Article In Press : Article / Volume 3, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5003/012
Exploring the Clinical Impact of Magnetite Nanoparticles in a Multifaceted Approach to Treating Multiple Sclerosis
- Laboratory of Applied Nanotechnology of Belousov.
- Kharkiv National Medical University, Ukraine.
- Krasnokutsk Central District Hospital, Ukraine.
A.N. Belousov
A.N. Belousov, E.Yu. Belousova, A.V. Mysik. (2024). Exploring the Clinical Impact of Magnetite Nanoparticles in a Multifaceted Approach to Treating Multiple Sclerosis. Archives of Immunology Research and Therapy, 3(1). DOI: 10.58489/2836-5003/012
© 2024 A.N. Belousov, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 21-04-2024
- Accepted Date: 09-07-2024
- Published Date: 12-07-2024
multiple sclerosis; treatment; nanodevice; Micromagе-B; neurological status assessment; remyelination.
Abstract
Multiple sclerosis (MS) is a serious neurological disorder due to its widespread prevalence, chronic nature, frequent progression to disability, and tendency to affect young people. The pathogenesis of MS is based on the immunopathogenesis hypothesis. Biocompatible magnetite nanoparticles, which exhibit selective sorption activity towards cell membrane surface proteins, circulating immune complexes, lymphocytotoxic antibodies, and the complement system, as well as enhance phagocytic activity and the completion index of leukocyte phagocytosis, can be effectively used for immunocorrection. The main goal of the study is to slow the progression of MS, improve the neurological status and overall condition of the patient, and reduce the dynamics of the spread of demyelinating lesions in the brain. Materials and methods: A patient diagnosed with multiple sclerosis, secondary progressive type, cerebrospinal form, at the clinical aggravation stage was included in the study. Neurological status and disability were assessed using the EDSS scale, and brain MRI with contrast enhancement was performed. The nanodevice Micromage-B was administered orally as an immunosorbent and immunomodulator. The regimen and dosage of Micromage-B were personalized. Assessments of general condition and neurological status were conducted every 7 days for 6 months, with contrast-enhanced brain MRI performed in the 5th month. Results: The use of Micromage-B in MS treatment led to an objective improvement in neurological status, with reduced stiffness and fatigue in the lower extremities. Gait and coordination improved, hand tremors decreased, depression and concentration disorders subsided, appetite was restored, and speech improved. Throughout the treatment period, positive dynamics in the normalization of neurological status were observed. After 6 months, the total score on the EDSS scale decreased from 210 to 45. The most significant improvements were observed in the evaluation of the pyramidal system and coordination, with the EDSS Disability Scale score decreasing from 6.0 to 5.0. For the first time, contrast-enhanced brain MRI showed a reduction in the number of new demyelination foci by the 4th month of Micromage-B administration. The positive changes in neurological status correlated with the MRI results. The recovery of central nervous system activity in MS is likely not only due to the immunosuppressive properties of magnetite nanoparticles but also due to the activation of remyelination mechanisms and oligodendrocyte differentiation through enzymatic methylation. Conclusion: The use of biocompatible nanodevices in the complex treatment of MS is promising. Further improvement and study of the regimen and method of using biocompatible magnetite nanoparticles to enhance MS treatment effectiveness are required.
Introduction
Multiple sclerosis (MS) is a significant neurological issue due to its widespread prevalence, chronic nature, frequent progression to disability, and tendency to affect young people, with an average onset age of 30 years. The primary hypothesis of MS immunopathogenesis suggests that immunological tolerance is disrupted, leading to the active penetration of autoreactive cells sensitized to nervous tissue antigens through the blood-brain barrier into brain tissue. B-lymphocytes recognize myelin and signal T cells to initiate an immune attack [1-7]. T- and B-cells secrete chemicals that attract other immune cells, causing inflammation [8,9]. Plasma cells produce antibodies that attack myelin and recruit other immune cells [10,11]. T- and B-cells establish a persistent presence in the central nervous system (CNS) and continue their attack [12,13].
There are two main hypotheses for MS pathogenesis: the outside-in hypothesis, which posits that immunocompetent cells activated in the periphery penetrate brain tissue, and the inside-out hypothesis, which suggests primary damage to nervous tissue leads to the expression of damage receptors from the DAMPs (Danger-associated Molecular Patterns) family, resulting in immune activation and loss of tolerance to myelin antigens [14]. Antibodies produced by plasma cells actively destroy the protective covering of nerve cells, causing inflammation. Over time, this tissue becomes scarred, disrupting conduction. Consequently, impulses from the brain fail to reach the limbs and organs, leading to a loss of body control [15]. Common initial clinical symptoms include weakness and impaired sensation in one or more limbs, decreased vision, urinary disturbances, and cerebellar ataxia.
Currently, immune modulatory and immune suppressive drugs that alter the course of MS form the cornerstone of pathogenetic treatment. Their mechanisms of action involve: 1) selective immune suppression, 2) complete immunosuppression, 3) prevention of the migration of activated cells from lymph nodes or into brain tissue, or 4) a combination of immunoregulatory, anti-inflammatory, antioxidant, and potentially neurotrophic actions. Future directions for new MS treatments include selective local immunocorrection, remyelination and neuroprotection, enhancement of neuroplasticity and functional relocalization, evaluation of the efficacy and safety of cell therapy, and individualized therapy selection based on predictions of pathological process variants and potential treatment responses derived from the molecular and cellular biology of MS [16-22].
The development of inflammation and demyelination in MS is driven by an impaired immune response, imbalance between regulatory and effector T cells, activation of B-cell immunity, and microglia. All drugs that impact the course of MS either deplete T- or B-cells or modify the signaling pathways involved in immune response formation [23].
