Current Issue : Article / Volume 3, Issue 1
- Case Report | DOI:
- https://doi.org/10.58489/2836-5062/017
Neuroendocrine Carcinoma of the Breast: Literature Review and Case Analysis
1Clinical Oncology Service, Hospital de ClÃnicas, Faculty of Medicine, University of the Republic, Uruguay.
Natalia Camejo*
Clara Tambasco, Natalia Camejo, Cecilia Castillo, Gabriel Krygier. (2024). Neuroendocrine Carcinoma of the Breast: Literature Review and Case Analysis. Journal of Clinical Oncology Reports. 3(1); DOI: 10.58489/2836-5062/017
© 2024 Natalia Camejo, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 23-07-2024
- Accepted Date: 27-07-2024
- Published Date: 29-07-2024
Neuroendocrine carcinoma of the breast, neuroendocrine tumors, chemotherapy, differential diagnosis, immunohistochemistry.
Abstract
Introduction: Neuroendocrine tumors are rare neoplasms that can occur in various organs, being most common in the gastroenteropancreatic tract and lungs. Neuroendocrine carcinoma of the breast (NECB) is a rare and heterogeneous subtype, lacking standardized therapeutic guidelines and protocols, with limited prospective clinical studies. This paper reviews the available literature and presents a clinical case to illustrate the diagnostic and therapeutic management of NECB. Methods: A literature review was conducted using databases such as PubMed, Medline, and Google Scholar to identify studies on NECB. Additionally, a clinical case of a patient diagnosed with NECB was analyzed, documenting her clinical presentation, diagnosis, treatment, and evolution. Results: NECB represents less than 1% of all breast cancers, with variability in its presentation and prognosis. The case of a patient with NECB who received systemic treatment based on chemotherapy is presented, exemplifying the management of this rare and diagnostically and therapeutically challenging tumor. Discussion: The diagnosis of NECB is complex due to the rarity of the tumor and the lack of specific clinical characteristics. Immunohistochemistry is crucial for confirming the diagnosis. The lack of standardized therapeutic guidelines complicates treatment, often necessitating the extrapolation of strategies from other invasive breast cancers. Conclusion: NECB is a rare and aggressive tumor with limited treatment options. Chemotherapy with cisplatin and etoposide can be effective, as observed in this case. Given the aggressive nature of this tumor and the few treatment options available, it is vital to consider participation in clinical trials to improve outcomes. Additionally, a multidisciplinary approach and evaluation by a tumor board are essential to guide therapeutic decisions and ensure the best possible care for these patients.
Abbreviations
NECB: Neuroendocrine carcinoma of the breast
NET: Neuroendocrine tumors
IHC: Immunohistochemistry
SEER: Surveillance, Epidemiology, and End Results
Introduction
Neuroendocrine tumors (NETs) are diverse neoplasms that accumulate and secrete peptide hormones or biogenic amines. These cells, similar to those of the nervous system, are distributed throughout the body, being most common in the gastroenteropancreatic tract and broncopulmonary system. Neuroendocrine carcinoma of the breast (NECB) is a rare and heterogeneous subtype lacking standardized therapeutic guidelines and having limited prospective clinical research [1,2].
The classification and morphological and immunohistochemical criteria for diagnosing NECB have evolved over the years, leading to a lack of uniformity in the terminology and definition of NETs. This lack of uniformity complicates the accurate assessment of the incidence of NECB, with reported morbidity ranging considerably from 0.1% to 19.5%. A study using the SEER database in breast cancer patients showed that, according to the WHO 2003 diagnostic criteria, only 0.1% of breast cancers are NECB, a figure lower than the 2-5% reported by the WHO in 2012 [3].
The recent 2022 WHO classification for neuroendocrine neoplasms has introduced significant changes. The nomenclature has been consolidated to distinguish neuronal paragangliomas from epithelial neoplasms, dividing them into well-differentiated NETs and poorly differentiated NETs [4].
NECB is a particular histological subtype of breast cancer with morphological characteristics similar to gastrointestinal and pulmonary NETs, although it shows some degree of heterogeneity. This includes certain features that are generally difficult to identify from invasive ductal carcinoma of no special type (NST) [5].
