Research Article | DOI: https://doi.org/10.58489/2836-5062/008
Gamma knife radiosurgery outcomes for identified bilateral cavernous sinus meningiomas: A retrospective case series report
- Raef F.A. Hafez* 1
- Magad S. Morgan 2
- Esam Abed El Kawy 3
- Osama M. Fahmy 4
- Wael K. Zakaria 5
- Hamdy T. Hassan 6
- Prof. of Neurosurgery and Gamma knife Radiosurgery-International Medical Center-IMC, Cairo- Egypt.
- FRCS. Consultant Neurosurgery. International medical center-IMC, Cairo- Egypt.
- M.D. Consultant Neurosurgery. El Galla Military Hospital. An associate consultant -IMC, Cairo- Egypt.
- M.D. Prof of Neurosurgery. International medical center (IMC), Cairo- Egypt.
- M.D. Assistant Prof. of Neurosurgery Mansoura University Hospital. An associate consultant -IMC, Cairo- Egypt.
- M.D. Consultant Neurosurgery –International Medical Center-IMC, Cairo- Egypt
*Corresponding Author: Raef F.A. Hafez
Citation: Raef F.A. Hafez, Magad S. Morgan, Esam Abed El Kawy, Osama M. Fahmy, Wael K. Zakaria, and Hamdy T. Hassan, (2023). Gamma knife radiosurgery outcomes for identified bilateral cavernous sinus meningiomas: A retrospective case series report. Journal of Clinical Oncology Reports. 2(2). DOI: 10.58489/2836-5062/008
Copyright: © 2023 Raef F.A. Hafez, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 05 January 2023 | Accepted: 12 January 2023 | Published: 25 January 2023
Keywords: GKRS; Gamma Knife Radiosurgery, CSM; Cavernous Sinus meningioma, CNs; Cranial nerves, MIM; Multiple Intracranial Meningioma
Abstract
Objective: This retrospective case series aims to report five radiological identified patients with symptomatic bilateral CSMs treated with GKRS and analyze the outcomes. Results: All reported patients were females; the median age at presentation was 45 years and the median follow-up period was 74 months (range 40–132 months). Four patients (83.3%) achieved clinical control, including improvement in CNs function in 3 patients, and one remained stable. Tumor control was achieved in 4 patients (80%), two achieved tumor size reduction, and two remained. Following GKRS, the estimated survival free of radiographic tumor progression rates at 3, 5, and 7 years were 100%, 80%, and 75%, respectively. Conclusion: GKRS offered safe and effective long-term tumor and clinical control for small to medium-sized symptomatic benign bilateral CSM as much as it usually does with solitary cavernous sinus meningioma.
Introduction
Meningiomas are common brain tumors, accounting for approximately one-third of all adult primary brain tumors. Most intracranial meningiomas are single, and ≥90 % are pathologically benign. [9, 23, 26]
Solitary Cavernous sinus meningiomas (CSMs) are the most common primary cavernous sinus tumors, occurring in about 0.5 per 100′000 persons in the general population and over 90% are benign. [4, 5, 9]
After aggressive surgery for CSMs, mortality rates have ranged from 0% to 7%, and morbidity rates are between 10% and 65%. During the last two decades, numerous GKRS series related to CSM have reported tumor control rates that range from 88% to 100% [7,15,16, 21 ] and a low rate of treatment-related complications.[17,20,25 ]
Bilateral cavernous sinus meningioma has not been reported in the literature in multiple intracranial meningiomas. The current study aims to present a case series of bilateral cavernous sinus meningioma patients treated with GKRS in our center and address the outcomes.
