Case Report | DOI: https://doi.org/10.58489/2836-497X/009
Micro-invasive Primary Squamous Cell Carcinoma of Endometrium: Case Report, 2023
1 MD, Obstetrics and Gynecology, Orotta College of Medicine and Health Science, Post-graduate, Ministry of Health, Asmara, Eritrea
2 MD, Obstetrician and Gynecologist, Associate professor, Orotta college of Medicine and Health science, Post-graduate, Ministry of Health, Asmara, Eritrea
3 MD, Dekemhare Hospital, Zoba Debub, Ministry of Health, Eritrea
4 MD, Pathologist,Orotta College of Medicine and Health Science, Post-graduate, Ministry of Health, Asmara, Eritrea
*Corresponding Author: Berhe Tesfai*
Citation: Berhe Tesfai, (2023). Micro-invasive Primary Squamous Cell Carcinoma of Endometrium: Case Report, 2023. Archives of Gynaecology and Women Health.2(1). DOI: 10.58489/2836-497X/009
Copyright: © 2023 Berhe Tesfai, this is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 27 February 2023 | Accepted: 15 March 2023 | Published: 20 March 2023
Keywords: Primary squamous cell carcinoma; Endometrium; Postmenopausal; Eritrea
Abstract
Primary endometrial squamous cell carcinoma is an extremely rare tumor which is usually seen in postmenopausal women with unclear pathogenesis. We report a case of postmenopausal woman with primary endometrial squamous cell carcinoma.
Introduction
Pure primary endometrial squamous cell carcinomas (PESCC) are extremely rare, accounting for 1% of all malignancies of the corpus uteri with only 100 cases being reported in the literature, since the first report in 1892 by Gebhard [1,2]. It is usually seen in postmenopausal women and associated with cervical stenosis, pyometra, chronic inflammation, nulliparity and icthyosis uteri. [2] In view of the fact little is known about Its genesis, histogenesis, and biological behavior [1, 3] The diagnostic criteria for PSCC of the endometrium include the absence of the following: [1] coexisting endometrial adenocarcinoma; [2] a connection between squamous cell carcinoma (SCC) of the endometrium and the squamous epithelium of the cervix; and [3] a primary squamous lesion in the cervix, either in situ SCC or an invasive carcinoma. [2, 3]. We report case of Primary Squamous Cell Carcinoma of the Endometrium in which final histopathology diagnosis in the hysterectomy specimen confirmed this rare tumor.
Case report
This is 73 years old post-menopausal woman come to Orotta National Maternity Hospital on 7th Oct, 2022 with complaint of lower abdominal pain and down pushing sensation of six months’ duration. She also experienced back pain, and profound weight loss which she couldn’t quantify but no vaginal bleeding. She is Para nine whose menstrual cycle ended before 30 years. She denies any history of using contraceptives or taking drug for longer periods. Two days before her arrival to the hospital she also witnessed bloody urine accompanied with urgency and frequency. She is known hypertensive with poor adherence to treatment but she was not diabetic or had no other chronic illness.
Clinical examination revealed her general condition was good with blood pressure of 160/60 mmHg in left arm in sitting position, an axillary temperature of 36.2 °C, her pulse was 78 beats/min and respiratory rate of 14 breaths/min. Upon inspection, her conjunctiva was pink and chest was clear to auscultation. Abdomen was soft with mild tenderness in suprapubic area and uterus was palpated at 14 weeks’ size which was immobile and attached to deep structures but no to the skin. Speculum examination showed a macroscopically healthy external cervix with protruding mass through internal OS.
Investigations showed white blood count 4.56 ×103/μL, hemoglobin 12.98g/dl, and platelets of 834×103/μL. The serum level of cancer antigen 125 (CA125) was 91.28 U/mL (normal range: 0–34 U/mL), the carcinoembryonic antigen (CEA) was 34.87 ng/mL (normal range: 0–2.5 ng/mL) and the other serum tumor markers alpha-fetoprotein (AFP) and CA19-9 were within normal range. Abdominal ultrasonography showed enlarged uterine size of 5.9cm×5.9cm×7cm, with well-defined hypo-echoic intramural lesion 2.9cm ×3cm×3.2cm and small ovarian cyst with 4mm thickness of endometrium.
