Article In Press : Article / Volume 3, Issue 1
- Research Article | DOI:
- https://doi.org/DOI: 10.58489/2836-3604/014
Evaluation Of Renal Biomarkers During Coronavirus-2 Infection Of Severe Acute Respiratory Syndrome
1Laboratory of Biochemistry and Molecular Biology, Faculty of Medicine, Pharmacy and Odontology, Cheikh Anta Diop University of Dakar, Senegal
2Laboratory of Biochemistry, Aristide Le Dantec Hospital, Senegal
3Laboratory of Biochemistry, Dalal Djam Hospital, Senegal
4Laboratory of Biology, Abass Ndao Hospital, Senegal
5UFR health of Thiès, Senegal
6National Hospital Center Cheikh Ahmadoul Khadim, Senagal
Ndiaye A*
Ndiaye A, et.al. (2024). Evaluation Of Renal Biomarkers During Coronavirus-2 Infection Of Severe Acute Respiratory Syndrome. Covid Research and Treatment. 3(1). DOI: 10.58489/2836-3604/014
© 2024 Ndiaye A, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 27-07-2024
- Accepted Date: 03-08-2024
- Published Date: 05-08-2024
Covid-19, kidney disease
Abstract
Introduction : In December 2019, an outbreak of coronavirus disease 2019 (COVID-19) occurred in Wuhan, Hubei Province, China. It quickly spread to other parts of the world. Advances in the field of pathophysiology have shown that co-expression of angiotensin-converting enzyme 2 (ACE 2) receptors and TMPRSS proteases are required for virus entry into the host cell. Direct renal involvement of the virus was therefore strongly suspected due to the high concentration of these receptors at the renal level, particularly at the level of the proximal tubule.
Materials and Method : This was a prospective, descriptive and analytical study of patients infected with SARS-CoV2. For each patient, blood samples were taken on a heparin tube or dry tube for the determination of parameters (albumin, creatinine, urea, Na+ K+) with the Abbott ARCHITECT ci4100.
Results : Our study population consisted of 153 subjects with covid-19. The mean age was 55±19 years (15 and 93 years). The most representative age group was patients over 60 years of age (52.3%). Male sex accounted for 53.8% of the study population. 45.1% of patients had a severe form with 16.3% of deaths during hospitalization. The association of renal biomarkers with disease severity showed that the risk of severe disease was higher in patients with hypoalbuminemia (OR=5.3 ; p=0.001), hyperuraemia (OR=4.1; p=0.001), hypercreatinine (OR=3.6; p=0.001), hyponatremia (OR=2.8; p=0.008) and hyperkalemia (OR=2.7; p=0.003).
Conclusion :Disruptions of renal biomarkers during SARS-Cov2 infection increase the risk of severity and mortality. Our study suggests that clinicians should pay close attention to kidney biomarkers in hospitalized patients with COVID-19.
Introduction
In December 2019, an outbreak of coronavirus disease (COVID-19) occurred in Wuhan, Hubei Province, China, in patients with unexplained lung disease [1]. Coronaviruses are a large family of viruses that can cause illnesses in humans ranging from the common cold to Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS).
It quickly spread to other parts of the world. The spread began later in Africa, than in Asia and Europe.
Advances in the field of pathophysiology have shown that the co-expression of angiotensin-converting enzyme 2 (ACE 2) receptors and serine transmembrane proteases 2 (TMPRSS) are required for the virus to enter the host cell [2].
Direct renal damage by the virus was therefore strongly suspected due to the high concentration of these receptors at the renal level, particularly at the level of the proximal tubule [3].
In the context of the high prevalence of kidney disease due to chronic conditions such as diabetes and hypertension [4], this study should be conducted on the evaluation of renal biomarkers during SARS-CoV-2 infection.
Materials and Method
This was a prospective, descriptive and analytical study of 153 patients infected with SARS-Cov2 who tested positive for RT-PCR.
We grouped patients into two groups, one group with a severe clinical presentation and another with a moderate clinical presentation.
- Moderate : flu-like type with or without fever
- severe : gastrointestinal type and fatigue, confusion type and respiratory involvement
And for each patient, blood samples were taken on a heparin tube or dry tube for the determination of parameters (albumin, creatinine, urea, Na+ K+) with the Abbott ARCHITECT ci4100.
The information was carried forward in the Excel 2016 software and the statistical analyses were carried out using the SPSS Version 25 software.
The statistical significance threshold was set for a p less than 0.05 value to study the association between the different parameters.
