Complications from Odontogenic Infections: A Systematic Review. J Stomatol Oral Maxillofac Surg, S2468-7855(22)00206-3, doi:10.1016/j.jormas.2022.07.018.
- Ben Hadj Hassine, M.; Oualha, L.; Derbel, A.; Douki, N. (2015), Cerebral Abscess Potentially of Odontogenic Origin. Case Rep Dent, 2015, 267625, doi:10.1155/2015/267625. 3.
- Kichenbrand, C.; Marchal, A.; Mouraret, A.; Hasnaoui, N.; Guillet, J.; Rech, F.; Phulpin, B. (2020), Brain Abscesses and Intracranial Empyema Due to Dental Pathogens: Case Series. Int J Surg Case Rep, 69, 35–38, doi:10.1016/j.ijscr.2020.03.025. 4.
- Sasmanto, S.; Wasito, E.B. (2022), Odontogenic Brain Abscess Due to Anaerococcus Prevotii Infections: A Case Report and Review Article. Int J Surg Case Rep, 97, 107450, doi:10.1016/j.ijscr.2022.107450. 5.
- Arslan, F.; Karagöz, E.; Arslan, B.Y.; Mert, A. (2016), An Unnoticed Origin of Fever: Periapical Tooth Abscess. Three Case Reports and Literature Review. Infez Med, 24, 67–70. 6.
- Greenstein, A.; Witherspoon, R.; Leinkram, D.; Malandreni, M. (2015), An Unusual Case of a Brain Abscess Arising from an Odontogenic Infection. Aust Dent J, 60, 532–535, doi:10.1111/adj.12266.
- Lisboa, E. de C.C.; Silva, W.O.; Rodrigues, R.C.V.; Brum, S.C.; Alves, F.R.F. (2022), The Connection between Brain Abscess and Odontogenic Infections: A Systematic Review. Arch Oral Biol, 135, 105360, doi:10.1016/j.archoralbio.2022.105360. 8.
- Hanna, A.; Imam, Z.; Odish, F.; Dalal, B. (2020), Multiple Liver Abscesses Caused by S Treptococcus Intermedius Bacteremia in the Setting of a Routine Dental Cleaning. BMJ Case Rep, 13, e233097, doi:10.1136/bcr-2019-233097. 9.
- Basyuni, S.; Sharma, V.; Santhanam, V.; Ferro, A. (2015), Fatal Thalamic Abscess Secondary to Dental Infection. BMJ Case Rep, 2015, bcr2015212589, doi:10.1136/bcr-2015-212589.
- Takahashi, S.; Segoe, H.; Kikuiri, T.; Maruo, Y.; Sato, T.; Watanabe, Y.; Jimei, Z.; Yoshimura, Y.; Ishiyama, M.; Takeda, A.; et al. (2022), A Rare Case of Multiple Brain Abscesses Caused by Apical Periodontitis of Deciduous Teeth in Congenital Heart Disease: A Case Report. BMC Oral Health, 22, 261, doi:10.1186/s12903-022-02294-z. 11.
- AlHarmi, R.A.; Henari, D.F.; Jadah, R.H.S.; AlKhayyat, H.M. (2018), A Brain Populated with Space-Occupying Lesions: Identifying the Culprit. BMJ Case Rep, 2018, bcr-2018-224286, doi:10.1136/bcr-2018-224286. 12.
- Kawase, S.; Okada, Y.; Isono, K.; Iwasaki, H.; Kuno, T.; Matsumura, K.; Fu, Y.; Harada, Y.; Ogasawara, T. (2019), Cerebral Abscess Following the Self-Extraction of Teeth in Patient with Ebstein’s Anomaly: A Case Report. BMC Oral Health, 19, 200, doi:10.1186/s12903-019-0893-3. 13.
- Clifton, T.C.; Kalamchi, S. (2012), A Case of Odontogenic Brain Abscess Arising from Covert Dental Sepsis. Ann R Coll Surg Engl, 94, e41-43, doi:10.1308/003588412X13171221499667. 14.
- Valdés-de la Torre, G.E.; Martínez-Bustamante, M.E. (2020), [Cerebral abscess due to Eikenella corrodens in an immunocompetent pediatric patient]. Bol Med Hosp Infant Mex, 78, 136–142. 15.
- Akimoto, Y.; Yanaka, K.; Onuma, K.; Nakamura, K.; Ishikawa, E. (2021), Prevotella Brain Abscess in a Healthy Patient with a Patent Foramen Ovale: Case Report. Surg Neurol Int, 12, 548, doi:10.25259/SNI_783_2021. 16.
