Archive : Article / Volume 2, Issue 2
- Research Article | DOI:
- https://doi.org/10.58489/2836-3558/009
Influence Of Baseline Comorbid Diseases on Major Depression and The Effect of Intensive Medical Treatment on Functional Mobility in Depressed Patients Compared with Those Without Depression
Centre for Neurodegenerative Diseases and Movement Disorders Kreuzbergstr. 12-16, 77709 Wolfach, Germany
Ibrahim Raoua Ouedraogo
Ibrahim Raoua Ouedraogo (2023). Influence of baseline comorbid diseases on major depression and the effect of intensive medical treatment on functional mobility in depressed patients compared with those without depressionâ.Psychiatry and Psychological Disorders (JPPD) 2 (2). DOI: 10.58489/2836-3558/009
© 2023 Ibrahim Raoua Ouedraogo, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 27-02-2023
- Accepted Date: 15-03-2023
- Published Date: 03-04-2023
Comorbidity, Major depression, Functional mobility, Partial remission, Geriatric patients.
Abstract
Objectives
Somatic diseases, depression and functional mobility were examined in a follow-up study in geriatric patients. The first aim of the study was to assess the independent and moderator effects of baseline diseases on depression before adjustment by examining whether this influence will sustain or switch after adjustment. The second aim was to explore the differential treatment outcomes in functional mobility in depressed patients versus those with no depression.
Methods
A sample of n = 1,816 multimorbid patients consisting of n = 902 with a diagnosis of major depression and their counterparts n = 914 without depression were examined at two time points. They all underwent acute rehabilitation. Those who were diagnosed with major depression received an antidepressant and psychotherapy treatment. Depressive symptoms were recorded with the Geriatric Depression Scale. Functional mobility was measured using the Tinetti Test.
Results
We found that 431 patients (47%) were in partial remission at follow-up. The results yield a significant improvement in functional mobility in both groups as an effect of the intensive rehabilitation program. These findings support published findings highlighting an overall functional health enhancement owing to a combined medical rehabilitation, antidepressant and psychotherapeutic treatment as a result of early intensive rehabilitation for elderly patients with multiple medical conditions. The findings show that elderly patients with multiple chronic conditions benefit from intensive rehabilitation, psychotherapy and antidepressant treatment within three weeks of intensive stationary treatment.
Results showed that baseline comorbid diseases (mainly focal neurologic deficits and coronary artery diseases) each act as risk factors for major depression before treatment. An intercept effect was unveiled between obesity and arterial hypertension that arises as risk factors for depression before adjustment. After adjustment, we found that baseline chronic conditions, specifically coronary artery disease, focal neurologic deficits, heart or valvular insufficiency, artificial valvular or pace maker and tumour diagnosis in respiratory organ each act as a potential risk factor for depression occurrence. The intercept effect erased after treatment. Functional health was increased significantly in both groups at follow-up. However, there was no difference in the increase of functional mobility (Tinetti Test) in non-depressed and depressed patients following the rehabilitation.
Conclusion
The results bolster up the conjecture that specific somatic diseases influence major depression before and after treatment and support an association between somatic diseases, depression, and functional health in elderly patients. In depressed and non-depressed patients, geriatric rehabilitation boosts functional mobility, which is crucial for the maintenance of autonomy in elderly patients. Major depression may hamper functional mobility rehabilitationâs outcome only if not well managed or overlooked.
Introduction
A major challenge in the context of evaluating depression in the elderly is the role of multiple medical conditions. With ageing, there is a rapid increase in the prevalence of a number of medical disorders, including heart disease, neurodegenerative disorders, depression and functional losses. The relationship between functional mobility, chronic medical problems and depression is complex, as it appears to include associations between depression, functional decline, and somatic diseases on the one hand, and separate associations that affect the outcomes for each of these domains on the other hand. Previous research has focused on connections between specific aspects of these interactions such as the relationship between increasing weakness and the presence of depression, the interdependence between treatment outcomes of chronic diseases and major depression, and the effect of somatic diseases on the course of depression. A bulk of research, which tried to identify factors associated with functional decline in multimorbid depressed patients [16, 39, 35, 37, 20, 28],
and those which assessed the relationship between somatic diseases and the outcomes of treatment for depression [2, 15, 30], did not tackle the issue of independent and intercept effects of baseline diseases suspected of being related to depression occurrence. Likewise, most published findings did not examine the treatment outcome of acute rehabilitation on functional mobility in depressed persons versus those with no depression. Although major depression is suspected of hampering the functional rehabilitation outcome, the plausible hindering effect of depression on functional mobility rehabilitation has not been examined. Whether there are differential treatment outcomes related to any specific pattern of somatic diseases, is still unexplored. It remains unclear whether there are only independent effects of baseline diseases on depression or also moderator (or intercept) effects between certain somatic diseases that impact on major depression in pre and post rehabilitation phases.
The examination of these issues may have a beneficial impact on the clinical management of elderly patients presenting with multiple medical conditions. Furthermore, the use of clinical data in order to address these issues may have a beneficial effect on clinical practice. Given the global ageing of the population, the topic of boosting functional mobility, sustain mental health and maintain autonomy has become a central paradigm in acute rehabilitation. Patients with major depression, n = 902, received an antidepressant treatment either with selective serotonin reuptake inhibitors (SSRIs) or serotonin and noradrenaline reuptake inhibitors (SNRIs) combined with a psychotherapeutic intervention. All patients involved in the sample (n =1816) received an intensive medical treatment and adhered to a scheduled rehabilitation program. In targeting major depression, the expected outcome is a partial remission that is, an improvement in 80% of symptoms of depression before release from hospital.
We hypothesized that the two groups (non-depressed and depressed) would benefit from the acute rehabilitation program. Based on the suspected hampering effect of major depression on functional rehabilitation outcome in elderly, we hypothesized that the performance in the Tinetti test at time two of assessment in non-depressed patients would be higher than those depressed at baseline. The research postulated that whereas some chronic conditions would act independently as a trigger for depression, some other would need a moderator factor (co-factor path) to trigger depression occurrence before and after adjustment.