Multiple intracranial meningiomas (MIMs) are rare when not associated with neurofibromatosis. They are the presence of ≥ 2 spatially separated synchronous or metachronous lesions. The prevalence rate of those tumors varied from 2.3 to 8.9% of all intracranial meningiomas, usually benign in 95% of cases. The incidence of multiple meningiomas is climbing, which may indicate more sensitive diagnostic modalities or increased exposure to environmental risk factors [1, 4, 3, 11, 23, 24, and 26]
Intracranial meningiomas are higher in females (65%), and this preponderance is even more prevalent in MM (70-90%). Like solitary meningiomas, MMs can appear at any location. The supratentorial area is commonly predominant at the convexity / falcine/parasagittal, followed by the skull base location and the posterior fossa, which remains rare. Although MMs are usually located in the same hemisphere, they can be bilateral. [23, 25, 26]
To date, surgical resection for growing symptomatic MIM is the mainstay treatment modality. However, the surgical operation of MIMs is still challenging for neurosurgeons because of the number and locations of tumors, such as the brainstem, skull base, or other eloquent areas.[2, 6, 19]
Many studies have been performed to establish the safety and effectiveness of GKRS for solitary meningiomas. However, there are limited data regarding the treatment of MIMs by GKRS, and the available evidence includes only limited cases. [2, 4, 6, 8,10,11,16, 22]
Whether the established effectiveness of GKRS in treating solitary CSMs is similar to the outcome with bilateral CSMs is still not determined and needs to be investigated and addressed.
Objective
This retrospective case series aims to report radiological identified five patients with symptomatic bilateral CSMs (10 tumors) treated with GKRS at our institution, in addition, to analyzing tumors response and treatment-related morbidity.
Material and Methods
Patient population: The reported five patients with bilateral CSMs represented 0.5 % of all treated intracranial meningiomas in our center between 2005- 2020. Two patients were excluded from the series (one had nasopharyngeal adenocarcinoma infiltrating the skull base extended into both cavernous sinuses, and the other did not complete the regular follow-up).
The characteristics and features of these retrospective cases are presented in Table 1.
Table 1 Summary of characteristics in the reported 5 patients with bilateral CSMs* treated with GKRS
Case No
| Sex | Age | TV* in cc*
| Clinical presentation | Other meningiomas in addition to the Bilateral CSMs at presentation | ||
Right | Left | Right side | Left side | ||||
1
| Female | 53 | 6.5 | 3.8 | 3rd, 4th, 6th CNs Ophthalmoplegia. | Trigeminal pain |
|
2
| Female | 40 | 4.5 | 3.2 | 3rd CN+ Visual impairment | Trigeminal paraesthesia | Newly developed small convexity Meningioma post-GKRS., on follow-up |
3
| Female | 35 | 1 | 9 | Trigeminal pain | 3rd CN+ Visual impairment& Exopthlomus |
|
4
| Female | 45 | 1.95 | 5.08 | Visual impairment | Visual impairment | Left large frontal convexity operated upon & Small right occipital follow-up |
5 | Female | 45 | 7.5 | 3.6 | 3rd, 4th, 6th CNs Ophthalmoplegia | Trigeminal pain | Right frontal convexity meningioma underneath skull bone hyperostosis on follow-up |
cc*=cubic centimeter, TV*= Tumor volume, CSM*=cavernous sinus meningioma
All reported patients were females; the median age at presentation was 45 years, and the median follow-up period was 74 months (range 40–132 months). Patients were diagnosed with benign meningioma based on the natural course of the disease and the radiological features. The typical natural course of benign meningioma includes a long medical history, slow tumor progression, and no history of cancer metastasis. Radiological features include wide dural tail attachment, clear boundaries, and uniform MRI contrast enhancement. Patients were deemed eligible for GKRS if the tumor is typically located at cavernous sinus ≥ 3cm in maximum diameters uniformly contrast-enhanced.
GKRS was the primary treatment for all reported CSM patients. None of the reported cases had associated clinical or radiological evidence of neurofibromatosis type II.
Three patients had GKRS for their tumors in two separate sessions 3- 12 months apart, starting with the larger side, which was usually more clinically symptomizing. The volume of both CSM in those patients was >8cc. Two patients were treated for both CSMs in a single session; the volume of both lesions was < 8cc>
Pre-GKRS neurological manifestations: Neurological manifestations are usually predominant toward the larger CSM, with moderate to minimal manifestations toward the smaller tumor side. All patients presented with different degrees of headache. Four patients presented with diplopia and ocular movement disorders (4 had oculomotor nerve palsy, 2 had abducens nerve palsy, and two had apparent ophthalmoplegia). Three patients presented with trigeminal pain, and one showed trigeminal tingling and paraesthesia. Three patients presented with visual impairment, one of them had, in addition, left eye exophthalmos.