Recently, significant attention has been given to the role of B-cells in chronic CNS inflammation, evidenced by their involvement in autoantibody formation, antigen presentation, and continuous T-cell activation in the brain parenchyma. Anti-B-cell therapies (Rituximab, Ocrelizumab, Ofatumumab) have shown effectiveness in both remitting and progressive MS. Stimulating remyelination in MS is associated with the development of new monoclonal antibody preparations, such as anti-LINGO and human immunoglobulin M (IgM), which promote remyelination and the differentiation of oligodendrocytes and their precursors [24].
One of the key mechanisms of axonal degeneration is mitochondrial dysfunction. Some drugs, such as Dimethylfumarate, Idebenone, and Biotin, show promise in addressing this issue [25]. Additionally, the use of drugs that affect the redistribution of ion channels in demyelinated axons (Lamotrigine, Amiloride, Fampridine) can help reduce the energy deficit in axons and neurons [26].
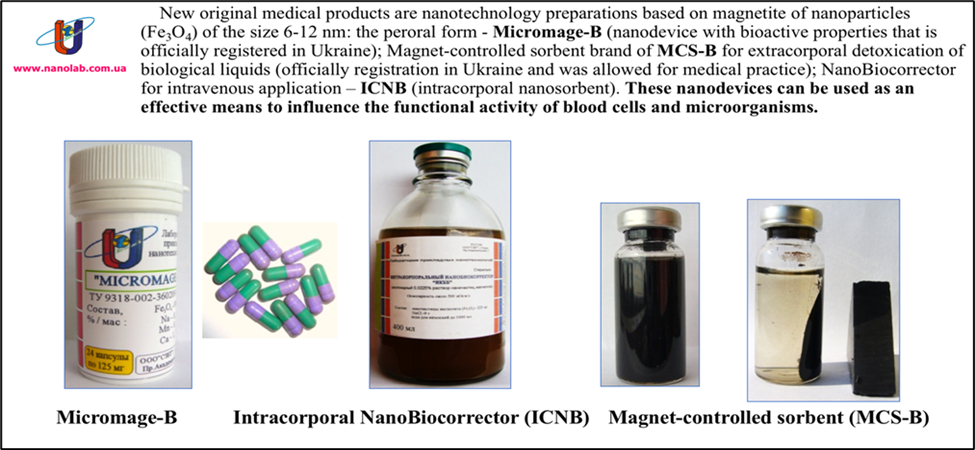
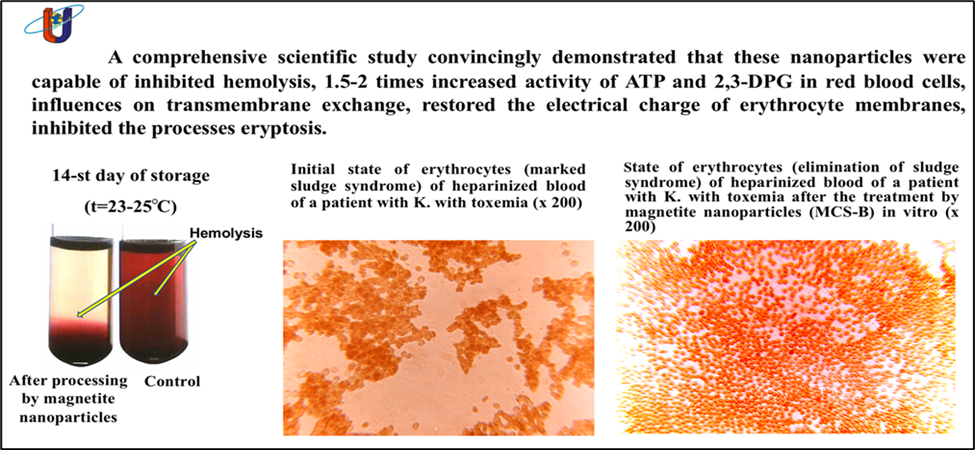
Recently, biocompatible nanotechnological preparations have seen increasing use in medicine. Since 1998, Ukrainian clinics have been officially using nanodevices developed by Belousov's Applied Nanotechnology Laboratory, including the Micromage-B, MCS-B, and ICNB brands (Figure 1) [27]. These nanodevices are based on biocompatible magnetite nanoparticles, whose unique physical and chemical characteristics enable a wide range of applications. They influence the quantitative and qualitative composition of bodily fluids, metabolic and biochemical processes, and the energy balance of cells. Their selective sorption activity against surface proteins of cell membranes, circulating immune complexes, lymphocytotoxic antibodies, and the complement system, as well as their ability to enhance phagocytic activity and leukocyte phagocytosis completion index [28], allow these nanodevices to be effectively used for immunocorrection. Moreover, these nanopreparations impact glycolysis processes, cell membrane ion channel activity, normalize erythrocyte function, improve microcirculation, and reduce the platelet aggregation index (Figure 2) [29-31]. They also activate the system of antiradical enzymes and inhibit lipid peroxidation processes [32,33].
The results of these studies lay the foundation for developing innovative techniques for the effective and safe use of biocompatible magnetite nanoparticles in treating severe autoimmune diseases, including multiple sclerosis. The primary objective of the study is to slow the progression of MS, improve the neurological status and overall condition of the patient, and reduce the spread of demyelinating foci in the brain.