Objectives
The present study aims at determining the influence of independent and moderator effects of baseline diseases on depression before treatment. It also intended to examine whether that purported influence will sustain or switch following acute rehabilitation and combined antidepressant and psychotherapy treatment. Furthermore, the research aims to analyse the differential treatment outcomes in functional mobility in depressed persons versus those with no depression.
Materials and Methods
Sample and procedure
We used data from a series of neuropsychological and medical diagnostic procedures run on 2,151 subjects at the Evangelic Geriatric Centre Berlin: “Evangelisches Geriatriezentrum Berlin” EGZB. The length of stay for the stationary treatment is currently three weeks. After the required admission’s medical examination (medical diagnosis, geriatric basic assessments, geriatric screening) a series of neuropsychological tests for depression and cognitive function was run in patients by senior psychologists. Patients of both sexes were eligible for the present study if they were 60 years or older, disclosed either a diagnosis of major depression or no depression, had multiple medical conditions as well as functional decline. The exclusion criteria were a diagnosis of dementia, head injury after an accident or fall, bipolar disorder, schizophrenia, delirium or terminal disease condition. Subsequent to the psychological diagnostic procedure, n = 902 patients who scored between 11 and 15 on the GDS-15 and fulfilled the clinical criteria of the ICD-10 for major depression, and n = 914 patients without depression were retrospectively maintained for the study design. This led to a sample of n = 1,816 patients (n = 902 with major depression + 914 without depression) which the study focused on. Patients of both groups fully fulfilled the Charlson comorbididy index [39] and the functional comorbidity index [37]. They all had more than six current somatic diagnoses, had functional mobility and functional ability decline and were admitted to the Geriatric Centre for acute medical treatment and rehabilitation. Medical and psychiatric diagnoses were extracted by senior geriatrics physicians and senior psychologists.
Measures
Sociodemographic characteristics
Age, gender, education, marital status and living situation (home versus nursing home) were determined at the baseline interview.
Depression: Follow-up assessment
Depression was diagnosed according to the criteria of the ICD-10 for major depression and scored using the Geriatric Depression Scale’s short form, GDS-15 [41]. This version of the scale has been shown to have good internal consistency with Cronbach’s Alpha = 0.80 [7]. All patients diagnosed with major depression scored between 11 and 15 on GDS-15 at baseline. Psychiatric diagnoses were done by senior psychologists in close collaboration with psychiatrists for medical prescription. Apart from the Lachs screening, all assessments were done at admission and shortly before discharge i.e. Follow-up assessment.
Lachs screening
The Geriatric Screening Scale [18], which was administered at admission, is an important indicator of functional disturbance and geriatric risks. It is used by family doctors and general practitioners. The World Health Organization recommends that people aged 65 years or over should be screened once a year. The scale (15 items) provides data on independence, memory, depression, social situation, dexterity action, skilfulness, flexibility, mobility and mental capacity. The scale was administered by the physician who made the basic physical examination at admission.
Tinetti gait and balance Test (Follow-up assessment)
The test of functional mobility which consists of gait and balance [34], was used to identify patients at risk of fall at admission and discharge from hospital. The test (0-28 points) analyses differential aspects of mobility, such as control, gait and balance.
Medical diagnoses (Follow-up assessment)
Medical diagnoses were extracted by senior geriatrics physicians at admission and shortly before discharge from hospital. The diagnoses are based on the International Classification of Disease [40]. Information on medication taken before admission was determined based on medical records sent either by the family doctor or the referring hospital.
Statistical Analysis
Statistical analyses used IBM SPSS version 24 for Windows. Preliminary descriptive analysis showed that Tinetti and Bi Scores were distributed normally and Type I error effect was checked for. Given the sample size (902 vs. 914 = 1,816), effect sizes were relatively large and observed powers were excellent. Descriptive analyses included means and standard deviations for continuous variables and frequencies for categorical variables. The McNemar’s Test appeared the best to make statistical decisions as to whether or not the combined medical rehabilitation, antidepressant and psychotherapeutic treatment had an effect on the outcome of depression. Contingency table modelling for dichotomous variables using the McNemar’s Test as a repeated measures version of a chi-square test of independence was then applied to assess the improvement in depression symptoms in terms of partial remission at follow up. The test is suitable for dichotomous variables with two dependent sample studies. All criteria for the use of the McNemar’s Test were met. These include the before-after effect, a 2X2 contingency table with the dichotomous variable at time 1 and time 2 and matched paired studies. General Linear Modelling, in particular two-ways Analysis of Variances (ANOVA) with repeated measures design, were used to assess the treatment outcomes in functional health in depressed and non-depressed patients with regard to Tinetti test assessed at two time points. Furthermore, multiple baseline characteristics, including the indicator of geriatric risk (Lachs), age, gender, living situation and medical support were used to test for intercept effects because each may affect the outcomes for depression and functional health. Multiple Logistic Regressions with intercept terms were used to model the binary response of baseline diseases etiologically linked to major depression with and without adjustment.
Results
Table 1 (Insert Table 1 approximately here.)
