Research Article | DOI: https://doi.org/10.58489/2836-5038/006
Observational Survey to Assess Platelet Concentration and Ani - Microbial Potency of Different Blood Extracts
1. Department of Periodontology, Babu Banarasi Das College of Dental Sciences, Lucknow
2. Department of Oral Pathology, Babu Banarasi Das College of Dental Sciences, Lucknow
3. Department of Public Health Dentistry, Institute of Dental Sciences, Bareilly
4. Institute of Dental Sciences, Bareilly
*Corresponding Author: Arjun Singh
Citation: Arjun Singh ,2023. Snigdha Biswas, Deba Kumar Das, Nagma Raj,Observational Survey to Assess Platelet Concentration and Anti-Microbial Potency Of Different Blood Extracts,International Journal of Stem cells and Medicine. 2(1). DOI: 10.58489/2836-5038/006.
Copyright: © 2023 Arjun Singh,this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 02 January 2023 | Accepted: 10 January 2023 | Published: 21 January 2023
Keywords: Platelet Concentrates, Antimicrobial Efficacy, PRP, PRF And IPRF
Abstract
Introduction: Platelet concentrates have gained popularity in periodontal regenerative therapy because of its autologous nature. it promotes wound healing after surgical periodontal therapy.
Aim: to study the platelet count and antimicrobial efficacy of various platelet concentrates, such as PRP, PRF and IPRF
Methodology: An Observational Study was carried out at Department of Periodontology & Implantology at Babu Banarasi das College of Dental Sciences. Sample size was 45. Ten ml of blood was drawn from the patient out of which 3ml each of blood will be used for PRP, PRF and I-PRF preparation and remaining 1ml of blood was used for determining the platelet count. For I-PRF preparation, 3ml of blood wias used, d centrifuged at 700 rpm for 3 minutes. For PRF preparation, Agar plates will be inoculated with plaque sample of same patient and will be labelled and divided into 3 compartments. Wells was prepared in the inoculated agar plate and 0.1 ml of PRP, PRF and I-PRF will be placed in those wells. Inoculated blood agar plates was then incubated aerobically at 37℃ for 24 hours to 48 hours.
Results: The platelet count of i-PRF was statistically significant when compared to control (P < 0.001). It was also significant when compared to PRP (P < 0.01) and PRF (P < 0.001). Mean zone of inhibition around i-PRF (P < 0.01) and PRF (P < 0.05) reached statistical significance. Although a distinct zone of inhibition was seen with PRP, it was not statistically significant (P > 0.05).
Conclusion: In the present study, although a distinct zone of inhibition was obtained with all test samples, it was significant with only i-PRF and PRF.
Introduction
Periodontitis is an inflammatory condition that gradually destroys the tooth's supporting tissues and is brought on by a particular bacterium or a collection of microorganisms[1]. Progressive bone loss and attachment loss result from this. Hence, the goal of periodontal therapy is to replace any destroyed periodontal structures.
Since they are autologous, platelet concentrates have recently become more popular in periodontal regeneration therapy. The reason for its regenerative capacity is because platelet -granules contain a variety of growth factors that are released at the local site upon activation. As a result, it aids in wound healing following surgical periodontal therapy. Additionally, they exhibit anti-inflammatory qualities, which lessen postoperative discomfort and swelling. [2]
Additionally, fibrin, fibronectin, and vitronectin are secreted by platelets; these compounds serve as a connective tissue matrix and adhesion molecules for more effective cell migration. As a result, these are essential for osteoid development, collagen synthesis, and cell proliferation. 2
According to recent studies, periodontal disorders are managed using platelet concentrates.
Platelets, white blood cells, red blood cells, and plasma are the basic building blocks of human blood. These blood platelets play a crucial function in wound healing by releasing growth factors at the site of injury.