Materials and Methods
Patient K. was diagnosed with multiple sclerosis, secondary progressive type, cerebrospinal form, at the clinical aggravation stage. The patient presented with pronounced spastic tetraparesis, more severe in the lower extremities, leading to walking impairment, pronounced urinary-ataxic syndrome, and sphincter and sensory disorders. MRI revealed signs of multifocal diffuse brain lesions (more than 30) of a demyelinating nature, indicating the active phase of the disease, and a diffuse atrophic process in the cerebral cortex. The average number of relapses in the year before study inclusion was 1.0, and the EDSS disability score was 6.0. The disease had progressed for 24 years since the onset of the first symptoms. For 14 years, the patient received regular treatment with vascular and metabolic drugs in combination with hormonal therapy. In the 6th year, despite active treatment, the disease progressed to a secondary progressive course, leading to the addition of the immunosuppressive drug Teriflunomide to the therapy regimen.
However, despite all treatment efforts, the patient's general condition progressively worsened, and the neurological status did not stabilize. MRI examinations over the last four years showed a continuous increase in the number of new demyelinating foci in the brain.
Given the above, the therapy regimen was supplemented with the prescription of Micromage-B [34]. Micromage-B is an oral nanodevice officially registered by the Ministry of Health of Ukraine. It is a powder form of magnetite (Fe3O4) nanoparticles designed for the prevention and treatment of various diseases and to enhance the body's resistance to adverse environmental factors. As a nanotechnology device, Micromage-B features magnetite nanoparticles sized between 6 and 12 nm. The therapeutic effect of Micromage-B is based on the mechanism of sorption and the action of a constant magnetic field on cellular and subcellular structures induced by the magnetite nanoparticles. The nanoparticles have a sorption surface area of 800 to 1200 m²/g and an induced magnetic field strength of 300-400 kA/m. The target of Micromage-B is the microenvironment of the cell's aqueous spaces and surface membrane proteins. Through selective sorption, the magnetite nanoparticles alter the quantitative and qualitative composition of cell surface proteins, and the constant magnetic field changes the mobility and orientation of hydrogen protons in the cell's aqueous microenvironment (Figure 3).
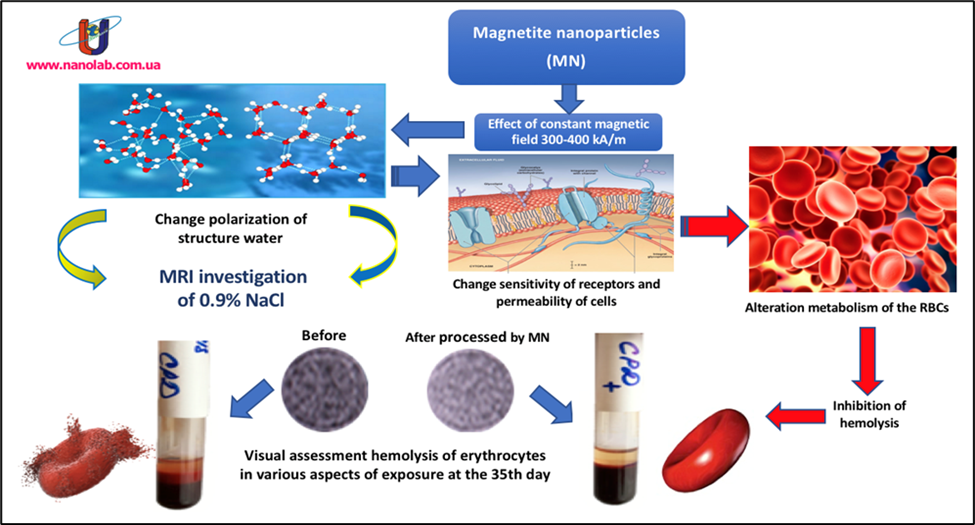
This leads to the activation of hydrolysis of the phosphate residue ATP, ultimately modifying the cell's transmembrane exchange and metabolism, and altering its susceptibility. The nanodevice enhances adaptive mechanisms and the potential of cell organelles, accelerates reparative processes at the membrane and macromolecule levels, significantly increases the level of synthetic intracellular reactions, and boosts the compensatory capabilities of organelles within renal glomerulus cells and the epithelial cells of the proximal and distal nephron sections. This structural enhancement is expressed through improved bioenergetic support for synthetic intracellular processes, and increased reparative and adaptive capabilities of nephrons. By enhancing redox phosphorylation processes, which meet the energy demands of synthetic intracellular reactions occurring at the membrane and macromolecular levels in hepatic cells, Micromage-B functions as a direct activator of reparative intracellular processes in hepatocytes and augments glycogen synthesis. This characteristic renders it effective as a potent hepatoprotective agent in treating both acute and chronic liver ailments. Micromage-B also serves as a potent erythropoiesis stimulator, rapidly restoring blood hemoglobin levels. Moreover, it stimulates pulmonary surfactant synthesis, enhancing lung tissue stretchability and elasticity, thereby fortifying lung stability against internal and external environmental stressors by increasing alveolar macrophage activity. Clinically and in laboratory settings, Micromage-B enhances microcirculation and blood rheological properties by stabilizing erythrocyte membrane bioelectric charge, exhibiting a significant immunomodulatory effect, and selectively exerting bacteriostatic effects against pathogenic microflora while preserving normoflora. It impedes the growth and proliferation of various fungi and promotes the growth and activity of lactic acid bacteria in the intestines, thereby enhancing the efficacy of antibacterial and antifungal agents by 2-3 times. These attributes enable Micromage-B's effective application in dysbacteriosis and candidiasis treatment. Additionally, Micromage-B nanoparticles adsorb toxic substances and circulating immune complexes, significantly enhancing the treatment efficacy of various allergic diseases, autoimmune processes (such as rheumatoid arthritis, acute and chronic polyarthritis, eczema, etc.), and acute poisoning. Micromage-B moderately improves renal blood flow, exerting a mild diuretic effect.