Table 1 Clinical and Demographic Characteristics of Selected Patients without Depression admitted to Geriatric Centre and Those Diagnosed with Major Depression
Characteristics | Sample of patients without depression (N=914) | Sample of patients with a diagnosis of major depression (N=902) | P value | Statistical Technique |
| Age (mean, ±SD) | 77.1±8.7 | 79.1±8.1 | .030* | b |
| Gender (Female) (%) | 70.0 | 63.3 | .073 | a |
| Caucasian (%) | 100.0 | 100.0 | .001*** | a |
| Living with partner (%) | 38.9 | 44.7 | .112 | a |
| Living alone (%) | 61.1 | 55.3 | .185 | a |
| Admission Tinetti total (mean, ±SD) | 11.4±8.9 | 7.2±7.1 | .001*** | b |
| Admission BI (mean, ±SD) | 49.3±24.4 | 38.2±22.1 | .001*** | b |
| Lachs screening (mean, ±SD) | 5.5±2.6 | 6.8±2.6 | .001*** | b |
| Mini Mental State Examination (mean, ±SD) | 25.7±3.2 | 23.8±5.6 | .001*** | b |
Type of housing: Private flat (%) | 94.7 | 86.4 | .001** | a |
Type of housing: Nursing home (%) | 5.3 | 13.6 | .001** | a |
| Length of hospitalization, days (mean, ±SD) | 20.4±10.9 | 21.5±10.7 | .050* | b |
Number of medical diagnosis or comorbidity GDS (mean, ±SD) | 8.8±3.5
2.4 | 11.2±6.4
14.2 | .135
.001** | b
b |
Crosstabs Chi-Square Test (χ2) (a); Mann-Whitney U Test (b);
*** P ≤ 0.001 ** P≤ 0.01 * P ≤ 0.05
Tables 1
As noted in Table 1, the sample consisted of Caucasian patients (100%), the majority being female (70% versus 63%) and living alone (61.5% vs. 55.3%), mostly as a result of the partner’s death. The sample exhibited a significant mean level of cognitive impairment (25.7 vs. 23.8) with 52% scoring 25 or less on the MMSE. The total sample (n = 1,816) which is made up of n = 902 patients with major depression (50%) and n = 914 others without depression (50%) is consistent with the recommended methodological concern of sample size equivalence in clinical studies aimed at comparing two clinical groups after treatment. An important level of functional mobility decline was obvious in Tinetti gait and balance (mean = 11.4 vs. 7.2). Patients also exhibited a high level of functional ability decline as measured by the Barthel Index (mean = 49.3 vs. 38.2). Those without depression scored between 0 and 5 on the GDS-15 (2.4 vs. 14.2). Taken together, descriptive results show that functional decline was more accentuated in patients with major depression than in those without depression.
Table 2 (Insert Table 2 approximately here.)
Table 2 Illness Categories and Number (Percentage) of Patients with Major Depression and Comorbid Illnesses (N = 902)
| Illness Categories | N | Frequency |
| Arterial hypertension | 537 | 62.7 % |
| Arrhythmia diagnosis | 259 | 30.2 % |
| Heart or valvular insufficiency | 222 | 25.9 % |
| Stroke | 204 | 23.8 % |
| Focal neurologic deficits | 198 | 23.1 % |
| Cerebral infarct | 176 | 20.5 % |
| Coronary heart disease | 166 | 19.4 % |
| Artificial valvular or pace maker | 154 | 18.0 % |
| Heart operation | 153 | 17.9 % |
| Leg or thorax fracture | 130 | 15.2 % |
| Obesity due to excess calories | 117 | 13.7 % |
| Nutrition disturbance | 95 | 11.1 % |
| Oesophagus and stomach disease | 89 | 10.4 % |
| Pneumonia | 63 | 7.4 % |
| Adiposity fat localised | 58 | 6.8 % |
Chronic arthritis Hypercholesterolaemia Liver disease Tumour in respiratory organ | 58 56 45 30 | 6.4 % 5.5% 5.3% 3.5% |
Table 2 reports the frequency distribution for medical illnesses among the sample of major depression. Arterial hypertension was present in 62.7% of the participants. Arrhythmia diagnosis was present in 30%. Heart or valvular insufficiency, stroke, focal neurologic deficits and cerebral infarct were present in over 20%. Coronary heart disease, artificial valvular or pace maker, heart operation, leg or thorax fracture, obesity, nutrition disturbance, oesophagus or stomach disease were ascribed to more than 10% whereas pneumonia, adiposity, chronic arthritis, hypercholesterolemia and liver disease occurred in more than 5%. Tumour in respiratory organ was found in more than 3%. The occurrence of multiple chronic disorders was also common, with 20% having five illnesses, 25% having eight illnesses and 45% having more than ten illnesses.
Table 3 (Insert Table 3 approximately here.)
Table 3 Illness Categories and Number (Percentage) of Patients without Major Depression and Comorbid Illnesses (N = 912)
| Illness Categories | N | Frequency |
| Arterial hypertension | 515 | 56.3 % |
| Arrhythmia diagnosis | 269 | 29.4 % |
| Heart or valvular insufficiency | 209 | 22.9 % |
| Stroke | 199 | 21.8 % |
| Cerebral infarct | 163 | 17.8 % |
| Focal neurologic deficits | 149 | 16.3 % |
| Artificial valvular or pace maker | 137 | 15.0 % |
| Heart operation | 134 | 14.7 % |
| Coronary heart disease | 128 | 14. % |
| Nutrition disturbance | 123 | 13.5 % |
| Leg or thorax fracture | 121 | 13.2 % |
| Obesity due to excess calories | 108 | 11.8 % |
| Oesophagus and stomach disease | 74 | 8.1 % |
| Pneumonia | 52 | 5.7 % |
| Adiposity fat localised | 52 | 5.7 % |
Liver disease Tumour in respiratory organ Chronic arthritis Hypercholesterolaemia | 30 31 21 20 | 3.5 % 3.4% 2.3% 2.% |
Table 3 reports the frequency distribution for medical illnesses among the sample of patients without major depression. Arterial hypertension was present in 56.3% of the participants. Arrhythmia diagnosis was present in 29.4%. Heart or valvular insufficiency were present in 23%. Stroke was present in 22%. Cerebral infarct was present in 18% and Focal neurologic deficits were present in 17%. Coronary heart disease, artificial valvular or pace maker, heart operation, leg or thorax fracture, obesity, nutrition disturbance ranged between 10% and 18% whereas oesophagus or stomach disease, pneumonia, adiposity, chronic arthritis, hypercholesterolemia and liver disease occurred in more than 5%. Tumour in respiratory organ was found in more than 3%. Like their counterparts with major depression, the occurrence of multiple chronic disorders was also common.