- Funakoshi, Y.; Hatano, T.; Ando, M.; Chihara, H.; Takita, W.; Tokunaga, K.; Hashikawa, T.; Kamata, T.; Higashi, E.; Nagata, I. (2020), Intracranial Subdural Abscess Caused by Actinomyces Meyeri Related to Dental Treatment: A Case Report. NMC Case Rep J, 7, 135–139, doi:10.2176/nmccrj.cr.2019-0246. 17.
- Brook, I. (2006), Microbiology of Intracranial Abscesses Associated with Sinusitis of Odontogenic Origin. Ann Otol Rhinol Laryngol, 115, 917–920, doi:10.1177/000348940611501211. 18.
- Clancy, U.; Ronayne, A.; Prentice, M.B.; Jackson, A. (2015), Actinomyces Meyeri Brain Abscess Following Dental Extraction. BMJ Case Rep, 2015, bcr2014207548, doi:10.1136/bcr-2014-207548. 19.
- Pereira, R.S.; Bonardi, J.P.; Ferreira, A.; Latini, G.L. (2017), An Unusual Case of Dental Infection by Pseudomonas Aeruginosa Causing a Brain Abscess: Case Report. Aust Dent J, 62, 523–527, doi:10.1111/adj.12539. 20.
- Henrich, B.; Rumming, M.; Sczyrba, A.; Velleuer, E.; Dietrich, R.; Gerlach, W.; Gombert, M.; Rahn, S.; Stoye, J.; Borkhardt, A.; et al. (2014), Mycoplasma Salivarium as a Dominant Coloniser of Fanconi Anaemia Associated Oral Carcinoma. PLoS One, 9, e92297, doi:10.1371/journal.pone.0092297. 21.
- Rahamat-Langendoen, J.C.; van Vonderen, M.G.A.; Engström, L.J.; Manson, W.L.; van Winkelhoff, A.J.; Mooi-Kokenberg, E.A.N.M. (2011), Brain Abscess Associated with Aggregatibacter Actinomycetemcomitans: Case Report and Review of Literature. J Clin Periodontol, 38, 702–706, doi:10.1111/j.1600-051X.2011.01737.x. 22.
- Costantinides, F.; Luzzati, R.; Tognetto, D.; Bazzocchi, G.; Biasotto, M.; Tirelli, G.C. (2012), Rapidly Progressing Subperiosteal Orbital Abscess: An Unexpected Complication of a Group-A Streptococcal Pharyngitis in a Healthy Young Patient. Head Face Med, 8, 28, doi:10.1186/1746-160X-8-28. 23.
- Sah, R.; Nepal, G.; Sah, S.; Singla, S.; Upadhyay, P.; Rabaan, A.A.; Dhama, K.; Rodriguez-Morales, A.J.; Ghimire, R. (2020), A Rare Case of Brain Abscess Caused by Actinomyces Meyeri. BMC Infect Dis, 20, 378, doi:10.1186/s12879-020-05100-9. 24.
- Hibberd, C.E.; Nguyen, T.D. (2012), Brain Abscess Secondary to a Dental Infection in an 11-Year-Old Child: Case Report. J Can Dent Assoc, 78, c49. 25.
- Bodilsen, J.; Duerlund, L.S.; Mariager, T.; Brandt, C.T.; Petersen, P.T.; Larsen, L.; Hansen, B.R.; Omland, L.H.; Tetens, M.M.; Wiese, L.; et al. (2022), Clinical Features and Prognostic Factors in Adults with Brain Abscess. Brain, awac312, doi:10.1093/brain/awac312. 26.
- Amorim, R.P.; Henriques, V.M.; Junior, F.T.; Reis, V.G.; Bulhões, S.O. (2022), Hydrocephalus and Intracranial Hypertension by an Odontogenic Brain Abscess. Cureus, 14, e26945, doi:10.7759/cureus.26945. 27.
- Prieto, R.; Callejas-Díaz, A.; Hassan, R.; de Vargas, A.P.; López-Pájaro, L.F. (2020), Parvimonas Micra: A Potential Causative Pathogen to Consider When Diagnosing Odontogenic Brain Abscesses. Surg Neurol Int, 11, 140, doi:10.25259/SNI_20_2020. 28.
- Dai, T.-G.; Ran, H.-B.; Qiu, Y.-X.; Xu, B.; Cheng, J.-Q.; Liu, Y.-K. (2019), Fatal Complications in a Patient with Severe Multi-Space Infections in the Oral and Maxillofacial Head and Neck Regions: A Case Report. World J Clin Cases, 7, 4150–4156, doi:10.12998/wjcc.v7.i23.4150. 29.
- Shibata, T.; Hashimoto, N.; Okura, A.; Mase, M. (2021), Brain Abscess of Odontogenic Origin in Patients with Malignant Tumors: A Report of Two Cases. Surg Neurol Int, 12, 417, doi:10.25259/SNI_541_2021. 30.
