Archive : Article / Volume 2, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5070/007
Healthy Me: A retrospective review of a pediatric resident run clinic for children and with overweight or obesity
Associate Professor Pediatrics, Atrium Health Navicent Macon, Georgia, United States.
Christy Peterson, MD.
Christy Peterson, (2023). Healthy Me: A retrospective review of a pediatric resident run clinic for children and with overweight or obesity. Journal of Obesity and Fitness Management. 2(1). DOI: 10.58489/2836-5070/007.
© 2023 Christy Peterson, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 05-01-2023
- Accepted Date: 13-01-2023
- Published Date: 26-01-2023
sleep apnea, cardiovascular disease, fatty liver disease, gall stones, diabetes, skin conditions, orthopedic problems
Abstract
Objective: Using motivational interview techniques, we aimed to encourage families to make healthy lifestyle choices with the goal of a decreased childâs body mass index percentile for age over time. Methods:We designated one afternoon each week to a special clinic focusedon healthy lifestyle habits. Parents were referred to our clinicfrom private pediatricians in the area. During the initial visit which included the parent, the child and the resident, plus or minus a nutritionist or a family and marriage therapist, we focused discussion on assessment of current lifestyle habits and then on goal setting regarding lifestyle, exercise and diet. Patients and their families were seen every 1-3 months. During subsequent visits we focused discussion on reassessment of previously stated goals. Results: Over one half of our patients achieved a lower or steady body mass index percentile for age compared to their starting percentile. Conclusions: Simple and effective techniques can be incorporated into every pediatric visit to helpeducate and encouragefamilies with a child with overweight or obesity.
Introduction
Childhood obesity is a serious healththreat because it is associated with many serious medical conditions including sleep apnea, cardiovascular disease, fatty liver disease, gall stones, diabetes, skin conditions, orthopedic problems and others [1]. Childhood obesity is also a threat to psychological healthas it leads to emotional problems [1]. The American Academy of Pediatrics (AAP) Periodicity Schedule recommends that providers who see children for Preventative Pediatric Health Care document a Body Mass Index (BMI) starting at the age of two [2]. The AAP recommendations regarding the prevention of child and adolescent overweight and obesity are designed with the hope that by identifying elevated BMI and unhealthy eating or poor physical activity habits, providers can lower the risk of thesechildren becoming obeseadults [2]. The BMI is plotted against age matched peers to note a percentile. The Centers for Disease Control defines obesity for children as having a body mass index that is equal to or greater than 95 % of age and sex matched controls [3]. Overweight is defined as having an age and sex matched BMI percentile less than the 95th percentile but greater than the 85th percentile [3]. Currently approximately 1 in 3 US children meet criteria for being overweight or obese [4]. Pediatric Obesity is increasing in severity and prevalence across the United States [3]. Even in the preschool years many children are already found to have obesity, but the problem increases in prevalence with increasing ages of children [3]. Morbid obesity, defined as having a BMI greater than or equal to 140 % of the 95th percentile [3], is the fastest growing subcategory and is linked to severe health risks in adulthood [5]. In addition, the 2012 Institute of Medicine report "Accelerating Progress in Obesity Prevention” sites primary care providers with the task of preventing Obesity.
We approached our project with the idea that perhaps if interventions to shape healthy habits are applied early enough in a child’s life the disease of obesity can be altered in a positive direction, away from Morbid Obesity, a prevention rather than a cure. If this change were possible, it would save significant health care costs over the course of the child’slife [6].