Results
The mean age of our study population was 55 ± 19 years and the extremes were 15 and 93 years. The most representative age group was that of patients over 60 years of age with a prevalence of 52.3%.
Male sex accounted for 53.8% of the study population with a sex ratio of 1.15.
Regarding clinical characteristics, at admission 45.1% of patients had a severe form of the disease. The mortality rate was 16.3% in our study population.
Table I : Clinical characteristics of patients with SARS-CoV-2 infection
| Features | Population | (%) | |
| Clinical forms | Moderate | 84 | 54,9 |
| Severe | 69 | 45,1 | |
| Total | 153 | 100,0 | |
| Evolution | Healings | 128 | 83,7 |
| Death | 25 | 16,3 | |
The study of the characteristics of the study population according to clinical presentation and age, shows a slight predominance of subjects over 60 years of age (52.2%) in patients with a severe form without showing a statistically significant difference.
Table II : Distribution of the population by age and clinical presentation
| Age | Moderate | Severe | P-value |
| < 60> | 40 (47,60%) | 33 (47,80%) |
P less then 0,001* |
| ≥ 60 | 44 (52,40%) | 36 (52,20%) |
Depending on the sex, severe forms were significantly higher (60.9%) in men than in women with a p=0.046.
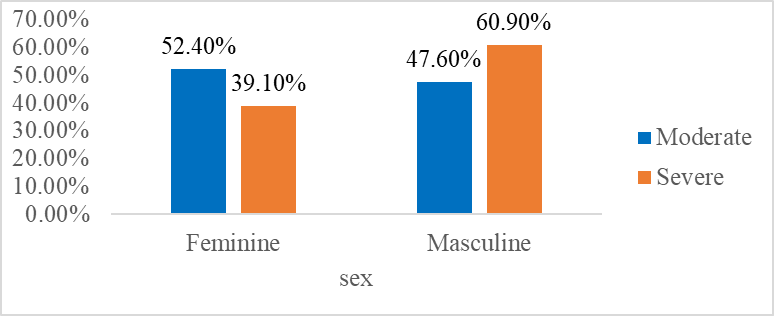
Fig 1: Distribution of the population by sex and clinical presentation
And according to the history, the results showed that patients who had kidney disease, 26.1% had a severe form.
Table III : Distribution of the population according to clinical presentation and history
| Features | Moderate | Severe | P-value |
| Diabetes | 7 (8,3%) | 11 (15,9%) |
P<0> |
| High blood pressure | 13 (15,5%) | 7 (8,3%) | |
| Kidney disease | 7 (8,3%) | 18 (26,1%) |
Disruption of renal biomarkers was observed only in patients who had developed a severe form with a statistically significant difference.
Table IV : Variation in Renal Biomarkers by Clinical Symptomatology
| Biomarkers | Severe | Moderate | |
| Average±SD | Average±SD | P-value | |
| Albumin | 28,9±8,5 | 36,3±6,3 | 0,001* |
| Urea | 0,85±0,81 | 0,4±0,37 | 0,001* |
| Créatinine | 44±5 | 19±3 | 0,001* |
| Na+ | 136,3±4,6 | 137,5±3,4 | 0,047* |
| K+ | 4,6±0,1 | 4,32±0,7 | 0,001* |
Severe disease was more pronounced in patients with hypoalbuminemia (OR=5.3 ; p=0.001), hyperuraemia (OR=4.1 ; p=0.001), hypercreatinine (OR=3.6 ; p=0.001), hyponatremia (OR=2.8 ; p=0.008) and hyperkalemia (OR=2.7 ; p=0.003).
Table V : Association between renal biomarkers and disease severity
| Renal biomarkers | Severe | Moderate | OR (IC (95)) | P-value | |
Hypoalbuminemia | Yes | 51 | 29 |
5,3 (2,6-10,8) |
0,001* |
| No | 18 | 55 | |||
Hyperuremia | Yes | 35 | 17 |
4,1 (2,2-8,2) |
0,001* |
| No | 34 | 67 | |||
Hypercreatininemia | Yes | 32 | 16 |
3,6 (1,7-7,5) |
0,001* |
| No | 37 | 68 | |||
Hyponatremia | Yes | 22 | 12 |
2,8(1,2-6,2) |
0,008* |
| No | 47 | 72 | |||
Hyperkaliemia | Oui | 35 | 23 |
2,7 (1,3-5,3) |
0,003* |
| Non | 34 | 61 |
Discussion
In December 2019, a new coronavirus was identified in the city of Wuhan, Hubei province in China, in patients with severe unexplained lung disease. [5]
The particularity of the virus is its rapid human-to-human transmission, this speed of spread of SARS-CoV-2 has led scientists all over the world to carry out a great deal of research to better understand and confront this formidable virus, described by the WHO as the "enemy of humanity"[6].