With its inherent magnetic moment, magnetite nanoparticles within Micromage-B facilitate the breakdown and dissolution of kidney and bile duct stones, subsequently eliminating them from the body as magnetically sensitive crystalline forms through the excretory system. Micromage-B actively contributes to normalizing lipid and protein levels in the blood. Micromage-B influences atherogenesis factors, impeding the progression of atherosclerotic processes. The continuous magnetic field of magnetite nanoparticles within Micromage-B diminishes the release of excessive aggressive mediators into the bloodstream within macrophage cells. Consequently, this elicits notable anti-inflammatory and mild analgesic effects. Micromage-B regulates the activity of antioxidant enzymes, absorbs lipid peroxidation products, and rebalances antiradical and pro-radical product levels. Under Micromage-B influence, monocytes actively produce tumor necrosis factor (cachexin), exerting cytotoxic and cytostatic effects on tumor cells. Topically applied (as powders, ointments, or aqueous colloidal solutions), Micromage-B accelerates mucous membrane and skin wound healing, transitioning wet tissue necrosis to dry. Micromage-B demonstrates non-toxicity and does not disrupt organ or systemic functional activity [35,36].
The dosing regimen for Micromage-B entails 500 mg daily for the first month, 500 mg every other day for the second month, and subsequently, 500 mg once every three days. The selection of Micromage-B dosage and regimen is tailored individually, considering the patient's rate of improvement and neurological recovery.
The study monitored changes in neurological status using a modified version of the Multiple Sclerosis Patient Assessment Scale [37,38], which evaluates the severity of motor impairments alongside other nervous system damage indicators. Disability was quantitatively assessed using Kurtzke's online EDSS calculator [39]. Manifestations of cerebral demyelination foci were examined through contrast-enhanced MRI.
The patient's overall condition and neurological status were assessed every 7 days over a 6-month period. As per the protocol, a contrast-enhanced MRI of the brain was conducted annually, aligning with the 5th month of Micromage-B usage.
Results
The progression of neurological changes was assessed using a modified scale. One week following the administration of Micromage-B, a marked enhancement in the patient's neurological condition was evident. The patient reported a notable reduction in lower limb stiffness and rapid fatigue. Objectively, improvements were observed in gait and coordination, reduction in hand tremors, complete alleviation of depression and concentration issues, restoration of appetite, and enhancement in speech. Positive trends in normalizing neurological status persisted throughout the entire duration of Micromage-B treatment. Table 1 illustrates the evaluation of a multiple sclerosis patient's neurological status before and after 6 months of Micromage-B administration.
Table 1: Assessment of Neurological Status Scale for Patient K. with Multiple Sclerosis.
. | ||||||
| Input data | Six months after application Micromage-B | Clinical manifestations | ||||
| Arm | Leg | Arm | Leg | |||
| 0 | 0 | 0 | 0 | Norma | ||
| 5 | 10 | 5* | 10* | Absence of loss symptoms, revival of tendon reflexes, enlargement of reflexogenic zones, clonus, presence of pathological signs, anisoreflexia, (absence of paresis) | ||
| 10 | 20 | 10 | 20 | Raises a limb independently, full volume of active movements, signs of pyramidal lesion, overcomes not only the gravity of his own limb, but also an additional obstacle of moderate strength, positive Barre-Rusetsky's symptom | ||
| 15 | 40 | 15 | 40 | Raises a limb independently, the volume of active movements is full, cannot hold a limb in a given position for a long time, and cannot overcome an additional obstacle. | ||
| 20* | 60* | 20 | 60 | Can pull a limb off the plane, the amount of active movement is limited, cannot hold a limb in a given position. | ||
| 40 | 80 | 40 | 80 | Cannot detach a limb from the plane, active movements in the joints of the fingers, ankle and wrist, elbow, knee joints are possible only on the plane. | ||
| 50 | 100 | 50 | 100 | Complete absence of movement (paralysis) | ||
2. Sensitivity | ||||||
| Before | After | (a) superficial sensitivity | ||||
| 0 | 0* | Norma | ||||
| 5 | 0 | Paresthesias, burning sensation, numbness, coldness of a limb (no objective disorders) | ||||
| 10* | 10 | Hyperesthesia or hypoesthesia | ||||
| 15 | 15 | Anesthesia phenomena | ||||
| b) deep sensitivity | ||||||
| 0* | 0* | Norma | ||||
| 10 | 10 | Disorder of joint and muscle feeling in small joints | ||||
| 20 | 20 | Disorder of joint and muscle feeling up to the level of the middle joints (wrist, ankle) | ||||
| 40 | 40 | Disorder of joint and muscle feeling up to the level of large joints (elbow, shoulder, knee, hip) | ||||
3. Coordination | ||||||
| 0 | 0 | Norma | ||||
| 10 | 10* | Unsteadiness, swaying in the sensitized Romberg's test while standing on one leg, mild intensional trembling (in the complicated test), slight ataxia in the heel-knee test, deviation when walking with eyes closed. | ||||