Table 4 (Insert Table 4 approximately here.)
Table 4 Summarizes results from McNemar’s Test using Cross Tabulation Modelling.
Improvement in depression in term of partial remission
| Improvement in Depression Symptom | Depression_T1 by | Depression_T2 | ||
df | Value | P | ||
| Person | 1 | 437.254 | .001 | |
| Continuity | 1 | 634.557 | .001 | |
| Likelihood Ratio | 1 | 805.940 | .001 | |
| Fischer’s Exact Test | .001 | |||
| Linear by linear | 1 | 636.903 | .001 | |
| Asssociation |
| |||
| McNemar’s Test | .001 | |||
| Sample size | 1,816 | |||
Criteria = Alpha (. 05); Significance level: p < .001 **, p < .05 *
(Insert Table 5 approximately here.)
Table 5 (Insert Table 5 approximately here.)
Table 5. Risk Estimate Table
| Odds Ratio | Value | 95% Confidence Interval | |
| Lower Upper | |||
For major depression T1 no depression/depression | 498.320 | 123.678 2007. 817 | |
For cohort major depression T2 = no depression | 2.088 | 1.950 2.236
| |
For cohort major depression T2 = depression | .004 | .001 .017 | |
| N of Valid Cases | 1816 | ||
Improvement in depression symptoms i.e., partial remission
The results (Table 4, 5) strongly demonstrate an improvement in depression symptoms at T2, McNemar’s Test [(p < .001); Person (χ2 = 437.254); Odds ratio= 2.08; 95% confidence interval (CI) = 1.95 - 2.23]; the relationship is strong between the variables. We can report the result as showing statistically significant improvement in depression symptoms due to treatment effect at follow- up assessment. In fact, the results point to a significant improvement in depression in terms of partial remission at the second time point assessment.
All results yielded a significant and strong power effect that accounts for 47% improvement or partial remission at follow-up. 53% remained depressive at T2. All remitters scored below 5 points on the GDS-15 i.e., between 0 and 5 on the GDS-15. Some residual symptoms of depression were still present but most key symptoms of major depression were no longer reported and an improvement in functional mobility was noticeable.
Table 6 (Insert Table 6 approximately here.)
Table 6 Results from ANOVA, Tinetti score (Within-Subjects Effects)
| Source | Type III sum of Squares | df | Mean Square | F | P | Partial Eta Squared | Observed Power |
| Time | 5362.044 | 1 | 5362.044 | 382.544 | .000 | .265 | 1.000 |
| Time X Dep. T1 | 18.510 | 1 | 18.510 | 1.321 | .251 | .001 | .209 |
| Time X lachsT1 | 7.378 | 1 | 7.378 | .526 | .468 | .001 | .112 |
| Error (Time) | 14885.857 | 1062 | 14.017 |
ANOVA with follow-up design; Criteria = Alpha (. 05); Significance level: p < .001 **,
p < .05 *; ηp2 (Partial Eta Squared)
Table 7 (Insert Table 7 approximately here.)
Table 7 Results from ANOVA, Tinetti score (Between-Subjects Effects)
| Source | Type III Sum of Squares | df | Mean Square | F | P | Partial Eta Squared | Observed Power |
| Intercept | 154903.369 | 1 | 154903.369 | 1328.098 | .000 | .556 | 1.000 |
| Dep. T1 | 4837.843 | 1 | 4837.843 | 41.478 | .000 | .038 | 1.000 |
| Lachs_T1 | 5268.703 | 1 | 5268.703 | 45.172 | .000 | .041 | 1.000 |
| Error | 123866.912 | 1062 | 116.636 |
ANOVA with follow-up design; Criteria = Alpha (. 05); Significance level: p < .001 **,
p < .05 *
Insert Graphic 1 (approximately here.)
Graphic 1. Improvement in functional mobility (Tinetti gait and balance) in depressed patients versus those with no depression at follow-up
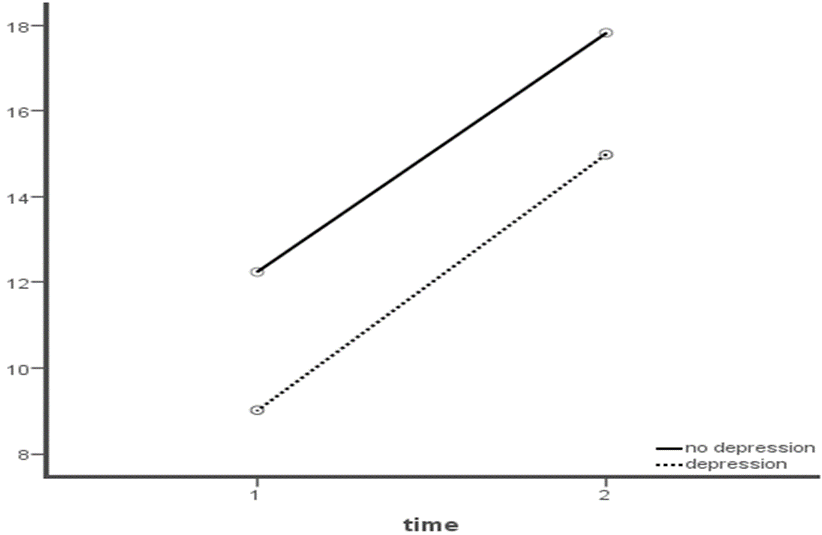
Interpretation of ANOVA with Repeated Measures Analysis
Regarding Tinetti gait and balance (Table 6, 7) an analysis was run to test whether the rehabilitation program drove a change of the measurement level over time.