Covid-19 is associated with numerous biological disorders affecting many tissues and/or organs, due to their ubiquitous expression of the angiotensin-converting enzyme 2 (ACE2) receptor [7]. And among these organs, the kidney is one of them.
The results of our study showed, epidemiologically, an average age of 55±19 years with extremes of 15 and 93 years. The most representative age group was that of patients over 60 years of age with a proportion of 52.3%. Similar results were found in a study carried out in Wuhan in China by Placai et al with an average age of 55.5 years and an interval of 43 and 60 years. This can be explained by immunosenescence during age or the progressive deterioration of the immune system caused by the natural advancement of age [8], [9].
The sex ratio was 1.15, and similar results were noted In several studies in Wuhan, China by authors such as Guan et al (sex-ratio=1.4) [10]. This can be explained by the fact that female sex hormones ; estrogen and progesterone, but also allopregnanolone, which comes from the metabolism of progesterone, are thought to play an anti-inflammatory role. These hormones are thought to influence immune cells by stimulating the production of antibodies, and are thus potential inhibitors of the ACE2 receptor, the route of entry of the coronavirus into cells [11].
The case fatality rate of our study population was 16.3% which is similar to that of Cheng et al, a study conducted in China with a case fatality rate equal to 16.1% [12].
The study of the variation in epidemiological parameters according to the severity of the disease showed that severe forms were significantly more observed in men than in women (p=0.046). This result is close to the study by Michalakis et al in France and which suggests a hypothesis that this difference is due to a G6PDH deficiency [13]. This hypothesis is based on the fact that in vitro experiments have shown that the human coronavirus HCoV229E produces significantly more viral particles in human cells deficient in G6PD than in human cells that are not deficient [14].
The variation in renal biomarkers in patients with SARS-CoV-2 showed us that patients with hypoalbuminemia (28.9±8.5), hypercreatinine (44±5), hyperuremia (0.85±0.81), hyperkalemia (4.6±0.1) and hyponatremia (136.3±4.6) had more severe form. to a lesser extent, by the glomerulus [1].
This high expression of ACE2 would increase or promote the penetration of the virus into the cell and can consequently lead to destruction of the renal tubules and/or dysfunction of the glomeruli.
The association of renal biomarkers with disease severity showed that the risk of severe disease was higher in patients with hypoalbuminemia (OR=5.3; p=0.001), hyperuraemia (OR=4.1; p=0.001), hypercreatinine (OR=3.6; p=0.001), hyponatremia (OR=2.8; p=0.008), hyperkalemia (OR=2.7; p=0.003). These results are similar to those made by Cheng et al who found that patients with hypercreatinine were more likely to be admitted to the intensive care unit and undergo mechanical ventilation [15]. It can be caused by the virus-induced inflammatory response in the kidney or more general mechanisms such as hemodynamic instability, hypoxia and hypercoagulability, not to mention the different therapeutic means [16].
The association of renal biomarkers with disease mortality showed that the risk of death was more observed in patients who had hypoalbuminemia (OR=3.4 ; p=0.009), hyperuraemia (OR=4.1; p=0.001), hypercreatinine (OR=3.6; p=0.001), hyponatremia (OR=2.8; p=0.008) and hyperkalemia (OR=2.7; p=0.001). It was reported in a study by Chu et al that indicators of kidney damage on admission were associated with a higher risk of death in hospital[100]. This observation was correlated with a poor prognosis regardless of the initial severity of COVID-19 and general condition. Our results are also superimposed on those of Hatem Ali et al, who showed that severe acute kidney injury is associated with a high risk of mortality (OR=3.08) [17].
Conclusion
Our study found that monitoring of renal function should be prioritized even in patients with mild respiratory symptoms, and impaired renal function should be given special attention after admission.
Early detection and treatment of kidney abnormalities, including adequate hemodynamic support and avoidance of nephrotic medications, may help improve the life-threatening prognosis of patients with COVID-19.