Upon presentation, two patients had other intracranial meningiomas in addition to the bilateral CSMs, and another patient developed a new surface meningioma detected through the follow-up period.
Management and gamma knife procedure: The Elekta-Leksell Gamma Knife (models B, and 4-C, depending on the year of treatment); was used to treat the reported six patients. Four patients were treated in a single GKRS session for both defined CSM, and two were treated in separate sessions because of tumor volume. The standard stereotactic Leksell G- frame is applied to the head after local anesthesia and placed low and anterior as possible. 8-mm collimator was the commonly used helmet, and in cases where the optic pathway was in the vicinity of radiation, doses the 4-mm collimator was also used. The 72° angle was applied in many cases so that the radiation beams became parallel to the optic pathway, avoiding harming it. The target localization was determined with high-resolution stereotactic contrast MRI T1 and T2 coronal and axial-weighted sequences, which displayed the optic path and cranial nerves. Slices were performed on 2-mm thickness without gap and at zero angles. Treatment planning was performed with the Elekta Leksell Gamma Plan. The median tumor volume was 4.34cc (range 1–9 cc). The median tumor peripheral prescription dose (PPD) was 14.5Gy (range 12-15Gy), the median isodose line was 37.5% (range 35-55%), and the median maximum dose was 36Gy (range 30- 42.9Gy). Table 2
Table 2 GKRS treatment parameters of the reported 5 patients with bilateral CSMs* and outcomes
Case
| No of GKRS Sessions | Median PPD* | Median Isodose line% | Median Maximum dose | Median% Coverage | Follow-up Period / months | Tumor control | Clinical control |
1
| Each CSM treated in a separate session | 14.5 | 35 | 41.5 | 96 | 132 | Controlled& Decreased | Improved |
2
| Both CSM treated in the same session | 15 | 38 | 40.2 | 95 | 108 | Controlled& Stable | Stable |
3
| Each CSM treated in a separate session | 13.5 | 35 | 34.6 | 92 | 40 | Lost control& Progress | deteriorated |
4
| Both CSMs treated in the same session | 12 | 35 | 36.3 | 97 | 84 | Controlled& Stable | Improved |
5
| Each CSM treated in a separate session | 12 | 37.5 | 32.4 | 97.5 | 52 | Controlled& Decreased | Improved |
mos*=Months, PPD*=Peripheral prescription dose, CSM*=cavernous sinus meningioma
Clinical and Radiological and follow-up: Patients who underwent GKRS at our center were regularly followed up at the outpatient after 6 months post-GKRS, then yearly afterward for five years, after which follow-ups were done each two years or whenever indicated. The clinical follow-up was performed by neurological evaluation and ophthalmological testing. The reported outcomes were either clinical control (stable or improved) or worsened.
Radiological follow-up, including high-resolution contrast MRI, T1, and T2 sequences images compared to the GKRS treatment stereotactic neuroimaging. The median follow-up period was 74 months (40-132 months). Tumor growth was controlled is considered if both or either treated tumors shrinkage ≥ 10% or unchanged. Loss of tumor control was considered whenever either of the treated bilateral tumors increased in size ≥ 10%.
Results
All reported five bilateral CSMs patients were females. A total of 10 symptomatic benign CSM tumors were radiologically identified and treated with GKRS, with a median age at presentation of 45 years (range 35-56 years).
Clinical outcome: The overall clinical control at the last evaluation was achieved in 4 patients (80%), including improvement in CNs function in 3 patients, and one remained stable. Three patients who presented with eye movement disorders improved or recovered, and one remained stable. None of the patients presented with normal visual acuity and standard field of vision before treatment experienced visual deterioration. Among the three patients presenting with visual disturbances pre-GKRS, one improved in the visual field and remained stable. One patient developed worsening preexisting visual impairment with progressive exophthalmos in the left eye. This particular patient had concomitant confirmed tumor progression 40 months post-GKRS.