| 40* | 10 | Unsteadiness in simple Romberg's pose, atactic gait with open eyes and legs spread wide apart, "drunkenness," moderately pronounced intensional tremor and ataxia in the heel-knee test. | ||||
| 100 | 100 | Because of ataxia, the patient cannot move without assistance, sharp hypotonia of muscles, intensional shaking of the head, trunk, coarse - upper extremities, coarse ataxia during heel-knee test, trembling of upper extremities when trying to perform purposeful movement, chanted speech. | ||||
4. Psycho-emotional sphere | ||||||
| 0 | 0* | Norma | ||||
| 10 | 10 | Mild impairment of the intellect in combination with euphoria, rapid change of mood, neurasthenic syndrome. | ||||
| 20* | 0 | Euphoria, depression, decreased criticism of one's condition, decreased memory. | ||||
| 100 | 100 | Severe mental disorder, complete intellectual disintegration, Korsak's syndrome, etc. | ||||
5. Nystagmus | ||||||
| 0 | 0* | Norma | ||||
| 5 | 5 | Nystagmus is detected only in the extreme leads (degree 1) | ||||
| 10* | 10 | Nystagmus when looking straight ahead (degree 2) | ||||
| 15 | 15 | Sharp beating nystagmus, nystagmus in both directions, even toward the slow component (3rd degree) | ||||
6. State of the sphincters | ||||||
| 0 | 0* | Norma | ||||
| 10* | 10 | Impulsive urges, inability to hold urine for a long time, difficulty urinating | ||||
| 20 | 20 | Urinary incontinence, urinary retention, intermittent urination disorders, persistent constipation | ||||
7. Sexual function | ||||||
| 0 | 0* | Norma | ||||
| 5* | 5 | Decreased sexual activity in men (intermittent impotence), sexual coldness in women | ||||
| 10 | 10 | Total impotence, menstrual disorders in women | ||||
8. The ocular fundus | ||||||
| 0 | 0 | Norma | ||||
| 5 | 5 | Disturbance of vascular pattern, narrowing of arteries, dilation of veins, changes on fluorescence ophthalmoscopy | ||||
| 10* | 10* | Partial optic atrophy (bitemporal pallor), optic neuritis | ||||
| 15 | 15 | Complete atrophy of the optic nerve | ||||
9. Visual acuity | ||||||
| 0 | 0 | Norma (vision within 1.0 or myopia) | ||||
| 5 | 5 | Occasional blurring of vision, rapid fatigue when reading and performing work without impaired visual acuity | ||||
| 10* | 10* | Visual acuity from 0.9 to 0.7 | ||||
| 15 | 15 | Visual acuity from 0.6 to 0.4 | ||||
| 20 | 20 | Visual acuity from 0.3 to 0.1 | ||||
| 25 | 25 | Visual acuity 0.1 and below | ||||
| 100 | 100 | Blindness in one or both eyes | ||||
10. Oculomotor nerves | ||||||
| 0 | 0* | Norma (absence of subjective and objective symptoms) | ||||
| 5* | 0 | Concealed insufficiency, without visible dysfunction of one of the oculomotor nerves, inter-nuclear ophthalmoplegia syndrome | ||||
| 10 | 10 | Mild visible impairment, visible insufficiency of one or more nerves, diplopia, ptosis, anisocoria | ||||
| 15 | 15 | Convergent or divergent strabismus | ||||
| 20 | 20 | Complete ophthalmoplegia (in one or both eyes) | ||||
11. The trigeminal nerve | ||||||
| 0* | 0* | Norma (absence of subjective and objective symptoms) | ||||
| 5 | 5 | Subjective sensations in the form of pain, numbness, sense of "creeping chills", oppression in the face. | ||||
| 10 | 10 | Objective signs of lesions, hypoesthesia, loss or decrease in the corneal reflex. | ||||
| 20 | 20 | Severe anomalies with loss of trigeminal nervous functions, with or without neuralgic disorders. | ||||
12. The facial nerve | ||||||
| 0 | 0* | Norma | ||||
| 5* | 0 | Moderate weakness of facial muscles (eye closes completely, but cannot actively close it), asymmetry of frontal and nasolabial folds | ||||
| 10 | 10 | Moderate weakness of mimic muscles (lagophthalmus, positive Bell's symptom, facial asymmetry in grinning), with preservation, to some extent, of mimic movements | ||||
| 20 | 20 | Complete paralysis of facial muscles | ||||
13. Bulbar group of cranial nerves (nerves 9,10,11,12) | ||||||
| 0 | 0* | Norma | ||||
| 5* | 5 | Mildly pronounced bulbar phenomena (gagging when taking liquid food, change in speech, without gross organic symptoms of prolapse) | ||||
| 10 | 10 | Severe dysphagia, dysarthria, decreased soft palate and posterior pharyngeal wall reflexes | ||||
| 100 | 100 | Complete bulbar paralysis | ||||
14. Auditory nerve | ||||||
| 0* | 0* | Norma | ||||
| 5 | 5 | Conversational speech at a distance of 4 to 6 m, whispered speech at a distance of 1 to 3 m. | ||||
| 10 | 10 | Speech - from 2 to 4 m, whisper - from 0.5 to 1 m. | ||||
| 15 | 15 | Spoken speech 2 m or less, whispered speech 0 to 0.5 m | ||||
| 20 | 20 | Complete deafness in one or both ears | ||||
| Total: | Total: | |||||
| 210* | 45* | |||||
Note: * - estimated scores of the neurological status before and after using the Micromage-B.
The data presented in Table 1 illustrate a positive trend in normalizing neurological status following 6 months of Micromage-B usage. Initially, the total points amounted to 210, which decreased to 45 after the 6-month period, indicating a reduction of 165 points. The most significant improvement was observed in the assessment of the pyramidal system and coordination. Additionally, the EDSS disability scale score decreased from 6.0 to 5.0.