References
- Bonny, V., Maillard, A., Mousseaux, C., Plaçais, L., & Richier, Q. (2020). COVID-19: Pathogenesis of a multi-faceted disease. La Revue de medecine interne, 41(6), 375-389.
- Hikmet, F., Méar, L., Edvinsson, Å., Micke, P., Uhlén, M., & Lindskog, C. (2020). The protein expression profile of ACE2 in human tissues. Molecular systems biology, 16(7), e9610.
- Wang, L., Li, X., Chen, H., Yan, S., Li, D., Li, Y., & Gong, Z. (2020). Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. American journal of nephrology, 51(5), 343-348.
- Faye, M., Ka, E. H. F., Lemrabott, A. T., Cisse, M. M., Fall, K., Omar, D. A. K., ... & Diouf, B. (2014). Prévalence de la maladie rénale dans une zone semi-urbaine du Sénégal: résultats d’une enquête transversale à la commune de Guéoul. Néphrologie & Thérapeutique, 10(5), 398.
- Zhu, N., Zhang, D., Wang, W., Li, X., Yang, B., Song, J., ... & Tan, W. (2020). A novel coronavirus from patients with pneumonia in China, 2019. New England journal of medicine, 382(8), 727-733.
- Amir, I. J., Lebar, Z., & Mahmoud, M. (2020). Covid-19: virologie, épidémiologie et diagnostic biologique. Option/Bio, 31(619-620), 15-20.
- Yeung, M. L., Teng, J. L. L., Jia, L., Zhang, C., Huang, C., Cai, J. P., ... & Yuen, K. Y. (2021). Soluble ACE2-mediated cell entry of SARS-CoV-2 via interaction with proteins related to the renin-angiotensin system. Cell, 184(8), 2212-2228.
- Franceschi, C., Valensin, S., Fagnoni, F., Barbi, C., & Bonafè, M. (1999). Biomarkers of immunosenescence within an evolutionary perspective: the challenge of heterogeneity and the role of antigenic load. Experimental gerontology, 34(8), 911-921.
- Ferrara, R., Mezquita, L., Auclin, E., Chaput, N., & Besse, B. (2017). Immunosenescence and immunecheckpoint inhibitors in non-small cell lung cancer patients: does age really matter?. Cancer treatment reviews, 60, 60-68.
- Guan, W. J., Ni, Z. Y., Hu, Y., Liang, W. H., Ou, C. Q., He, J. X., ... & Zhong, N. S. (2020). Clinical characteristics of coronavirus disease 2019 in China. New England journal of medicine, 382(18), 1708-1720.
- Ketfi, A., Chabati, O., Chemali, S., Mahjoub, M., Gharnaout, M., Touahri, R., ... & Saad, H. B. (2020). Profil clinique, biologique et radiologique des patients Algériens hospitalisés pour COVID-19: données préliminaires. The Pan African Medical Journal, 35(Suppl 2).
- Cheng, Y., Luo, R., Wang, K., Zhang, M., Wang, Z., Dong, L., ... & Xu, G. (2020). Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney international, 97(5), 829-838.
- Michalakis, Y., Sofonea, M. T., & Alizon, S. (2020). Les effets sexe spécifiques de COVID-19 en France pourraient-ils être expliqués par des comorbidités? (Doctoral dissertation, Centre National de la Recherche Scientifique (CNRS); Institut de recherche pour le développement (IRD); Université de Montpellier (UM), FRA.).
- Wu, Y. H., Tseng, C. P., Cheng, M. L., Ho, H. Y., Shih, S. R., & Chiu, D. T. Y. (2008). Glucose-6-phosphate dehydrogenase deficiency enhances human coronavirus 229E infection. The Journal of infectious diseases, 197(6), 812-816.
- Cheng, Y., Luo, R., Wang, K., Zhang, M., Wang, Z., Dong, L., ... & Xu, G. (2020). Kidney disease is associated with in-hospital death of patients with COVID-19. Kidney international, 97(5), 829-838.
- Legrand, M., Bell, S., Forni, L., Joannidis, M., Koyner, J. L., Liu, K., & Cantaluppi, V. (2021). Pathophysiology of COVID-19-associated acute kidney injury. Nature Reviews Nephrology, 17(11), 751-764.
- Ali, H., Daoud, A., Mohamed, M. M., Salim, S. A., Yessayan, L., Baharani, J., ... & Soliman, K. M. (2020). Survival rate in acute kidney injury superimposed COVID-19 patients: a systematic review and meta-analysis. Renal failure, 42(1), 393-397.