Tumor outcome: At the last recent follow-up contrast MRI evaluation, tumor size was controlled in 4 patients (80%), two patients achieved tumor size evident reduction, and two had stable tumor sizes. After 40 months post-treatment, one patient was confirmed to develop an increase in treated left-side CSM tumor size with deterioration of left eye vision and progressive exophthalmos.
Estimated survival free of radiographic tumor progression rates at 3, 5, and 7 years following GKRS were 100%, 80%, and 75%, respectively. No mortality-related GKRS was reported in this case series.
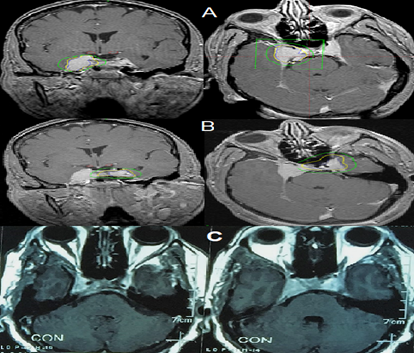
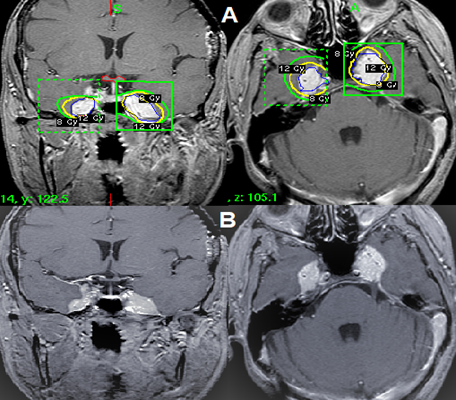
Contrast MRI brain for a female patient 56 years old with bilateral cavernous sinus meningiomas. (A) Stereotactic MRI at first GKRS session in 2011; for the right cavernous sinus meningioma (6.5cc volume treated with 14Gy to 35% isodose line). (B) Stereotactic MRI at the 2nd GKRS session in 2012; for left cavernous sinus meningioma (3.8cc volume treated with 15Gy to 35% isodose line). (C) Follow-up contrast MRI 11 years post-GKRS, revealed some reduction of both treated cavernous sinus meningiomas.
Discussion
The literature about MIMs is relatively scarce; most published papers are case reports or small case series. Management of solitary meningioma has been extensively studied; however, similar Knowledge for multiple intracranial meningiomas remained limited. Approximately two-thirds of patients with multiple meningiomas require therapy, but only one-third need active treatment. [9, 26]
The multiplicity of intracranial meningioma is uncommon and represents 1-10% in the literature, particularly if not associated with neurofibromatosis type II. The treatment strategy decision, outcome, and natural history of MIMs still need to be determined. [3, 9, 11, 13, 23, 24, 25, and 26]
In a total of 1106 meningioma patients treated with GKRS at our center between 2005- 2020, 96 patients (8.7%) had MIMs. Among those treated MIM patients, we reported five patients with clinical and images-defined benign bilateral cavernous sinus meningiomas (10 tumors).
Tsermoulas G. et al. 2018, in a study of 133 consecutive MIMs patients, reported female/male ratio was higher (3.5:1) compared with the 2:1 ratio reported for single lesions. [26]
It is unclear why female preponderance is significantly higher in multiple lesions. However, the recent hypothesis is that hormonal dependency may be higher, as suggested by more robust progesterone expression in these tumors compared with their single counterparts. Genetic factors may enhance the potential for tumorigenesis in women. [9, 13, 25,26]
Our results for female predominance in multiple intracranial meningiomas followed those obtained in the literature [9, 23, 24, 25, and 26]. All reported patients in this series were females, and none reported cases had associated clinical or radiological evidence of neurofibromatosis type II.