A contrast-enhanced MRI of the brain conducted after 4 months of Micromage-B usage revealed a decrease in the number of new demyelination foci in the brain for the first time. The favorable progression of neurological status correlated with the brain MRI findings.
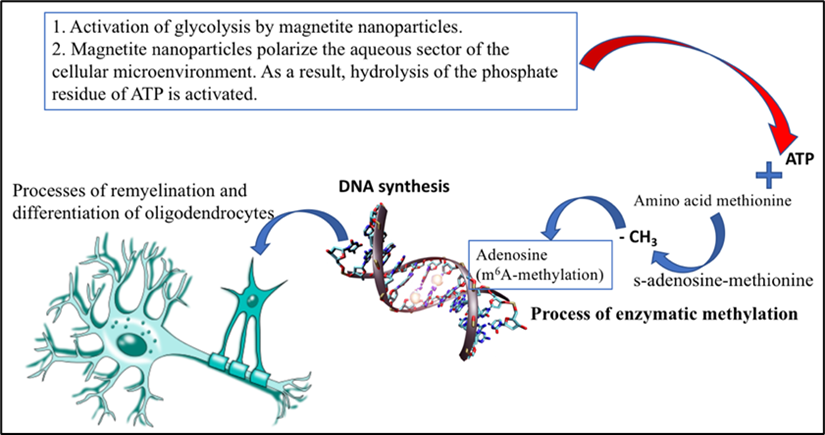
Upon analyzing the collected data, particular attention should be given to the observed positive clinical effects attributed to immunosorption and the active contribution of Micromage-B's magnetite nanoparticles to neurological status restoration. This effect may be attributed to remyelination processes and oligodendrocyte differentiation. Oligodendrocytes, a type of neuroglial cell, form the myelin sheath around neurons in the central nervous system (CNS). The molecular mechanisms underlying cell differentiation and specialization remain complex and poorly understood, presenting a challenging area in cell and developmental biology. The development and maturation of various cell types continue to pose significant research challenges.
However, it is now understood that one mechanism underlying oligodendrocyte maturation involves enzymatic methylation, specifically the addition of a methyl group (-CH3) to the N6 nitrogen atom in adenosine's nitrogenous base, referred to as m6A-methylation. Despite its seemingly minor nature, this modification can significantly impact subsequent stages of protein biosynthesis. The role of m6A-methylation has been demonstrated in numerous processes associated with oligodendrocyte maturation [40]. The body's universal methyl group donor is S-adenosylmethionine, generated through the interaction between the amino acid methionine and ATP.
Given that Micromag-B activates glycolysis, it significantly increases the production of the macroergic compound ATP [41,42], and promotes the formation of the reduced form of the coenzyme NADPH2, facilitating the conversion of oxidized glutathione to its reduced form [43]. These conditions are conducive to initiating enzymatic methylation processes, which likely enhance the mechanism of action of magnetite nanoparticles (Micromag-B). This, in turn, supports the differentiation of oligodendrocytes and the remyelination process. Additionally, it should be noted that these nanoparticles polarize the aqueous environment of the cellular microenvironment [44], leading to the activation of ATP hydrolysis, energy release, and the formation of ADP. For a detailed understanding of how biocompatible magnetite nanoparticles (Micromag-B) influence remyelination processes, refer to Figure 4.
Given the positive neurological status dynamics, it was deemed appropriate to continue Micromage-B nanopreparation administration at the prescribed dosage. Therapy was augmented with a regimen of rehabilitative exercises aimed at expediting the restoration of physical, cognitive, and psychosocial functions in patients with MS.
Considering the positive progression in neurological status, it was decided to continue the administration of the nanopreparation Micromage-B at the prescribed dosage. Additionally, the therapy was augmented with a comprehensive rehabilitation exercise program designed to expedite the recovery of physical, cognitive, and psychosocial functions in a patient with MS.
Conclusion
The study's results broadened the clinical effectiveness of biocompatible magnetic nanoparticles in treating severe autoimmune diseases [45-48]. The use of the Micromage-B nanopreparation in treating multiple sclerosis (MS) demonstrated a significant positive clinical effect. Positive trends in normalizing the neurological state were observed throughout the application period of Micromage-B. After six months of treatment, the overall score decreased from 210 to 45. The most notable improvement was seen in the assessment of the pyramidal system and coordination. The EDSS Disability Scale score decreased from 6.0 to 5.0. For the first time, contrast-enhanced MRI of the brain recorded a reduction in the number of new demyelination foci by the fourth month of Micromage-B administration. The normalized neurological condition correlated with positive brain MRI results. The restoration of central nervous system activity in MS is attributed not only to the immunosuppressive properties of magnetite nanoparticles but also likely to the activation of remyelination mechanisms and oligodendrocyte differentiation through enzymatic methylation. The design and method of using biocompatible magnetite nanoparticles to enhance MS treatment efficiency require further refinement and research. The use of biocompatible nanodevices in the comprehensive treatment of MS is a promising innovation, and the near future aims to incorporate magnetite nanoparticles into the protocols for complex MS treatment [49-51].
References
- Duffy, S. S., Lees, J. G., & Moalem-Taylor, G. (2014). The contribution of immune and glial cell types in experimental autoimmune encephalomyelitis and multiple sclerosis. Multiple sclerosis international, 2014.
- Ortiz, G. G., Pacheco-Moisés, F. P., Macías-Islas, M. Á., Flores-Alvarado, L. J., Mireles-Ramírez, M. A., González-Renovato, E. D., ... & Alatorre-Jiménez, M. A. (2014). Role of the blood–brain barrier in multiple sclerosis. Archives of medical research, 45(8), 687-697.