Methods
Born perhaps out of necessity, in 2013 we initiated our “Healthy Me Clinic.” We, the providers of a resident run clinic, welcomed children as young as 3 and as old as 18 into our obesity intervention clinic, called the Healthy Me Clinic. Residents and Attending physicians followed these children for an average of 2.6 years. In this clinic pediatric residents saw patients specifically to address their overweight or obesity according to their BMI measured as part of routine surveillance for all patients, regardless of Chief Complaint, in our hospital owned pediatric office. We established a yearly training program for residents and attending providers in obesity statistics, obesity prevention, obesity and weight loss management and motivational interviewing techniques in 2013. Any child, between the ages of 3 and 18, identified at any visit to have a BMI percentile greater than the 95th percentile was offered the opportunity to return for a visit in our Healthy Me Clinic. Each child included in our data was seen at least once for an “initial Healthy Me Clinic” visit where an initial BMI percentile was obtained. Each child was also seen at least one more time following that initial Healthy Me Clinicvisit where a final BMI percentile was obtained to compare to the initial BMI percentile. Data collection was complete December 2019. During the initial Healthy Me visit, lifestyle choices of the family were assessed with 5 standardized questions, one in each of 5 areas of intervention, using a 5-point scale where unhealthy lifestyle choices were on the left (lower numbers)and healthy lifestylechoices were on the right (higher numbers). The child was then asked to choose one of the 5 areas to move one step toward the “healthy” position.As an example, choices includedeating more freshfruits and vegetables, eating out less or increasing exercise. Using motivational interviewing techniques, the child was asked to make one, and only one, change over the next 1-3 months and then to return for a follow up visit after that amount of time. Each child was encouraged to continue with this pattern of meeting with the provider every 1-3 months until their BMI percentile dropped below the 85th percentile for age. During each visit the provider used a developmentally appropriate approach to assess the child’s willingness to make changes. Considering the family dynamics, the provider then recounted the decisions made by the child and the family. We chose to call the clinic, Health Me, to remove any stigma associated with obesity and to focus on healthy lifestyle choices rather than weight loss. Teaching healthy lifestyle choices was our goal. There is plenty of research in the area of childhood obesity and perhaps this very fact testifies that no solution is apparent. Many interventions, be it prevention or treatment of childhood obesity, have shown positive advances but often the follow up study indicates that these advanceswere not sustained over time [7,8,9]. Several of the hundreds of studies surrounding the prevention of or intervention for childhood obesity use motivational interviewing and when placed in a systematic review process the outcome is often positive [12]. Our results are consistent with these previous studies. A little over 2/3 of our patients, who were initially seen in this Healthy Me Clinic returned for a subsequent visit with us. If they returnedone or multiple times the most recent BMI percentile was collected in 2018 or 2019 as the “final BMI.” The time between initial visitand final BMI ranges from 2 monthsto 5 years but averages at 2.6 years.
Children were seen as many times and as often as they attended the office. Many subsequent visits were incorporated into other routinevisits once a child was identified as a “Healthy Me,” patient. It is likely that participation in the Healthy Me clinic as a provider changes that providers practice as it pertains to dealing with childhood obesity identified inpatients presenting for any complainteven outside of the HealthyMe clinic. This phenomenon is evident in that we have now moved to seeing patients for “Healthy Me” visits all 5 days of the week and any provider with a history of working in the Healthy Me clinic is eligible for this assignment of patients.
Results and Discussion
Atotal of 304 patients attendedat least one visit in the HealthMe Clinic over the 6 years from 2013 to 2019. Of the total patients, 55.3 percent or 167 self-identified as female. Of the total patients, 69.9 percent self-identified as black, 17.9 percent self- identified as Hispanic, 11.6 percent self-identified as white and 0.3 percent as Asian. Age categories were determined by “age at 1st visit,” with the mean age at 1st visit being 11 years of age. The average initial BMI percentile was 98.4 %. The average final BMI percentile was 97.6 %. Approximately 2/3 of our patients initially seen in the Healthy Me clinic returned for a subsequent visit before December 2019. Of those who returned within the 6-year period for any visit where a BMI was evaluated, 2/3 had a similar or improved BMI percentile at most recent follow up. See table 1 and figure 1. This result seems to be consistent across all age groups. See table 2 and figures 2-5.As expected, the largest percentage of patients with BMI percentile improvement was seen in the youngest age group (n = 44) at 73 percent of patients remaining at or below their original BMI percentile at most recent follow up. See table 2 and Figure 2. The smallest percent of patients showingimprovement was seen in the ages of 7-11 (N = 95) at 50
%.See table 2 and figure 3. A similar percentage of patients who stayed the same or dropped in BMI percentile was seen in the 12-15 and the 16-18 age groups (N = 99 and 40 respectively) which was 61% and 65 % respectively. See table 2 and figures 4 and
5. Our “lost to follow up” rate was about 1/3 of our patients. One could ask why we had so many persons not return for a second visit. The failure to return could be due to weight gain since the initial visit. Or it is also possible that the patient had such success that the family no longer felt the need to seek help. If we assume that all the patients who failed to return for a 2nd visit gained weight and thus had a higher BMI percentile for age, our resultswould be about 40 % having lost or remainedthe same. Statistical analysis indicates that any differences found based on gender or race were not significant. Other variables measured such as how many total visits thepatient attended were also not significant.