Complete removal of cavernous sinus meningioma (CSM), including its dural base, is impossible without significant potential risks. Reported gross-total resection rates for CSM have varied between 12% and 80%; however, after surgery, the mortality rates have ranged from 0% to 7%, and morbidity rates are between 10% and 65%. [10, 11, 12] During the last two decades, numerous Radiosurgical series related to CSM have reported tumor control rates that range from 88% to 100% and a low rate of treatment-related complications. However, there are limited data regarding the treatment of MIMs by GKRS, and the available evidence includes only limited cases [7, 17, 18, 19, 20,22]
Clinical outcome: In this report, three patients had GKRS in two sessions for the identified bilateral CSMs (volumes >8cc), and two patients were treated for both CSMs in the same session with a total tumor volume <8cc>
Overall clinical control was achieved in 4 patients (80%) in this case series. At the last clinical evaluation, three patients with ocular movement disorders improved or recovered, and one remained stable. Patients who presented with total ophthalmoplegia recovered with confirmed radiological tumor reduction. None of the patients who presented with normal visual acuity and standard field of vision before treatment experienced visual deterioration after GKRS. For those presented with visual disturbances pre-GKRS, one improved, one remained stable, and one worsened with preexistent visual impairment. This particular patient acquired in addition tumor size progression. Trigeminal and facial pain improved in two patients.
Régis et al. 2000; studied 92 patients with benign cavernous sinus meningiomas who underwent GKRS at 30.5 months (range 12-79 months). There was no new oculomotor deficit observed. Among the 54 patients with oculomotor nerve deficits, 15 improved, eight recovered, 30 remained stable, and one worsened. [18] Park et al. 2019; analyzed the outcome of GKRS in 200 patients with CSMs and found that 44 patients (26%) improved existent cranial nerve deficit, and 116 patients (58%) remained clinically stable. A decline in CN function was observed in 25 patients, and permanent CNs deficits were acquired in 15 patients. [16] The favorable clinical outcomes of GKRS for bilateral CSMs in our case series did not differ from the former series with solitary CSMs.
Tumor control: Tumor growth control was achieved in 4 patients (80 %). Tumor reduction was observed in 2 and remained stable in size in 2 patients. One patient developed MRI evidence of tumor-size progression of the treated left CSM toward the left optic foramen with intra-orbital extension. In contrast, the treated right side CSM was stable. This patient was operated on for partial tumor reduction and orbital De-roofing 40 months post-GKRS.
Nicolato et al. published a retrospective series evaluating 122 benign cavernous sinus meningiomas treated with GKRS at a marginal dose of 14.6Gy. After a median follow-up period of 48.9 months, disease-free progression over 5 years was 96.5 % [15]. Lee et al. examined 159 cases of cavernous sinus meningioma treated with GKRS at a marginal dose of 13Gy; the control rate was 93.1 % over 10 years. [12]
Park et al. 2019, retrospectively assessed tumor control outcomes 5–18 years after GKRS in 200 patients with CSMs; the authors reported tumor volume regressed in 121 (61%) patients, was unchanged in 49 (25%) and increased in 30 (15%), with overall tumor control of 85%. Actuarial tumor control rates at the 5-, 10-, and 15-year follow-ups were 92%, 84%, and 75%, respectively. [16]
Estimated survival free of radiographic tumor progression rates at 3, 5, and 7 years following GKRS were 100%, 80%, and 75%, respectively. Most published series reported a high tumor control rate for solitary CSM post-GKRS ranging from 85-96.5%. Although our reported GKRS favorable outcomes were for bilateral CSMs, they were very much following reported outcomes for solitary CSMs.