In addition to their capacity for regeneration, platelet concentrates have been shown to have antibacterial action against a number of pathogens, including Staphylococcus aureus, Escherichia coli, Klebsiella pneumoniae, and Streptococcus oralis.
It is well known that the leukocytes in PRF have antibacterial properties. Since I PRF was only recently launched, there isn't much proof that it has an antibacterial effect on certain periodontal infections. I PRF is being researched for its ability to promote regeneration and the release of growth factors, but due to its simplicity in preparation and ability to be combined with other biomaterials, it also needs to be examined for its antibacterial qualities. The study's primary objective was to examine the platelet count and antibacterial effectiveness of several platelet concentrates, including PRP, PRF, and IPRF. Additionally, the goals included examining the platelet counts in PRP, PRF, and IPRF as well as the antibacterial effects of various platelet concentrates on bacterial plaque.
Methodology
At the Babu Banarasi Das College of Dental Sciences in Lucknow, an observational research was conducted by the departments of oral pathology, microbiology, and periodontology & implantology. The sample size was 45. The research comprised individuals with normal periodontium, patients with gingivitis, patients with periodontitis, and individuals between the ages of 18 and 50. Additionally, those who smoked or chewed tobacco, had any systemic diseases, were pregnant or nursing, or had used antibiotics or inflammatory medicines during the previous six months were eliminated. In their native tongue, the patient was told about the procedures and potential results, and written informed agreement was acquired.
The personalised case history questionnaire . the questionnaire was used to record the demographic information for each participant. Ten millilitres of blood were taken from the patient, of which three millilitres each would be used to prepare PRP, PRF, and I-PRF. The remaining one millilitre of blood was used to calculate the platelet count in accordance with the standards established by Kour P, et al. 1 3 ml of blood were used to prepare the I-PRF; this blood was collected in a vacutainer without any additives and centrifuged for three minutes at 700 rpm. In order to prepare the PRF, 3ml of blood was drawn into a glass collection tube with no other ingredients and centrifuged for 10 minutes at 3000 rpm. Blood was drawn into a collecting tube containing 3.2% sodium to prepare PRP and centrifuged at 1000 rpm for 13 minutes.
The plasma's outermost layer will be eliminated. Following this, a second cycle of centrifugation will be performed for ten min at 2000 rpm. The lower half of the plasma will be used to test the antibacterial activity while the upper half will be discarded. 1 Agar plates will be labelled and separated into three compartments before being injected with a plaque sample from the same individual. On the wells that were formed in the inoculated agar plate, 0.1 ml each of PRP, PRF, and I-PRF will be added. After being incubated aerobically at 37°C for 24 to 48 hours with inoculated blood agar plates, the zone of inhibition was then reached. 2 Clinical screenings for Normal Periodontium, Gingivitis and Periodontitis as per criteria given by Armitage (1999) will be performed on all patients entering the Periodontology and Implantology Department's Outpatient Clinic.[3]
In the Microsoft Excel spreadsheet, data were recorded. Calculated descriptive statistics included frequency distribution and percentages. To determine whether there is a statistically significant difference between the means of three or more independent groups, inferential statistics like one-way ANOVA (Analysis of Variance) will be used, and post-hoc Tukey's test will be used to examine the difference between the variables utilising SPSS.
Results
The purpose of this research was to evaluate the platelet count and antimicrobial effectiveness of several platelet concentrates, including PRP, PRF, and IPRF. the antibacterial effectiveness of various platelet concentrates on bacterial plaque, as well as the amount of platelets in PRP, PRF, and IPRF.