Non-dep: x̅tinT1 = 12.43; x̅tinT2 = 18.03; Dep: x̅tinT1 = 8.83; x̅tinT2 = 14.08
x̅TotaltinT1 = 10.62; x̅TotaltinT2 = 16.39; df = 1. 1062; F = 382.544
x̅Total_diff = 3.04; p < .001); CI (2.11-3.96); Mean Square = 5362.044; F = 382.544; p < .001; ηp2 = .26; Observed Power = 1; yielded a highly significant within-group change in both groups. There is a genuine main time effect in terms of within-patient change in Tinetti gait and balance mean (Table 6) in both groups. The results corroborate the hypothesis that both groups of patients benefit from the acute rehabilitation. However, there is no significant difference in the increase of functional mobility (Tinetti test) over time between the two groups (non-depressed vs. depressed patients) as noticeable in Table 6: Mean Square = 18.510; F = 1.321; p < .251; ηp2 = .001; Observed Power = .209. The within-group treatment mean of non-depressed patients is not higher than those with depression at follow-up. The artefact we dealt with here originated from the clinical data. The two groups already significantly differed on the Tinetti at baseline (non-dep tinT1 12.43 vs. dep tinT1 8.83). The non-depressed group has an increase on Tinetti of 5.6 points and the depressed group of 5.25 points. The hypothesis that the treatment mean of non-depressed patients at follow-up will be higher than those with depression at baseline is not confirmed.
Table 8 (Insert Table 8 approximately here.)
Table 8 Logistic Regression for Effect of Illness Category on Depression |
| ||||
Without adjustment for baseline disability (before treatment)a | With adjustment for follow-up disability (in partial remission)b | ||||
Sig.(P) | Odds Ratio (95.0 % CI) | Sig.(P) | Odds Ratio (95.0 % CI) |
| |
| Focal neurologic deficits | 0.003 | 1.45 (1.13 - 1.86) | 0.007 | 1.60 (1.14 - 2.26) |
|
| Cerebral infarct | 0.500 | 1.09 (0.84 - 1.42) | 0.558 | 1.12 (0.76 - 1.64) |
|
| Coronary heart disease | 0.032 | 1.34 (1.02 - 1.75) | 0.001 | 2.00 (1.37 - 2.33) |
|
| Heart operation | 0.618 | 1.39 (0.37 - 5.16) | 0.089 | 1.14 (0.01 - 1.34) |
|
| Leg or thorax fracture | 0.321 | 1.14 (0.87 - 1.50) | 0.320 | 0.81 (0.55 - 1.21) |
|
| Acute myocarditis infarct | 0.785 | 0.95 (0.65 - 1.37) | 0.963 | 1.01 (0.59 - 1.71) |
|
| Heart or valvular insufficiency | 0.883 | 1.01 (0.80 - 1.28) | 0.001 | 1.77 (1.27 - 2.48) |
|
| Artificial valvular or pace maker | 0.687 | 0.76 (0.20 - 2.81) | 0.033 | 11.27 (1.22 - 104.10) |
|
| Tumour diagnosis in respiratory organ | 0.728 | 1.09 (0.65 - 1.84) | 0.011 | 2.73 (1.25 - 5.95) |
|
| Liver disease | 0.424 | 0.79 (0.45 - 1.35) | 0.171 | 1.86 (0.76 - 4.55) |
|
| Oesophagus and stomach disease | 0.287 | 1.20 (0.85 - 1.69) | 0.737 | 1.08 (0.67 - 1.75) |
|
| Obesity due to excess calories | 0.047 | 0.57 (0.33 - 0.99) | 0.478 | 1.38 (0.56 - 3.40) |
|
| Arterial hypertension | 0.971 | 0.99 (0.81 - 1.21) | 0.579 | 1.08 (0.80 - 1.46) |
|
| Obesity due to excess calories by arterial hypertension | 0.004 | 2.54 (1.34 - 4.83) | 0.731 | 0.83 (0.30 - 2.30) |
|
|
|
| |||
- Intercept and independent main effect of each coexistent illness on Major depression without adjustment
Omnibus Tests of Model Coefficients
χ2= 30.355; df = 15; p < .01
Model Summary:
-2Log likelihood = 2487.077
Goodness of fit:
Hosmer and Lemeshow Test: χ2= 4.550; df = 8; p = .804
1. Intercept and independent main effect of each coexistent illness on Major depression after adjustment
Omnibus Tests of Model Coefficients
χ2= 69.579; df = 15; p < .001
Model Summary:
-2Log likelihood = 1181.679
Goodness of fit:
Hosmer and Lemeshow Test: χ2= 6.760; df = 8; p = .563
Interpretation of the results
Main effect before adjustment
The results (Table 8) demonstrate that before adjustment coronary heart disease [exponential ß = 1.34; 95% confidence interval (CI) = 1.02 - 1.75; p < .001]; focal neurologic deficits [exponential ß = 1.45; 95% confidence interval (CI) = 1.13 - 1.86; p < .003], are each independently highly predictive for depression. Interpretation of the regression coefficient exponential (ß) suggests that the presence of coronary heart disease contributes to a 1.34 times higher risk for depression compared to patients without coronary heart disease. The presence of focal neuropsychological diseases leads to an increase in risk for depression (odds ratio) by 1.45.
Intercept effects before adjustment
Table 5 shows that some comorbid medical conditions are independently linked to depression risk before adjustment. In referring to intercept models, the logic behind this is to test for a possible moderator or co-factors path.