A retrospective analysis of the National Cancer Database (NCDB) from 2004 to 2017 revealed that NECBs tend to be of higher grade and present at a more advanced stage of the disease compared to invasive ductal carcinoma [6].
Histologically, primary invasive NETs of the breast are indistinguishable from their counterparts in the pulmonary region. High-grade NECB includes small cell and large cell neuroendocrine carcinomas, with the latter being extremely rare. Immunohistochemistry (IHC) is essential for identifying neuroendocrine phenotypes in breast cancer subpopulations, showing immunoreactivity to markers such as chromogranin A (CgA) and synaptophysin (Syn). Most NECBs show positivity for hormone receptors and negativity for HER-2, presenting a phenotype similar to the luminal subtype [7,8].
Molecularly, NECB has different mutational profiles compared to other luminal subtype breast cancers, with a lower frequency of PIK3CA mutations and a higher rate of mutations in other genes [9,10].
The clinical characteristics of NECB are similar to those of other breast tumors, generally presenting as a palpable mass in the breast and, in some cases, with involvement of other distant organs. The differential diagnosis of NECB includes metastases from extramammary NETs, such as those from the lung or gastrointestinal tract, which are differentiated through immunohistochemistry. Lymphomas, malignant melanomas, and invasive ductal carcinomas (NST type) that may present similar characteristics should also be considered. Additionally, solid papillary and mucinous carcinomas can also show neuroendocrine differentiation. Immunohistochemistry, using markers such as GATA3, mammaglobin, and GCDFP15, is essential to distinguish between a primary breast tumor and a metastasis [1,2].
He treatment of NECB is not well defined due to the rarity of these tumors. Therapeutic strategies are based on extrapolations from treatments used for invasive breast cancer, including surgery, chemotherapy, and radiotherapy. An individualized approach based on the clinical and molecular characteristics of the tumor is necessary. Participation in clinical trials and a multidisciplinary approach are essential to optimize treatment and improve the prognosis of patients with NECB [11].
In the metastatic setting, there are no specific treatments for NECB. Somatostatin analogs, used in gastro-pancreatic NETs, have not shown benefit in NECB. The use of CDK4/6 inhibitors (such as palbociclib) in combination with hormonal therapy has been investigated, showing promising results in subgroups of patients with NECB. Immunotherapy could be a potential therapeutic option, although there are still no consistent data demonstrating its benefit [12].
The prognosis of NECB is controversial, with contradictory data regarding survival. Although some studies suggest that NECB could be associated with worse outcomes compared to other breast cancer subtypes, the lack of uniformity in the definition and classification of these tumors makes direct data comparison difficult. More large-scale prospective studies are needed to better clarify the prognostic factors and improve treatment strategies for NECB [13].
This study aims to review the existing literature on neuroendocrine carcinoma of the breast and present a clinical case to illustrate its diagnostic and therapeutic management.
Materials and Methods
Objective and Study Design: The objective of this study is to review the existing literature on NECB and analyze a clinical case to provide a comprehensive understanding of its diagnosis and treatment.
Literature Review: An exhaustive search was conducted in databases such as PubMed, Medline, and Google Scholar using terms like "neuroendocrine carcinoma of the breast," "neuroendocrine tumors," and "differential diagnosis." Relevant studies published up to 2023 were included.
Clinical Case Analysis:
A case of a 70-year-old patient diagnosed with NECB was documented, including her clinical presentation, diagnosis through IHC, chemotherapy treatment, and clinical evolution.