- Pereira, A.J. da S.P.R.; Tavares, A.T.; Prates, M.; Ribeiro, N.; Fonseca, L.F.; Marques, M. do R.; Proença, F. (2022), Brain Abscess: A Rare Clinical Case with Oral Etiology. Case Rep Infect Dis, 2022, 5140259, doi:10.1155/2022/5140259. 31.
- Tsonis, I.; Karamani, L.; Xaplanteri, P.; Kolonitsiou, F.; Zampakis, P.; Gatzounis, G.; Marangos, M.; Assimakopoulos, S.F. (2018), Spontaneous Cerebral Abscess Due to Bacillus Subtilis in an Immunocompetent Male Patient: A Case Report and Review of Literature. World J Clin Cases, 6, 1169–1174, doi:10.12998/wjcc.v6.i16.1169. 32.
- Costa Mendes, L.; Vaysse, F.; Maret, D. (2020), Brain Abscess Secondary to a Dental Infection. Case Rep Emerg Med, 2020, 3248174, doi:10.1155/2020/3248174. 33.
- Al Moussawi, H.; Krzyzak, M.; Awada, Z.; Chalhoub, J.M. (2018), Streptococcus Intermedius Brain and Diverticular Abscesses After Dental Manipulation: A Case Report. Cureus, 10, e2061, doi:10.7759/cureus.2061. 34.
- Alhamshari, Y.S.M.; Punjabi, C.; Pressman, G.S.; Govil, A. (2015), Sinus Venosus Atrial Septal Defect Presenting with Brain Abscesses in a 77-Year-Old Immunocompetent Patient. BMJ Case Rep, 2015, bcr2015212165, doi:10.1136/bcr-2015-212165. 35.
- Bokhari, M.R.; Mesfin, F.B. (2022), Brain Abscess. In StatPearls; StatPearls Publishing: Treasure Island (FL). 36.
- Pettersson, S.; Trzebiatowska-Krzynska, A.; Engvall, J. (2022), An Uncommon Case of Congenital Thoracic Venous Anomaly and Extracardiac Sinus Venosus Defect in an Asymptomatic Adult First Presenting with Brain Abscesses: A Case Report. Eur Heart J Case Rep, 6, ytac052, doi:10.1093/ehjcr/ytac052. 37.
- Horiuchi, Y.; Kato, Y.; Dembo, T.; Takeda, H.; Fukuoka, T.; Tanahashi, N. (2012), Patent Foramen Ovale as a Risk Factor for Cryptogenic Brain Abscess: Case Report and Review of the Literature. Intern Med, 51, 1111–1114, doi:10.2169/internalmedicine.51.7133. 38.
- Douglas, J.E.; Patel, T.; Rullan-Oliver, B.; Ungerer, H.; Hinh, L.; Peterson, E.L.; Kohanski, M.A.; Kennedy, D.W.; Palmer, J.N.; Adappa, N.D.; et al. (2022), Odontogenic Sinusitis Is a Common Cause of Operative Extra-Sinus Infectious Complications. Am J Rhinol Allergy, 19458924221114940, doi:10.1177/19458924221114941. 39.
- Gupta, M.; Das, D. (2015), Extensive Complex Odontoma in the Maxillary Sinus Pushing 3rd Molar near the Orbital Floor Causing Transient Diplopia and Chronic Sinusitis: A Rare Presentation and Surgical Management. J Maxillofac Oral Surg, 14, 338–340, doi:10.1007/s12663-013-0561-0.
- Hayashi, K.; Koto, M.; Demizu, Y.; Saitoh, J.-I.; Suefuji, H.; Okimoto, T.; Ohno, T.; Shioyama, Y.; Takagi, R.; Ikawa, H.; et al. (2018), A Retrospective Multicenter Study of Carbon-Ion Radiotherapy for Major Salivary Gland Carcinomas: Subanalysis of J-CROS 1402 HN. Cancer Sci, 109, 1576–1582, doi:10.1111/cas.13558. 41.
- Woelber, J.P.; Kruse, A.; Hanna, G.; Ermer, M.; Beringer, A.; Ratka-Krueger, P. (2016), Gehirnabszess nach parodontaler Therapie. Ein Fallbericht über einen Gehirnabszess assoziiert mit Fusobacterium nucleatum nach parodontaler Therapie. Swiss Dent J, 126, 921–927. 42.
- M Das, J.; Tommeraasen, M.A.; Cooper, J.S. (2022), Hyperbaric Evaluation and Treatment Of Intracranial Abscess. In StatPearls; StatPearls Publishing: Treasure Island (FL). 43.
- Park, S.Y.; Suh, D.W.; Park, C.M.; Oh, M.S.; Lee, D.-K. (2014), Brain Abscess Due to Odontogenic Infection: A Case Report. J Korean Assoc Oral Maxillofac Surg, 40, 147–151, doi:10.5125/jkaoms.2014.40.3.147.