- Larochelle, C., Alvarez, J. I., & Prat, A. (2011). How do immune cells overcome the blood–brain barrier in multiple sclerosis? FEBS letters, 585 (23), 3770-3780.
- Cross, A. H., & Waubant, E. (2011). MS and the B cell controversy. Biochimica et Biophysica Acta (BBA)-Molecular Basis of Disease, 1812(2), 231-238.
- Dalakas, M. C. (2008). B cells as therapeutic targets in autoimmune neurological disorders. Nature clinical practice Neurology, 4 (10), 557-567.
- Constant, S. L. (1999). B lymphocytes as antigen-presenting cells for CD4+ T cell priming in vivo. The Journal of Immunology, 162(10), 5695-5703.
- Crawford, A., MacLeod, M., Schumacher, T., Corlett, L., & Gray, D. (2006). Primary T cell expansion and differentiation in vivo requires antigen presentation by B cells. The Journal of Immunology, 176(6), 3498-3506.
- Bar‐Or, A., Fawaz, L., Fan, B., Darlington, P. J., Rieger, A., Ghorayeb, C., ... & Smith, C. H. (2010). Abnormal B‐cell cytokine responses a trigger of T‐cell–mediated disease in MS?. Annals of neurology, 67(4), 452-461.
- Duddy, M., Niino, M., Adatia, F., Hebert, S., Freedman, M., Atkins, H., ... & Bar-Or, A. (2007). Distinct effector cytokine profiles of memory and naive human B cell subsets and implication in multiple sclerosis. The Journal of Immunology, 178(10), 6092-6099.
- Genain, CP., et al. (1999). Identification of autoantibodies associated with myelin damage in multiple sclerosis. Nat Med, 5(2):170-175.
- Storch, M. K., Piddlesden, S., Haltia, M., Iivanainen, M., Morgan, P., & Lassmann, H. (1998). Multiple sclerosis: in situ evidence for antibody‐and complement‐mediated demyelination. Annals of neurology, 43(4), 465-471.
- Serafini, B., Rosicarelli, B., Magliozzi, R., Stigliano, E., & Aloisi, F. (2004). Detection of ectopic B‐cell follicles with germinal centers in the meninges of patients with secondary progressive multiple sclerosis. Brain pathology, 14(2), 164-174.
- Magliozzi, R., Howell, O. W., Reeves, C., Roncaroli, F., Nicholas, R., Serafini, B., ... & Reynolds, R. (2010). A gradient of neuronal loss and meningeal inflammation in multiple sclerosis. Annals of neurology, 68(4), 477-493.
- Dhaiban, S., Al-Ani, M., Elemam, N. M., Al-Aawad, M. H., Al-Rawi, Z., & Maghazachi, A. A. (2021). Role of peripheral immune cells in multiple sclerosis and experimental autoimmune encephalomyelitis. Sci, 3(1), 12.
- Kobelt, G., Thompson, A., Berg, J., Gannedahl, M., Eriksson, J., MSCOI Study Group, & European Multiple Sclerosis Platform. (2017). New insights into the burden and costs of multiple sclerosis in Europe. Multiple Sclerosis Journal, 23 (8), 1123-1136.
- Farooqi, N., Gran, B., & Constantinescu, C. S. (2010). Are current disease‐modifying therapeutics in multiple sclerosis justified on the basis of studies in experimental autoimmune encephalomyelitis?. Journal of neurochemistry, 115(4), 829-844.
- Polman, C. H., O'Connor, P. W., Havrdova, E., Hutchinson, M., Kappos, L., Miller, D. H., ... & Sandrock, A. W. (2006). A randomized, placebo-controlled trial of natalizumab for relapsing multiple sclerosis. New England Journal of Medicine, 354(9), 899-910.
- Yednock, T. A., Cannon, C., Fritz, L. C., Sanchez-Madrid, F., Steinman, L., & Karin, N. (1992). Prevention of experimental autoimmune encephalomyelitis by antibodies against α 4 β l integrin. Nature, 356(6364), 63-66.
- Ridge, S. C., Sloboda, A. E., McReynolds, R. A., Levine, S., Oronsky, A. L., & Kerwar, S. S. (1985). Suppression of experimental allergic encephalomyelitis by mitoxantrone. Clinical immunology and immunopathology, 35(1), 35-42.
- Huang, W. J., Chen, W. W., & Zhang, X. (2017). Multiple sclerosis: Pathology, diagnosis and treatments. Experimental and therapeutic medicine, 13(6), 3163-3166.
- Ghasemi, N., Razavi, S., & Nikzad, E. (2017). Multiple sclerosis: pathogenesis, symptoms, diagnoses and cell-based therapy. Cell Journal (Yakhteh), 19(1), 1.
- Hanafy, K. A., & Sloane, J. A. (2011). Regulation of remyelination in multiple sclerosis. FEBS letters, 585(23), 3821-3828.
- Ghasemi, N., Razavi, S., & Nikzad, E. (2017). Multiple sclerosis: pathogenesis, symptoms, diagnoses and cell-based therapy. Cell Journal (Yakhteh), 19(1), 1.
- Høglund, R. A., & Maghazachi, A. A. (2014). Multiple sclerosis and the role of immune cells. World journal of experimental medicine, 4 (3), 27.
- Barcelos, I. P. D., Troxell, R. M., & Graves, J. S. (2019). Mitochondrial dysfunction and multiple sclerosis. Biology, 8(2), 37.
- Hamada, M. S., & Kole, M. H. (2015). Myelin loss and axonal ion channel adaptations associated with gray matter neuronal hyperexcitability. Journal of Neuroscience, 35 (18), 7272-7286.