GKRS provides durable tumor control and a low risk of new cranial nerve deficits for small - medium-volume bilateral patients. Nevertheless, it remains a debate on how to best manage patients with large CSMs. One option is to perform initial non-radical surgery to reduce the tumor size to a volume more compatible with GKRS. [13, 16, 18]
For small size, none, symptomatic, or accidentally identified CSM, a regular follow-up is sufficient and active treatment should be offered for symptomatic or growing tumors. Microsurgery should be advised for large extensive CSMs (diameters >3 cm), especially those with significant visual affection, to decompress the optic path and debulk the tumor. [1, 5, 14]
Study strengths and limitations: The strengths of our study include a relatively homogenous patient population and regular follow-up documentation. With the limited number of patients and the retrospective nature, one must be careful in comparing the outcomes. Whether the established effectiveness of GKRS in treating solitary CSMs is similar to the outcome with bilateral CSMs is still to be determined. This case series report has several limitations that must be considered.
Conclusion
Bilateral cavernous sinus meningiomas, although rare yet, create therapeutic challenges through the multiplicity and the usual involvement of critical neurovascular. GKRS offered a safe, effective long-term tumor and clinical control for small to medium-sized symptomatic benign bilateral CSMs as much as it usually does with solitary cavernous sinus meningioma.
Retrospective study: For this study, formal consent is not required; it does not contain any studies with human participants.
Funding: No funding was received for this research.
Competing Interests: The authors declare that they have no competing interests and certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest.
Acknowledgments: We want to thank Dr. Tiit Rahn, MD, Ph.D. for long-term assistance in many patients' evaluation and management, Dr. Mahmoud El Badrawy for assistance in dose calibration, treatment dose conformity, and patient management, and we are grateful to Mrs. Hadeer Ezz for her sincere efforts in through patient’s direct communications and collection of patients paper and electronic data.
References
- Abdel-Aziz KM, Froelich SC, Dagnew E, Jean W, Breneman JC, Zuccarello M, van Loveren HR, Tew JM Jr. Large sphenoid wing meningiomas involving the cavernous sinus: conservative surgical strategies for better functional outcomes. Neurosurgery. 2004 Jun;54(6):1375-83; discussion 1383-4. doi: 10.1227/01.neu.0000125542.00834.6d. PMID: 15157294.
View at Publisher | View at Google Scholar - Andrew T Hale, Wang L, Strother MK, Chambless LB. Differentiating meningioma grade by imaging features on magnetic resonance imaging. J Clin Neurosci. 2018 Feb; 48:71-75. doi: 10.1016/j.jocn.2017.11.013. Epub 2017 Nov 22. PMID: 29174756.
View at Publisher | View at Google Scholar - BJ raújo Pereira, Nogueira de Almeida A, Pires de Aguiar PH, Paiva WS, Teixeira MJ, Nagahashi Marie SK. Multiple Intracranial Meningiomas: A Case Series and Review of the Literature. World Neurosurg. 2019 Feb;122: e1536-e1541. doi: 10.1016/j.wneu.2018.11.097. Epub 2018 Nov 22. PMID: 30471445.
View at Publisher | View at Google Scholar - Chen W, Wang X, Liu F, Chen J. Gamma Knife Radiosurgery for Patients with Multiple Intracranial Meningiomas. World Neurosurg. 2019 Aug;128: e495-e500. doi: 10.1016/j.wneu.2019.04.184. Epub 2019 Apr 30. PMID: 31048056.
View at Publisher | View at Google Scholar - Cusimano MD, Sekhar LN, Sen CN, Pomonis S, Wright DC, Biglan AW, Jannetta PJ. The results of surgery for benign tumors of the cavernous sinus. Neurosurgery. 1995 Jul;37(1):1-9; discussion 9-10. doi: 10.1227/00006123-199507000-00001. PMID: 8587667.
View at Publisher | View at Google Scholar - Ge, Y., Liu, D., Zhang, Z., Li, Y., Lin, Y., Wang, G., Zong, Y., & Liu, E. (2019). Gamma Knife radiosurgery for benign intracranial meningiomas: follow-up outcome in 130 patients, Neurosurgical Focus FOC, 46(6), E7. DOI: https://doi.org/10.3171/2019.3.FOCUS1956 PMID: 31153153
View at Publisher | View at Google Scholar - Hasegawa T, Kida Y, Yoshimoto M, Koike J, Iizuka H, Ishii D. Long-term outcomes of Gamma Knife surgery for cavernous sinus meningioma. J Neurosurg. 2007 Oct;107(4):745-51. doi: 10.3171/JNS-07/10/0745. PMID: 17937218.