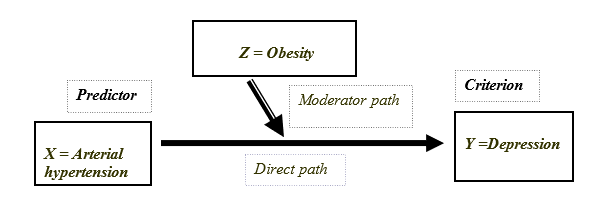
The results demonstrate that the interaction terms between arterial hypertension and obesity [exponential ß = 2.54; confidence interval (CI) = 1.134 – 4.83; p < .004] is (in this sample) jointly highly predictive for depression risk. There is a moderator effect between arterial hypertension, obesity and depression before treatment. Interpretation of the regression coefficient exponential (ß) suggests that the concomitant presence of arterial hypertension and obesity contribute to a 2.54-time higher risk for depression compared to patients without this interaction effect. While the interaction effect between arterial hypertension and obesity is significantly predictive of depression risk, the independent effect of each single predictor on depression does not have a risk effect [(arterial hypertension, Sig = .097; Expo ß = .099 CI= .81-1.21); (obesity, Sig = .047; Expo ß = .57; CI = .033-.99)]. It demonstrates that arterial hypertension in association with obesity predict depression risk better than arterial hypertension by itself. Obesity diagnosis does mediate the effect of arterial hypertension on depression. The results strengthen the hypothesis of a moderator effect. The combination of the two predictors is predictive of depression risk, and the model is efficient, statistically significant: goodness of fit = .563; χ2= 6,750; df = 8; p < .001; -2Log likelihood= 1181.679.
Main effect after adjustment
The results (Table 8) strongly demonstrate that after adjustment coronary heart disease [exponential ß = 2.00; 95% confidence interval (CI) = 1.37 - 2.33; p < .00]; focal neurologic deficits [exponential ß = 1.60; 95 % confidence interval (CI) = 1.14 - 2.26; p < .007]; heart or valvular insufficiency [exponential ß = 1.77; 95% confidence interval (CI) = 1.27 - 2.48; p < .001]; artificial valvular or pace maker [exponential ß = 11.27; 95% confidence interval (CI) = 1.22 - 104.10; p < .03]; tumour diagnosis in respiratory organ [exponential ß = 2.73; 95% confidence interval (CI) = 1.25 - 5.95; p < .01], are each independently highly predictive for depression recurrence or relapse. Interpretation of the regression coefficient exponential (ß) suggests that the presence of coronary heart disease contributes to a 1.37 times higher risk for depression recurrence compared to patients without coronary heart disease in partial remission. The presence of focal neurologic deficits leads to an increase in risk for depression (odds ratio) by 1.60. After treatment some new patterns of chronic condition (mainly heart or valvular insufficiency, artificial valvular or pace maker and tumour diagnosis in respiratory organs) were each independently predictive for depression occurrence. The intercept terms between arterial hypertension and obesity were no longer significant after adjustment [exponential ß = 0.83; 95% confidence interval (CI) = 0.30 - 2.30; p < .73].
The results support the conjecture that whereas some chronic conditions would act independently as a trigger for depression, some other would need a moderator factor (co-factor path) to trigger depression occurrence before and after adjustment.
Discussion
This study was designed to examine the specific effect of baseline comorbid diseases on major depression before and after adjustment for baseline disability. It also aimed at assessing the differential functional health outcome following acute medical rehabilitation in patients with a diagnosis of major depression versus no depression. We found that 431 patients (47%) were in partial remission at follow-up. The results which are convergent with those from [9, 39] show that that functional deficit was more accentuated in patients with major depression than in those without depression. Key results point to an improvement at follow-up in functional mobility in both non-depressed and depressed patients as an effect of the intensive rehabilitation. However, at follow-up assessment, the performance of non-depressed patients is not significantly higher than those with major depression at baseline. The plausible hampering effect of baseline depression on functional rehabilitation outcomes outlined by [19, 29, 39] was not supported by our results. We dealt with an endogenous artefact originating from the clinical data we relied on. Our study shows that like their counterparts without depression, patients with depression at admission benefited from the intensive rehabilitation in term of an increase in functional mobility as measured by the Tinetti at follow-up. This may be due to an effect of the multidisciplinary treatment which included simultaneous antidepressant and psychotherapy management.
Consistent results demonstrate that there is a synergetic relationship between certain illnesses and major depression. The results shed light on the conjecture that there is a connection between specific pattern of chronic comorbid diseases and major depression before medical treatment on the one hand, and after acute rehabilitation and partial remission on the other hand. This pathway (focal neurologic deficits, coronary artery disease) that brings on a potential risk factor for depression before medical treatment sustains after treatment and may act as a risk factor for occurrence of depression after acute rehabilitation, antidepressant and psychotherapeutic treatment. A cofactor effect between arterial hypertension and obesity has been unveiled with the capacity to set off depression before adjustment. Results disclosed a new pattern of chronic conditions mainly for valvular insufficiency, artificial valvular or pace maker and tumour diagnosis in respiratory organs that emerge independently as a risk factor for depression after adjustment. The intercept terms between arterial hypertension and obesity that act as risk factors for depression before adjustment were no longer significant after treatment. This may be due to a proper management of arterial hypertension and weight through adherence to a balanced diet during the course of hospitalization. Thus, although hypertension is very common in geriatric patients and may lead to disability, it may not be associated with depression if well managed [33, 27].
The findings of this study show that elderly patients with coronary heart disease, focal neurologic deficits, arterial hypertension and obesity with comorbid major depression have a higher odd for depression worsening. Nevertheless, they have an amelioration in functional health following the acute treatment. In contrast, other studies found that multimorbid geriatric patients have a poorer rehabilitation outcome probably as a result of worse reaction to medical treatment [16, 35]. Previous findings highlighting the moderator effect of disability suggest that chronic illnesses that lead to functional decline or disability are the most likely illnesses to negatively affect the treatment of depression [9]. Specifically, chronic diseases such as focal neurologic deficits, coronary heart diseases, heart or valvular insufficiency and tumour in respiratory organs that trigger depression are those linked to a high potential risk of fall, negative interference with pharmacotherapy and are associated with worse symptoms that weaken functional mobility [31, 33, 35]. Moreover, those illnesses that do not lead to significant functional limitation or those that are more effectively treated or managed may not be associated with treatment non-response. As suggested by the vascular depression hypothesis, the reduction in response to typical treatment may also reflect the need for intervention. Such intervention should also focus on the decline in functional mobility. For instance, combined healthy exercise and physiological therapy or enhanced psychopharmacological treatment of pain [30]. Of the effects noted before and after adjustment, coronary heart disease, focal neuropsychological diseases and the cofactor effects between arterial hypertension and obesity as well as valvular insufficiency, artificial valvular or pace maker and tumour diagnosis in respiratory organ are the most consistent findings. At first glance, one could hypothesize that this interaction is mediated through functional ability and mobility deficits. Moreover, with an increasing support for self-regulation’s positive effect on health, it becomes plausible that this interaction may be mediated through cognitive resources such as mood state, self-efficacy, implementation of healthy exercise and maintenance of autonomy.