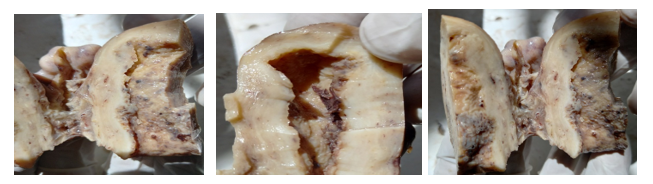
Under general anesthesia, laparotomy was performed and an enlarged uterus fixed to sounding structures was identified. Around 200ml foul smelling pus was evacuated and the posterior lower uterine segment was found fixed to rectum with extensive adhesion. Sub-total hysterectomy with bilateral salpingo-oophorectomy was performed and samples from the posterior uterine wall adherent to rectum was sent for analysis and showed an inflammatory process with no sign of malignant cells. Sample of the removed uterus and adnexa was sent for Pathological examination and discussion with the pathologist was made to take complete circular blocks of the lower uterine segment to rule out direct extension from the cervix. Punch biopsy was taken from three sites which showed only mild signs chronic inflammation. Final pathological analysis of the samples showed features of PSCCE. Total extra fascial hysterectomy with bilateral salpingo oophorectomy and pelvic with para-aortic lymph node dissection has to be done for complete staging. In our case there no lymphadenopathy and extensive adhesions hiders complete staging. Patient was attached to radio-chemotherapy for continuation of treatment. The histopathologic description of the uterus is presented below. (Figure: 1)
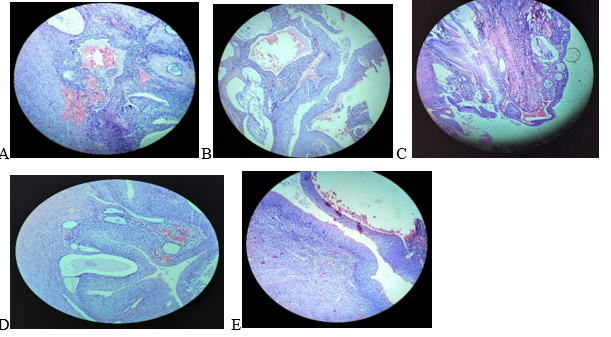
Microscopic description: Sections from the endometrium show polypoid lesions lined by squamoid cells with nuclear atypia and high mitotic activities, micro invasive seen main focally. Features are consistent with micro invasive squamous cell carcinoma of endometrium. (Figure 2)
Discussion
Primary endometrial SCC is a rare entity, most of endometrial cancer are adenocarcinomatous, and most of the endometrial squamous carcinomas originate from the SCC of the cervix or endometrial stem cell, and squamous metaplasia of the normal endometrium. Our case of primary squamous cell carcinoma of the endometrium, final diagnosis was based on histopathology of the hysterectomy specimen, and punch biopsy of the cervix. As the cervix is left behind circularly the isthmus of the uterus is analyzed in which the squamous lesion has no extension crossing towards the uterus, Immunocytological characteristics in specimens was not analyzed because it is not available in our setting. In recourse limited areas preoperative diagnosis of PESCC is more challenging because of its vague clinical presentation and unknown pathogenesis. In our case the patient beside her age has no an identifiable risk in which she is not obese or using any estrogen containing drugs. Currently causes and pathogenic mechanisms responsible for PSCCE is not well studied. Accurate revision of the literature revealed that diverse and controversial hypotheses were suggested by some researchers. [1]
Her clinical presentation was also atypical in which she denies any history of vaginal bleeding or discharge. Speculum exam showed a small mas protruding through the internal cervical canal without active bleeding. The preoperative diagnosis of PESCC in our case was challenging because of the speculum finding of cervical appearance, the sonographic finding of small ovarian cyst, elevated level of serum CA-125, suggested more for ovarian or endometrial cancer. Though cervical smear status has been reported to be abnormal in only about half of cases, and many patients have undergone multiple gynecologic examinations and curettage prior to surgery, [4]
Intraoperatively, there was extensive adhesion to the rectum and the abscess was higher up from the cervix with in posterior wall which could indicate that PESCC had direct invasion rather than hematogenous or lymphatic spread. However, the pathogenesis and etiology of PSCCE are poorly investigated and incompletely understood. The factors predisposing to the development of PSCCE included pyometra, pelvic radiation, estrogen deficiency, and estrogen excess. [1] Our patient had pus collection which might predispose her to PSCCE which is supported by many literatures.