View at Publisher | View at Google Scholar - Haselsberger K, Maier T, Dominikus K, Holl E, Kurschel S, Ofner-Kopeinig P, Unger F. Staged gamma knife radiosurgery for large critically located benign meningiomas: evaluation of a series comprising 20 patients. J Neurol Neurosurg Psychiatry. 2009 Oct;80(10):1172-5. doi: 10.1136/jnnp.2008.156745. PMID: 19762911.
View at Publisher | View at Google Scholar - Huang H, Buhl R, Hugo HH, Mehdorn HM. Clinical and histological features of multiple meningiomas compared with solitary meningiomas. Neurol Res. 2005 Apr;27(3):324-32. doi: 10.1179/016164105X39932. PMID: 15845217.
View at Publisher | View at Google Scholar - Jang CK, Jung HH, Chang JH, Chang JW, Park YG, Chang WS. Long-Term Results of Gamma Knife Radiosurgery for Intracranial Meningioma. Brain Tumor Res Treat. 2015 Oct;3(2):103-7. doi: 10.14791/btrt.2015.3.2.103. Epub 2015 Oct 30. PMID: 26605265; PMCID: PMC4656885.
View at Publisher | View at Google Scholar - Koech F, Orege J, Ndiangui F, Macharia B, Mbaruku N. Multiple intracranial meningiomas: a review of the literature and a case report. Case Rep Surg. 2013; 2013:131962. doi: 10.1155/2013/131962. Epub 2013 Aug 29. PMID: 24069543; PMCID: PMC3773437.
View at Publisher | View at Google Scholar - Lee JY, Niranjan A, McInerney J, Kondziolka D, Flickinger JC, Lunsford LD. Stereotactic radiosurgery providing long-term tumor control of cavernous sinus meningiomas. J Neurosurg. 2002 Jul;97(1):65-72. doi: 10.3171/jns.2002.97.1.0065. PMID: 12134934.
View at Publisher | View at Google Scholar - Maiuri F, Mariniello G, Guadagno E, Barbato M, Corvino S, Del Basso De Caro M. WHO grade, proliferation index, and progesterone receptor expression are different according to the location of meningioma. Acta Neurochir (Wien). 2019 Dec;161(12):2553-2561. doi: 10.1007/s00701-019-04084-z. Epub 2019 Oct 21. PMID: 31637512.
View at Publisher | View at Google Scholar - Nanda A, Thakur JD, Sonig A, Missios S. Microsurgical resectability, outcomes, and tumor control in meningiomas occupying the cavernous sinus. J Neurosurg. 2016 Aug;125(2):378-92. doi: 10.3171/2015.3. JNS142494. Epub 2016 Jan 8. PMID: 26745483.
View at Publisher | View at Google Scholar - Nicolato A, Foroni R, Alessandrini F, Bricolo A, Gerosa M. Radiosurgical treatment of cavernous sinus meningiomas: experience with 122 treated patients. Neurosurgery. 2002 Nov;51(5):1153-9; discussion 1159-61. doi: 10.1097/00006123-200211000-00009. PMID: 12383360.
View at Publisher | View at Google Scholar - Park KJ, Kano H, Iyer A, Liu X, Tonetti DA, Lehocky C, Faramand A, Niranjan A, Flickinger JC, Kondziolka D, Lunsford LD. Gamma Knife stereotactic radiosurgery for cavernous sinus meningioma: long-term follow-up in 200 patients. J Neurosurg. 2018 Jul 1:1-10. doi: 10.3171/2018.2. JNS172361. Epub ahead of print. PMID: 30028261.
View at Publisher | View at Google Scholar - Pollock BE, Stafford SL, Utter A, Giannini C, Schreiner SA. Stereotactic radiosurgery provides equivalent tumor control to Simpson Grade 1 resection for patients with small- to medium-size meningiomas. Int J Radiat Oncol Biol Phys. 2003 Mar 15;55(4):1000-5. doi: 10.1016/s0360-3016(02)04356-0. PMID: 12605979.