These results strengthen the vascular depression hypothesis. Indeed, coronary artery disease, focal neuropsychological diseases and tumour diagnosis in respiratory organs are among those illnesses which have been associated with worse treatment outcomes in major depression [31, 24], and appear to be strongly bound [32] to the pathogenesis of neurodegeneration and neurotransmitter disturbance in the ageing brain. In fact, the vascular depression hypothesis is supported by the high rate of depression in patients with hypertension, frontal lobe disease, diabetes and coronary heart disease [3, 8]. Patients who suffered from a stroke are also concerned [21, 37]. Consecutive to the combined rehabilitation, antidepressant and psychotherapy treatment, 53% of depressed patients at baseline did not improve at follow-up. Considering the number of geriatric patients with a diagnosis of major depression at baseline and their counterpart without depression that allowed the follow-up design, it is possible that this fact unveils a lack of treatment response [25, 10, 24, 41]. This finding is in phase with other reports in the literature [11, 17, 35]. Previous research which supports this assumption has found significant associations between increasing severity of decline in executive functions, certainly related to frontal lobe damage, with greater functional limitation and need for more health services [23]. Cytokine production (a non-antibody protein) is suspected to influence response rates in major depression [41, 26]. Research which consolidates this assumption highlighted chronic, non-infectious diseases (coronary artery disease, pulmonary disease) linked to increased levels of cytokines [14, 6]. However, this assumption is controversial. The results of this study have two major public health implications: According to the World Health Organization, the burden of depression and functional deficit is likely to be serious in the next decade. The public health implication of these estimates is further magnified when put in the context of available evidence that functional decline predicts further functional limitation, functional dependence, increased health care costs, and increased risk of death.
Limitations
We relied on data from clinical scenarios to test the suspected hampering effect of major depression on functional rehabilitation outcome in elderly undergoing geriatric rehabilitation.
Based on our data, the results did not support the conjecture that the treatment mean of non-depressed patients at follow-up will be higher than those with depression at baseline. An artefact endogenous to the clinical data, which we relied on, caused this. Indeed, the two groups were already different at baseline. Further clinical investigations should control this bias through an innovative experimental design. Whereas the treatment of somatic diseases and functional health were the treatment goals in both groups, a partial remission in depression symptoms was an additional goal for those with major depression. A longitudinal design could have helped to better assess how the improvement in functional mobility and depression evolved. Finally, although patients who were diagnosed with major depression received a proper treatment, we do not know whether this combined treatment was sustained in an ambulatory setting after discharge from hospital.
Conclusion
Before treatment, specific somatic diseases emerge through an independent and moderator path as risk factors for depression. Except for the intercept effects, this influence persists even after treatment. The results of this paper support the assumption that chronic diseases, as well as depression and functional decline are interconnected. The findings suggest that an accurate medical treatment aimed at enhancing functional health should tackle depression and chronic diseases.
The study considered all-important recommendations of the Helsinski Declaration of 1975 (in its most recently amended version) as well as the guidelines issued by the ethical standards of the ethics committee of the Charité Universitätsmedizin Berlin. Informed consent was obtained from all participants included in the study.
Acknowledgements
I would like to thank the following individuals for their expertise and assistance throughout all aspects of the study and for their help in writing the manuscript.
First and foremost, I would like to thank my supervisor, Professor Dr. Elisabeth Steinhagen-Thiessen for her invaluable guidance and support throughout the research process.
I would like to express my deepest gratitude to Professor Dr. Wolfgang Jost who provided expertise that greatly assisted the research and enabled the publication.
I am deeply indebted to Dr. Gernot Fischer and Dr. Rolf Nieczaj who moderated this paper and, in that line, improved the manuscript significantly.
I am extremely grateful to Wolfgang Reiner, Murat Karaman and David Emmans.
Words cannot express my gratitude to Dr. Aristide Traoré, IRSS/CNRST.