- www.nanolab.com.ua
- Belousov, А. N. (2011, September). The use of magnetite nanoparticles in applied medicine. In Materials Science Forum (Vol. 694, pp. 205-208). Trans Tech Publications Ltd.
- Belousov, A. N. (2014). The role of magnetite nanoparticles (ICNB) in discovery new factor which influence on permeability of erythrocytes and eryptosis. Journal Nanoscience and Nanotechnology Research, 2(1), 8-11.
- Belousov, A. N., Malygon, E., Yavorskiy, V., Belousova, E. (2018). Application of the stanardized form magnetite nanoparticles (ICNB) in creature simple and practical method of additive modernization of preservation solutions for red blood cells. Global Journal of Anesthesia and Pain Medicine, 1(1).
- Belousov, A. (2020). Study of the Effect of Nanotechnology Drugs (mcs-b) on the Aggregation of Human Blood Platelets. Journal of Nanosciences Research & Reports. Scientize Publishers, 1(1), 1-8.
- Belousov, A., Malygon, E., Yavorskiy, V., Belousova, E. (2019). Innovative method of nanotechnology to increase the storage time of RBCs due by stabilizing the molecular structure of proteins and lipids of erythrocyte membranes. Biomedical Journal of Scientific & Technical Research, 13(4), 10079-10087.
- Belousov, A., Kalynychenko, T., Malygon, E., Anoshyna, M., Yagovdik, M., Yavorskiy, V., Belousova E. (2022). Research of Lipid Peroxidation after Administration of Nanomodified Resuspending Solution in Donor Red Blood Cells on During Their Storage. International Journal of Biomed Research. 2(2).
- Patent Agency of Ukraine No. 30538А UA A 23L 1/304 Therapeutic and preventive product MICROMAGE-B / A.N. Belousov № 98052704. 25.05.98. Publ. 15.11.00. Bul. No. 6-11.
- http://nanolab.com.ua/products/micromagindex.html
- Belousov, A. (2018). A New Promising Method of Hepatitis Treatment at the Level of Ultrastructure of the Liver by Standardized Powder form of Magnetite Nanoparticles (Micromage-B). Journal of Pharmacology & Clinical Research 6(1).
- Gordeev Y.Y, Shamova T.M., Semashko V.V. Scale of evaluation of the neurological status in multiple sclerosis. (2006). Journal of GrSMU, 1, 75-78.
- Kurtzke, J. F. (1983). Rating neurologic impairment in multiple sclerosis: an expanded disability status scale (EDSS). Neurology, 33 (11), 1444-1444.
- https://edss.neurol.ru/
- Xu, H., Dzhashiashvili, Y., Shah, A., Kunjamma, R. B., Weng, Y. L., Elbaz, B., ... & Popko, B. (2020). m6A mRNA methylation is essential for oligodendrocyte maturation and CNS myelination. Neuron, 105 (2), 293-309.
- Belousov, A. (2012) Effect on Hemolysis and Transport ATPase Activity of Erythrocytes by Means Nanopareticles of Magnetit Controlled Sorbent (MCS-B). Pain, Anesthesia and Intensive Care, 1, 26-28.
- Belousov, A. N. (2014). The role of magnetite nanoparticles (ICNB) in discovery new factor which influence on permeability of erythrocytes and eryptosis. Journal Nanoscience and Nanotechnology Research, 2(1), 8-11.
- Belousov, A., Kalynychenko, T., Malygon, E., Anoshyna, M., Yagovdik, M., Yavorskiy, V., & Belousova, E. (2021). Study of effects a new resuspending solution which was nanotechnologically upgraded on lipoperoxidation, catalase activity and red blood cell peroxidation resistance in donor blood components. Archives in Biomedical Engineering and Biotechnology, 6(2), 1-6.
- Belousov, A. N. (2013). Myth and reality application of magnetite nanoparticles as selective contrasting means of the malignant tumors in MRI investigation. Biomedical Engineering Research, 2(3), 147-152.
- Singh, A. V., Khare, M., Gade, W. N., & Zamboni, P. (2012). Theranostic implications of nanotechnology in multiple sclerosis: a future perspective. Autoimmune diseases, 2012 (1), 160830.
- Silva, G. A. (2006). Neuroscience nanotechnology: progress, opportunities and challenges. Nature reviews neuroscience, 7 (1), 65-74.
- Kanwar, J. R., Sun, X., Punj, V., Sriramoju, B., Mohan, R. R., Zhou, S. F., ... & Kanwar, R. K. (2012). Nanoparticles in the treatment and diagnosis of neurological disorders: untamed dragon with fire power to heal. Nanomedicine: Nanotechnology, Biology and Medicine, 8(4), 399-414.
- Srikanth, M., & Kessler, J. A. (2012). Nanotechnology—novel therapeutics for CNS disorders. Nature reviews neurology, 8(6), 307-318.
- Fazil, M., Shadab, Baboota, S., Sahni, J. K., & Ali, J. (2012). Nanotherapeutics for Alzheimer’s disease (AD): past, present and future. Journal of drug targeting, 20(2), 97-113.
- Wankhede, M., Bouras, A., Kaluzova, M., & Hadjipanayis, C. G. (2012). Magnetic nanoparticles: an emerging technology for malignant brain tumor imaging and therapy. Expert review of clinical pharmacology, 5(2), 173-186.
- Patel, T., Zhou, J., Piepmeier, J. M., & Saltzman, W. M. (2012). Polymeric nanoparticles for drug delivery to the central nervous system. Advanced drug delivery reviews, 64(7), 701-705.