Conclusion
“An ounce of prevention is worth a pound of cure,” famously stated by Benjamin Franklin in the 1700’s surely applies to the disease of obesity. Not only is adult obesity prevention a public health priority, it is also a crucial component of pediatric care.11 Our study shows that it is possible to achieve success in pediatric patients with simple methods. Our methods included talking about body mass index at an early age and requesting that patients or their parents who are willing to change, choose their own strategy to address the obesity or overweight issue. Our clinic was designed by a resident and lead by residents who had been specifically trained in motivational interviewing techniques as well as in recognizing obesity related issues. We believe that some training is needed to achieve success.Providers involved in our HealthyMe clinic were encouraged by our findings but discouraged by the number ofdropouts. Even if we count all the patients who failed to return for a 2nd visit with those who gained weight, or increased their BMI percentile, the success rate is still encouraging enough to continue our efforts. Further study is needed to determine if the success in childhood continues into adulthood. Repeatedly, weight loss attempts for adults have failed and often lead to worsening of the obesity. Is it an education problem? Is it a motivation problem? Or is it a problem of habits established at a young age, carried into adulthood, leading to a dependency on an abundance of calories. Every pediatrician wants to help theirpatients achieve a happy, healthybody to take into adulthood.
Perhaps by discussing lifestylehabits early in a child’slife we can call attentionto the bad habits and introduce good habits that will carry them intoa healthy adulthood.
Further study is also needed to determine what factors including presenting lifestyles or lifestyle modifications chosen by the patients and their families affected greater BMI percentile improvement. Comparative studies in our clinic will be difficult because every provider that has worked in the Healthy Me clinic has incorporated these methods into their routine practice and it would be very difficult to find a group of patients attending our clinic who has not been touched by our techniques.
Acknowledgements: I would like to recognize Dr. Julia Thompson, MD for the naming and original idea for this clinic. Yera Chokshi, MD, Jenelle Fernandez, MD, BrittanyLord, MD, LynndseyParker, MD, and Jaimie Woods, MD helpedwith the originaldesign of the study. Along with the designers of the study, Kristen Bird, MD and Monica Patel, MD also contributed to the additionof data to the spreadsheet. As a student,Rachel Albrecht, MD, originally helped with enteringour first data points and then also as a student, Lauren Lewis, MD took over in this roll.
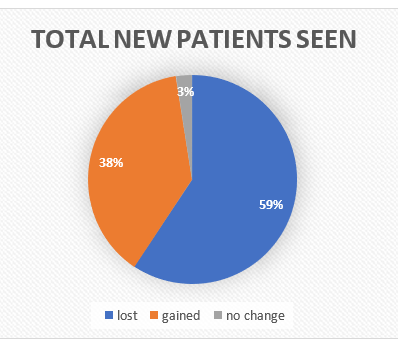
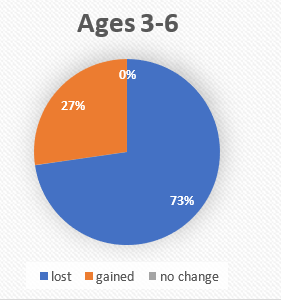
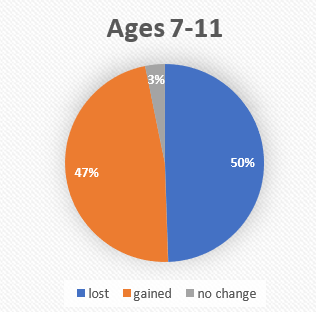
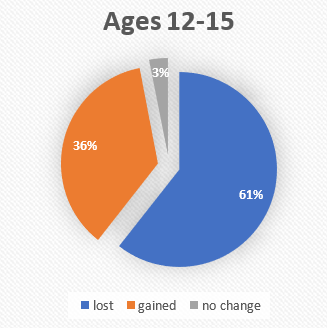
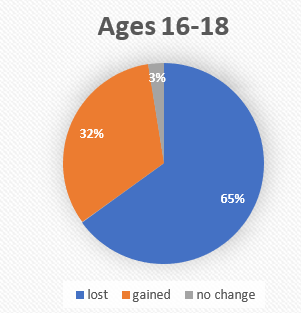
Table 1
Total Patients
| Number of patients | Percent of patients |
Total Patients |
278 |
100% |
LowerBMI % | 165 | 59% |
No change | 7 | 3% |
HigherBMI % | 106 | 38% |
Age Brackets
Table 2
| Number of patients | Percent of patients |