The common treatment methods include surgical hysterectomy with adnexactomy and radiotherapy. However, this type of endometrial cancer has a high degree of malignancy and poor prognosis, and the 5-year survival rate was very low except for individual cases. [5] After hysterectomy patient was attached to oncology unit to go abroad as radiotherapy is not available in our country, and patients who require radiotherapy are often sent to neighboring countries.
Conclusion
Micro-invasive primary squamous cell carcinoma of endometrium is asymptomatic, rare which needs early diagnosis and early treatment due to its poor prognosis. Diagnosis is based on pathological careful examination hysterectomy specimen, Pathogenesis of micro-invasive primary squamous cell carcinoma of endometrium and its association with risk factors was not yet determined. Due to the limited numbers of cases, it is difficult to draw protocol regarding its management. Community awareness is vital for early diagnosis and management of disease and initiation of radiotherapy treatment in our country is crucial for continuation of treatment.
Declarations
Acknowledgments: Author’s acknowledges the maternity staff on management of the patient during and after delivery
Funding: there was no any source of fund for this case report
Informed consent: Written informed consent was obtained from the patient to participate in the case report
Competing of interest: authors declare that there was no any conflict of interest to disclose
Authors contribution: all authors had contributed on data analysis and writing
References
- Fatima Zahra Farhane, Zineb Alami, Touria Bouhafa, Abderrahmane Elmazghi, Khalid Hassouni. (2018) Primary squamous cell carcinoma of endometrium: case report and literature review, Pan Afr Med J. ; 30: 8
View at Publisher | View at Google Scholar - Kafil Akhtar, Binjul Juneja, Ghazala Mehdi, Seema Rashid (2018) Primary squamous cell carcinoma of endometrium-a rare presentation. Obstetrics & Gynecology International Journal, November 30,
View at Publisher | View at Google Scholar - Tchin Darré, Abdoul-Samadou Aboubakari, Lantam Sonhaye, Baguilane Douaguibe, Akila Bassowa & Gado Napo-Koura. (2019) Primary squamous cell carcinoma of the endometrium associated with human papilloma virus in a young woman: a case report. Journal of medical case reports, Article number: 167
View at Publisher | View at Google Scholar - Hongyi Li, Jiatian Ye, Xiaorong Qi, Xi Wang. (2022) Primary endometrial squamous cell carcinoma with endometrial atypical hyperplasia in elderly women: a case report. GPM, Vol 5 September 25,
View at Publisher | View at Google Scholar - Chao Zhang, Hongyan Zhang, Linqing Yang, Yunfei Wang, Xiaoyu Li, Jinfeng Guo, Jing Xu, (2018) Primary squamous cell carcinoma of the endometrium in a woman of perimenopausal age. NIH, Nov 30
View at Publisher | View at Google Scholar - Giovanna Giordano, Tiziana D'Adda, Carla Merisio, Letizia Gnett. (2005) Primary squamous cell carcinoma of the endometrium: case report with immunohistochemical and molecular study. Volume 96, issue 3,
View at Publisher | View at Google Scholar - Sanda Rajhvajn. Primary squamous cell carcinoma of the endometrium—Case report with cytological characteristics in direct and indirect endometrial samples. Cytopathology Volume 32, Issue 6 p. 823-826
View at Publisher | View at Google Scholar