Case report
A 70-year-old woman with a medical history of hypertension and diabetes mellitus presented with a right breast tumor of 1-month evolution, exhibiting rapid growth. Physical examination revealed a fixed, stony mass in the upper outer quadrant of the right breast with erythematous skin, and palpable right axillary lymphadenopathy. Breast ultrasound showed an irregular hypoechoic nodule measuring 21 x 15 mm (BIRADS 4). (Fig 1)
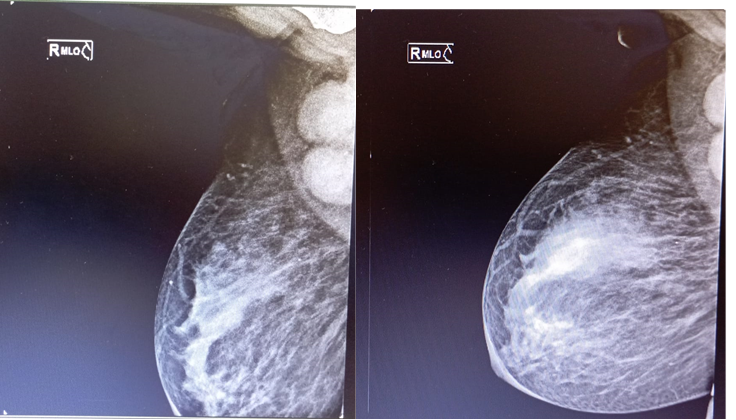
Fig 1: Mammogram, mediolateral oblique projection
The biopsy revealed an invasive carcinoma with neuroendocrine differentiation, positive for chromogranin A and synaptophysin, and negative for PAX8.
Staging CT and PET-CT scans showed axillary, supraclavicular, submaxillary, and subcarinal lymphadenopathy, along with mammary skin thickening and hypermetabolism in the right ovary. Biopsy of an axillary lymph node confirmed metastasis of high-grade neuroendocrine carcinoma (Ki-67 80%), with positivity for chromogranin A, synaptophysin, and cytokeratin AE1/AE3, and negativity for TTF-1, CK20, and CDx2. Hormone receptors and HER2 were negative (Fig 2)
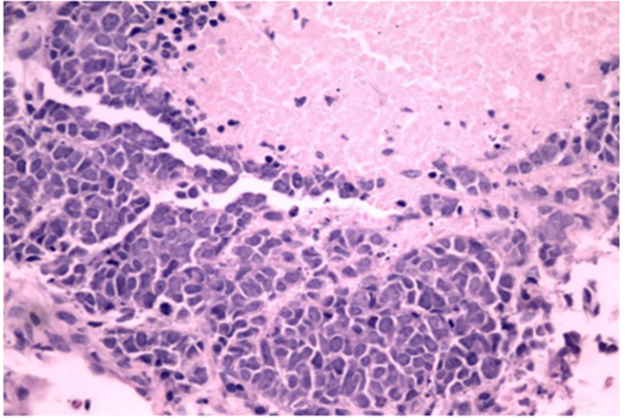
Fig 2: Biopsy of right axillary lymphadenopathy. Anatomopathological analysis.
It was discussed in the Tumor Board and determined to be triple-negative NECB, T2N3cM1, stage IV. Palliative treatment with cisplatin and etoposide-based chemotherapy was decided. After 6 cycles, with dose adjustments due to febrile neutropenia, the control CT scan showed a reduction in lymphadenopathy and the breast mass to 1 cm, with improvement in skin erythema and a decrease in axillary lymphadenopathy. The treatment was suspended, and regular follow-ups were planned.
Discussion
A 70-year-old female patient is presented, an age consistent with international literature reports for this type of tumor, with an incidence peak in the seventh decade of life [1,2].
She presented with a rapidly enlarging right breast tumor over the past month. Physical examination revealed a stony, fixed mass with erythematous skin in the upper outer quadrant of the right breast, accompanied by palpable right axillary lymphadenopathy. These clinical characteristics are typical of invasive ductal carcinomas (NST) and NECB, as NECB does not have a characteristic presentation [12].
In the imaging presentation, breast ultrasound revealed an irregular hypoechoic nodule measuring 21 x 15 mm (BIRADS 4). This is consistent with the literature, which indicates that most of these tumors appear on mammograms as high-density oval masses and on ultrasounds as hypoechoic, irregular masses with poorly defined margins, with or without posterior acoustic shadowing. Since these tumors do not have unique radiological features, the diagnosis is made through histology [7,8,14].