View at Publisher | View at Google Scholar - Roche PH, Régis J, Dufour H, Fournier HD, Delsanti C, Pellet W, Grisoli F, Peragut JC. Gamma knife radiosurgery in the management of cavernous sinus meningiomas. J Neurosurg. 2000 Dec;93 Suppl 3:68-73. doi: 10.3171/jns.2000.93.supplement. PMID: 11143266.
View at Publisher | View at Google Scholar - Samblas J, Luis Lopez Guerra J, Bustos J, Angel Gutierrez-Diaz J, Wolski M, Peraza C, Marsiglia H, Sallabanda K. Stereotactic radiosurgery in patients with multiple intracranial meningiomas. J BUON. 2014 Jan-Mar;19(1):250-5. PMID: 24659672.
View at Publisher | View at Google Scholar - Sheehan JP, Starke RM, Kano H, Kaufmann AM, Mathieu D, Zeiler FA, West M, Chao ST, Varma G, Chiang VL, Yu JB, McBride HL, Nakaji P, Youssef E, Honea N, Rush S, Kondziolka D, Lee JY, Bailey RL, Kunwar S, Petti P, Lunsford LD. Gamma Knife radiosurgery for sellar and parasellar meningiomas: a multicenter study. J Neurosurg. 2014 Jun;120(6):1268-77. doi: 10.3171/2014.2. JNS13139. Epub 2014 Mar 28. PMID: 24678777.
View at Publisher | View at Google Scholar - Spiegelmann R, Cohen ZR, Nissim O, Alezra D, Pfeffer R. Cavernous sinus meningiomas: a large LINAC radiosurgery series. J Neurooncol. 2010 Jun;98(2):195-202. doi: 10.1007/s11060-010-0173-1. Epub 2010 Apr 20. PMID: 20405308.
View at Publisher | View at Google Scholar - Starke RM, Przybylowski CJ, Sugoto M, Fezeu F, Awad AJ, Ding D, Nguyen JH, Sheehan JP. Gamma Knife radiosurgery of large skull base meningiomas. J Neurosurg. 2015 Feb;122(2):363-72. doi: 10.3171/2014.10. JNS14198. Epub 2014 Dec 5. PMID: 25479122.
View at Publisher | View at Google Scholar - Sun C, Dou Z, Wu J, Jiang B, Iranmanesh Y, Yu X, Li J, Zhou H, Zhong C, Peng Y, Zhuang J, Yu Q, Wu X, Yan F, Xie Q, Chen G. The Preferred Locations of Meningioma According to Different Biological Characteristics Based on Voxel-Wise Analysis. Front Oncol. 2020 Aug 21; 10:1412. doi: 10.3389/fonc.2020.01412. PMID: 32974148; PMCID: PMC7472960.
View at Publisher | View at Google Scholar - Terrier LM, François P. Méningiomes multiples [Multiple meningiomas]. Neurochirurgie. 2016 Jun;62(3):128-35. French. doi: 10.1016/j.neuchi.2015.12.006. Epub 2016 May 24. PMID: 27234913.
View at Publisher | View at Google Scholar - Touat M, Lombardi G, Farina P, Kalamarides M, Sanson M. Successful treatment of multiple intracranial meningiomas with the antiprogesterone receptor agent mifepristone (RU486). Acta Neurochir (Wien). 2014 Oct;156(10):1831-5. doi: 10.1007/s00701-014-2188-4. Epub 2014 Jul 31. PMID: 25078073.26
View at Publisher | View at Google Scholar - Tsermoulas, G., Turel, M. K., Wilcox, J. T., Shultz, D., Farb, R., Zadeh, G., & Bernstein, M. (2018). Management of multiple meningiomas, Journal of Neurosurgery JNS, 128(5), 1403–1409. doi.org/10.3171/2017.2. JNS162608 PMID: 28731398
View at Publisher | View at Google Scholar