| Age Bracket totals | Age Bracket Percent |
Ages 3-6 | 44 | 100% |
LowerBMI % | 32 | 73% |
No change | 0 | 0% |
HigherBMI % | 12 | 27% |
Ages 7-11 | 95 | 100% |
LowerBMI % | 47 | 50% |
No change | 3 | 3% |
HigherBMI % | 45 | 47% |
Ages 12-15 | 99 | 100% |
LowerBMI % | 60 | 61% |
No change | 3 | 3% |
HigherBMI % | 36 | 36% |
Ages 16-18 | 40 | 100 % |
LowerBMI % | 26 | 65% |
No change | 1 | 3% |
HigherBMI % | 13 | 32% |
References
- Sahoo K, Sahoo B, Choudhury AK, Sofi NY, Kumar R, Bhadoria AS. Childhood obesity: causes and consequences. J Family Med Prim Care. 2015;4(2):187-192. doi:10.4103/2249-4863.154628
- Sarah E. Barlow, and the Expert Committee; Expert Committee Recommendations Regarding the Prevention, Assessment, and Treatment of Child and Adolescent Overweight and Obesity: Summary Report. Pediatrics December 2007; 120 (Supplement_4): S164–S192. 10.1542/peds.2007-2329CAMA
- Skinner AC, Ravanbakht SN, Skelton JA Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in the US children, 1999-2016. Pediatrics. 2018;141 (3):e20173459.
- Kumar S, Kelly AS. Review of Childhood Obesity: From Epidemiology, Etiology, and Comorbidities to Clinical Assessment and Treatment. Mayo Clin Proc. 2017 Feb;92(2):251-265. doi: 10.1016/j.mayocp.2016.09.017. Epub 2017 Jan 5. PMID: 28065514.
- Zolotarjova J., Ten Velde G., Vreugdenhil ACE. Effects of multidisciplinary interventions on weight loss and health outcomes in children and adolescents with morbid obesity. Obesity Reviews. 2018; 7/19:931-946. [PMID: 29701298].
- Eric Andrew Finkelstein, Wan Chen Kang Graham, Rahul Malhotra; Lifetime Direct Medical Costs of Childhood Obesity. Pediatrics May 2014; 133 (5): 854–862. 10.1542/peds.2014-0063
- Serena Broccoli, Anna Maria Davoli, Laura Bonvicini, Alessandra Fabbri, Elena Ferrari, Gino Montagna, Costantino Panza, Mirco Pinotti, Simone Storani, Marco Tamelli, Silvia Candela, Eletta Bellocchio, Paolo Giorgi Rossi; Motivational Interviewing to Treat Overweight Children: 24-Month Follow-Up of a Randomized Controlled Trial. Pediatrics January 2016; 137 (1): e20151979. 10.1542/peds.2015-1979
- Anna Maria Davoli, Serena Broccoli, Laura Bonvicini, Alessandra Fabbri, Elena Ferrari, Stefania D’Angelo, Annarita Di Buono, Gino Montagna, Costantino Panza, Mirco Pinotti, Gabriele Romani, Simone Storani, Marco Tamelli, Silvia Candela, Paolo Giorgi Rossi; Pediatrician-led Motivational Interviewing to Treat Overweight Children: An RCT. Pediatrics November 2013; 132 (5): e1236–e1246. 10.1542/peds.2013-1738
- Karp SM, Gesell SB. Obesity Prevention and Treatment in School-aged Children, Adolescents, and Young Adults-Where Do We Go from Here? Prim Prev Insights. 2015; 5:1-4. doi:10.4137/PPRI.S12291
- Kameron B. Suire, Jan Kavookjian, Danielle D. Wadsworth; Motivational Interviewing for Overweight Children: A Systematic Review. Pediatrics November 2020; 146 (5): e20200193. 10.1542/peds.2020-0193
- Daniels SR, Hassink SG; COMMITTEE ON NUTRITION. The Role of the Pediatrician in Primary Prevention of Obesity. Pediatrics. 2015 Jul;136(1): e275-92. doi: 10.1542/peds.2015-1558. Epub 2015 Jun 29. PMID: 26122812.
- Güngör NK. Overweight and obesity in children and adolescents. J Clin Res Pediatr Endocrinol. 2014 Sep;6(3):129-43. doi: 10.4274/Jcrpe.1471. PMID: 25241606; PMCID: PMC4293641.