In the presented case, the core biopsy revealed an invasive carcinoma with neuroendocrine differentiation, necessitating a differential diagnosis between pulmonary or mammary origin. Immunohistochemical staining for neuroendocrine markers supported the diagnosis, showing positivity for chromogranin A, synaptophysin, cytokeratin AE1, AE3, and negativity for TTF-1, CK20, and CDx2, with a Ki-67 of 80%. Regarding the molecular subtype, most NECBs show positivity for hormone receptors and negativity for HER-2. However, in this case, there was no expression of hormone receptors or HER2, indicating a high-grade neuroendocrine carcinoma. Although cases of NECB with a triple-negative biological profile have been reported, their incidence is unclear [15,16].
It is important to consider that hormone receptor positivity alone is not sufficient to determine mammary origin, as these can also be expressed in metastatic NETs. Therefore, it is crucial to take into account relevant clinical history data to make an accurate diagnosis.
For tumor staging, the patient was studied with CT and PET scans, making it mandatory to rule out the possibility of breast metastases from other primary neuroendocrine tumors. In this case, 18-fluorodeoxyglucose PET was useful due to the high-grade nature of the neuroendocrine tumor. The CT scan showed right axillary lymphadenopathy, and the PET-CT identified lymph nodes and conglomerates in the right axilla, supraclavicular, and subcarinal regions, as well as a hypermetabolic right ovary, indicating disseminated disease with regional lymph node involvement, distant metastasis, and right ovarian metastasis. The most common sites of dissemination in NECB are the liver, bones, lungs, pancreas, and brain. No case reviews were found with ovarian involvement in patients with NECB [2,12].
Given the rarity of the case, it was discussed in the institution's tumor board. The main differential diagnoses were debated, including breast metastases from other primary neuroendocrine tumors (lung, gastro-pancreatic, and/or cervical), based on clinical, imaging, and pathological data. The treatment was also discussed, favoring the combination of cisplatin and etoposide for this high-grade, disseminated neuroendocrine tumor with a high proliferation rate. This regimen, consistent with previous studies, has demonstrated a response rate of over 60% [17]. Six cycles of chemotherapy were completed, requiring dose adjustments due to severe febrile neutropenia. The follow-up CT scan showed a reduction in lymphadenopathy and axillary conglomerates, leading to the decision to suspend treatment and continue with regular follow-ups.
Conclusion
Neuroendocrine carcinoma of the breast is a rare and challenging tumor, characterized by its aggressive nature and lack of standardized treatment options. Chemotherapy with cisplatin and etoposide, as observed in the presented clinical case, can be an effective therapeutic option for disease control. However, given the limited treatment options available and the aggressiveness of this tumor type, participation in clinical trials is highly recommended to improve outcomes in these patients. Additionally, a multidisciplinary approach is crucial to optimize the management of these patients. Tumor board reviews allow for more precise and personalized therapeutic decisions, ensuring that patients receive the best possible care. More prospective studies are needed to develop specific therapeutic guidelines and improve outcomes for patients with NECB.
Author’s Contribution
Clara Tambasco: Contributed to the study design, literature review, data collection, and initial drafting of the manuscript. Participated in the analysis and interpretation of data, and approved the final version of the manuscript.
Natalia Camejo: Provided significant contributions to the study design, literature review, and interpretation of data. Supervised the clinical aspects of the case study and contributed to the critical revision of the manuscript. Approved the final version of the manuscript. Corresponding author for all communication related to the manuscript.
Cecilia Castillo: Contributed to the study design and interpretation of data. Provided critical revisions and important intellectual content to the manuscript. Approved the final version of the manuscript.
Gabriel Krygier: Contributed to the study design and provided expertise in the oncological aspects of the study. Participated in the analysis and interpretation of data, and provided critical revisions to the manuscript. Approved the final version of the manuscript.
All authors have read and approved the final manuscript, and agree to be accountable for all aspects of the work.
Competing interest:
The authors declare that they have no competing interest.
References
- Yang, L., Lin, H., Shen, Y., Roy, M., Albarracin, C., Ding, Q., ... & Wu, Y. (2023). Clinical outcome and therapeutic impact on neuroendocrine neoplasms of the breast: a national cancer database study. Breast Cancer Research and Treatment, 202(1), 23-32.