References
- Alexopoulos GS (2003) Role of executive function in late-fife depression. J Clin Psychiatry 64 (14):18–23
- Bekhuis E, Boschloo L, Rosmalen JG (2016) Impact of somatic symptoms on the course of major depressive disorder. Journal of Affective Disorders 205:112–118
- Carney RM, Rich WM, Tevelde A, Saini J, Clark K, Jaffe AS (1987) Major depressive disorder in coronary artery disease. Am J Cardiol 60:1273–1275
- Charlson M, Peterson JC (2002) Medical comorbidity and late life depression: What is known and what are the unmet needs? Soc Biol Psychiatry 52: 226–235
- Charlson M, Szatrowski TP, Peterson J, Gold J (1994) Validation of a combined comorbidity index. J Clin Epidemiol 47(11):1245–51
- Cottone S, Mule G, Amato F, Riccobene R, Vadalà A, Lorito MC, Raspanti F, Cerasola G (2002) Amplified biochemical activation of endothelial function in hypertension associated with moderate to severe renal failure. J Nephrol 15:643–648
- D’Ath P, Katona P, Mullan E (1994) Screening, detection and management of depression in elderly primary care attenders: The acceptability and performance of the 15 items Geriatric Depression Scale (GDS15) and the development of short version. J Fam Prac 11: 260–266
- Disabato BM, Sheline YI (2012) Biological basis of late life depression. Curr Psychiatry Rep 14:273–9
- Egede LE (2004) Diabetes, major depression, and functional disability among U.S. adults. Diabetes Care 27:421–428
- Euba R, Panihhidina I, Zamar A (2015) Treatment-resistant depression: the experience of the first rTMS Clinic in the UK. Future Neurology 10(3):211–-215
- Fakhoury M (2016) Revisiting the serotonin hypothesis: implications for major depressive disorders. Mol Neurobiol. 53(5):2778–2786
- Greden J, Riba M, McInnis M (2011) Treatment resistant depression: A roadmap for effective care. Arlington VA: American Psychiatric Publishing
- Groll DL, To T, Bombardier C, Wright JG (2005) The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol 58(6):595–602
- Hannestad J, DellaGioia N, Bloch M (2011) The effect of antidepressant medication treatment on serum levels of inflammatory cytokines: A meta-analysis. Neuropsychopharmacology 36:2452–2459
- Hegeman JM, Fenema EM, Comijs HC (2017) Effect of chronic somatic diseases on the course of late-life depression. International Journal of Geriatric Psychiatry 32(7):779–787
- Hybels CF, Pieper CF, Blazer D G (2009) The complex relationship between depressive symptoms and functional limitations in community dwelling older adults: The impact of subthreshold depression. Psychol Med 39(10):1677–1688
- Iosifescu DV, Nierenberg AA, Alpert JE, Smith M, Bitran S, Dording C, Fava M (2003) The impact of medical comorbidity on acute treatment in major depressive disorder. Am J Psychiatry 160:2122–2127
- Lachs MS, Feinstein AR, Cooney LM, Drickamer MA, Marottoli RA, Pannill FC, Tinetti ME (1990) A simple procedure for general screening for functional disability in elderly patients. An Intern Med 112:699–706
- Lêng CH, Wang JD (2013) Long-term determinants of functional decline of mobility: An 11-year follow-up of 5464 adults of late middle aged and elderly. Arch Gerontol Geriatr. 57(2):215–20
- Lin SI, Lee H C, Chang K C, Yang YC, Tsauo JY (2017) Functional mobility and its contributing factors for older adults in different cities in Taiwan. Journal of the Formosan Medical Association. 116:72–79
- Lipsey JR, Spencer WC, Rabins PV, Robinson RG (1986) Phenomenological comparison of poststroke depression and functional depression. Am J Psychiatry 143: 527–529
- Oslin DW, Datto CJ, Kallan MJ, Katz IR, Edell WS, TenHave T (2002) Association between medical comorbidity and treatment outcomes in late-life depression. J Am Geriatr Soc 50:823–828
- Papakostas GI, Fava M (2010) Pharmacotherapy for depression and treatment-resistant depression. Hackensack NJ: World Scientific
- Preston JD, O’Neal JH, Talaga MC (2013) Handbook of Clinical Psychopharmacology for Therapists. 7th ed. New Harbinger Publications Inc: Oakland
- Robinson RG, Kubo KL, Starr LB, Rao K, Price TR (1984) Mood disorders in stroke patients: importance of location of lesion. Brain 107:81–93
- Royall DR, Chiodo LK, Polk MJ (2000) Correlates of disability among elderly retirees with subclinical cognitive impairment. J Gerontol Biol Sci Med Sc 55A:541–546
- Rubio-Guerra AF, Rodriguez-Lopez L, Vargas-Ayala G, Huerta-Ramirez S, Serna DC, Lozano-Nuevo JJ (2013) Depression increases the risk for uncontrolled hypertension. Exp Clin Cardiol 18(1):10–12
- Ryan A, Wallace E, O’Hara P, Smith SM (2015) Multimorbidity and functional decline in community-dwelling adults: A systematic review. Health and Quality of Life Outcomes13:168
- Sin NL, Yaffe K, Whooley MA (2015) Depressive symptoms, cardiac disease severity, and functional status among older patients with coronary heart disease: The heart and soul study. J Am Geriatr Soc. 63(1):8–15
- Stephen PR, Marissa M (2005) Pharmacologic treatment of depression in patients with heart disease. Psychosom Med 67:54–57
- Taylor WD, Aizenstein HJ, Alexopoulos GS (2013) The vascular depression hypothesis: Mechanisms linking vascular disease with depression. Mol Psychiatry 18:963–74
- Taylor WD, Steffens ME, Payne ME, MacFall JR, Marchuk DA, Svenson IK, Krishnan KR (2005) Influence of serotonin transporters region polymorphisms on hippocampal volumes in late-life depression. Arch Gen Psychiatry 62(5):537–544
- Thomas P, Hazif-Thomas C, Billon R, Peix R, Faugeron P, Clément JP (2009) Depression and frontal dysfunction: Risks for the elderly? Encephale 35(4):361–9
- Tinetti ME (1986) Performance oriented assessment of mobility problems in elderly patients. J Am Geriatr Soc 34:119–126
- Trivedi MH (2006) Major depressive disorder: Remission and associated symptoms. J Clin Psychiatry 67(6):27–32
- Trivedi RB, Nieuwsma JA, Williams JW (2011) Examination of the utility of psychotherapy for patients with treatment resistant depression: A systematic review. Journal of General Internal Medicine 26(6):643–650
- Valkanova V, Ebmeier KP (2013) Vascular risk factors and depression in later life: A systematic review and meta-analysis. Biol Psychiatry 73(5):406–13
- Walter M, Anton L (2015) How can we predict treatment outcome for depression? E BioMedicine 2: 9–10
- Wilcox ME, Freiheit EA, Faris P, Hogan DB, Patten SB, Anderson T, Ghali WA, Knudtson M, Demchuk A, Maxwell CJ (2016) Depressive symptoms and functional decline following coronary interventions in older patients with coronary artery diseases: A prospective cohort study. BMC Psychiatry 16:277
- World Health Organization (2004) ICD-10: Chapter V. Mental and behavioural disorders. Diagnostic criteria for research. Tenth revision of the international classification of diseases. WHO: Geneva
- Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, Leirer VO (1983) Development and validation of geriatric depression scale: a preliminary report. J Psychiatr R