- Mohamed, A., Zeidalkilani, J., Asa, S. L., Trybula, M., & Montero, A. J. (2024). Management of Neuroendocrine Breast Carcinoma (NEBC): Review of Literature. Oncology Reviews, 18, 12114.
- Wang, J., Wei, B., Albarracin, C. T., Hu, J., Abraham, S. C., & Wu, Y. (2014). Invasive neuroendocrine carcinoma of the breast: a population-based study from the surveillance, epidemiology and end results (SEER) database. BMC cancer, 14, 1-10.
- Rindi, G., Mete, O., Uccella, S., Basturk, O., La Rosa, S., Brosens, L. A., ... & Asa, S. L. (2022). Overview of the 2022 WHO classification of neuroendocrine neoplasms. Endocrine pathology, 33(1), 115-154.
- Sun, H., Dai, S., Xu, J., Liu, L., Yu, J., & Sun, T. (2022). Primary neuroendocrine tumor of the breast: current understanding and future perspectives. Frontiers in Oncology, 12, 848485.
- Martinez, E. O., Jorns, J. M., Kong, A. L., Kijak, J., Lee, W. Y., Huang, C. C., & Cortina, C. S. (2022). Primary breast neuroendocrine tumors: an analysis of the national cancer database. Annals of surgical oncology, 29(10), 6339-6346.
- Metovic, J., Cascardi, E., Uccella, S., Maragliano, R., Querzoli, G., Osella-Abate, S., ... & Papotti, M. (2022). Neuroendocrine neoplasms of the breast: diagnostic agreement and impact on outcome. Virchows Archiv, 481(6), 839-846.
- Kawasaki, T., Tashima, T., Enomoto, A., Kondo, T., Nagai, H., Nakamura, Y., ... & Kaira, K. (2023). Neuroendocrine neoplasms of the breast: diagnostic confusion and future perspectives. Virchows Archiv, 482(5), 929-930.
- Marchiò, C., Geyer, F. C., Ng, C. K., Piscuoglio, S., De Filippo, M. R., Cupo, M., ... & Reis‐Filho, J. S. (2017). The genetic landscape of breast carcinomas with neuroendocrine differentiation. The Journal of pathology, 241(3), 405-419.
- Peng, L., Ma, M., Zhao, D., Zhao, J., Sun, Q., & Mao, F. (2024). Comparison of clinical characteristics and outcomes in primary neuroendocrine breast carcinoma versus invasive ductal carcinoma. Frontiers in Oncology, 14.
- Trevisi, E., La Salvia, A., Daniele, L., Brizzi, M. P., De Rosa, G., Scagliotti, G. V., & Di Maio, M. (2020). Neuroendocrine breast carcinoma: a rare but challenging entity. Medical Oncology, 37, 1-8.
- Hasbay, B., Aytaç, H. Ö., & Bolat, F. A. (2022). Neuroendocrine tumors of the breast: single-center experience. European Journal of Breast Health, 18(1), 30.
- Yang, L., Roy, M., Lin, H., Shen, Y., Albarracin, C., Huo, L., ... & Wu, Y. (2021). Validation of prognostic significance of the proposed uniform classification framework in neuroendocrine neoplasms of the breast. Breast cancer research and treatment, 186, 403-415.
- Kayadibi, Y., Erginoz, E., Cavus, G. H., Kurt, S. A., Ozturk, T., & Velidedeoglu, M. (2022). Primary neuroendocrine carcinomas of the breast and neuroendocrine differentiated breast cancers: relationship between histopathological and radiological features. European Journal of Radiology, 147, 110148.
- Uccella, S. (2022). The classification of neuroendocrine neoplasms of the breast and its clinical relevance. Virchows Archiv, 481(1), 3-12.
- Uccella, S., Finzi, G., Sessa, F., & La Rosa, S. (2020). On the endless dilemma of neuroendocrine neoplasms of the breast: a journey through concepts and entities. Endocrine pathology, 31, 321-329.
- Yildirim, Y., Elagoz, S., Koyuncu, A., Aydin, C., & Karadayi, K. (2011). Management of neuroendocrine carcinomas of the breast: A rare entity. Oncology letters, 2(5), 887-890.