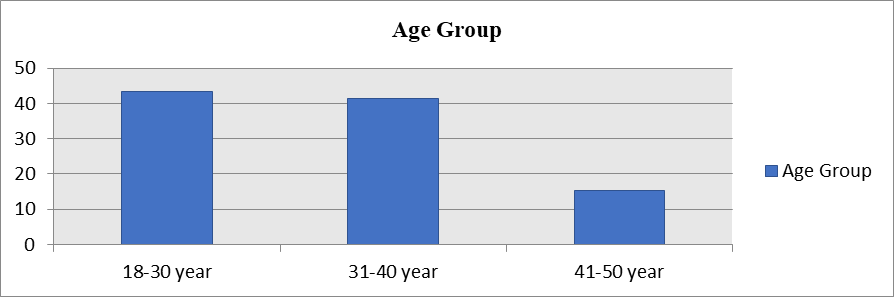
Graph 1 Age Group distribution among studied population
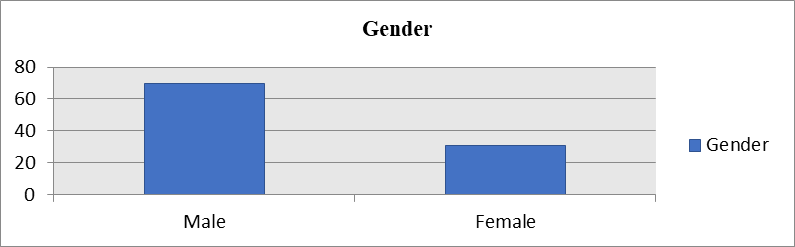
Graph-2 Gender distribution among studied population
Table-1 Quantification of platelets
| Platelet count/mm3 | p-value |
i-PRF | 1,434,000 ± 75,233 |
P < 0> |
PRP | 1,343,000 ± 81,486 | |
PRF | 249,000 ± 61,319 | |
Control | 291,000 ± 51,575 |
Comparing the platelet count of the i-PRF to the control, the difference was statistically significant (P 0.001). Additionally, it was significant when compared to PRP and PRF (P 0.01) and P 0.001. This shows that, in compared to certain other concentrations, i-PRF has the most platelets.
Table-2 Evaluation of antimicrobial potential
Antimicrobial Efficacy | Mean zone of inhibition (in cm) | p-value |
i-PRF | 1.42 ± 0.25 | P < 0> |
PRP | 1.3 ± 0.16 | P > 0.05 |
PRF | 1.02 ± 0.12 | P < 0> |
The presence of a distinct zone of inhibition around the samples served as evidence of the antibacterial effectiveness. Around i-PRF, PRF, and PRP, the mean zones of inhibition (measured in cm) were 1.42 0.25, 1.3 0.16, and 1.02 0.12, correspondingly. The mean zone of inhibition around the PRF and i-PRF reached statistical significance (P 0.01) and (P 0.05), respectively. Despite the fact that PRP produced a well-defined zone of inhibition, it was not statistically significant (P > 0.05). These findings suggest that, in comparison to other platelet concentrates, i-PRF significantly inhibits the proliferation of oral bacteria.
Table-3 Evaluation of Gingivitis Patients
Gingivitis Patients | |||
Parameters | N | Mean | Std. Deviation |
BOP | 15 | 2.52 | .510 |
PPD | 15 | 2.96 | .841 |
CAL | 15 | 1.56 | .507 |
Whole blood | 15 | 202515.12 | 45676.134 |
PRP | 15 | 1865649.52 | 266897.538 |
PRF | 15 | 2397508.00 | 381263.907 |
I-PRF | 15 | 3068625.60 | 258936.375 |
There were 15 participants with periodontitis out of the population of 45. We discovered that whereas the mean pocket probing depth was 3.95 with a standard deviation of 1.638, the mean bleeding of probing was 3.15 with a standard deviation of 1.040. According to Table 3, the mean of whole blood was 209558.45 with a standard deviation of 47542.014 and the mean of CAL was 2.35 with a standard deviation of 1.268.
Table-4 Evaluation of Periodontitis patients
Periodontitis patients | |||
Parameters | N | Mean | Std. Deviation |
BOP | 15 | 3.15 | 1.040 |
PPD | 15 | 3.95 | 1.638 |
CAL | 15 | 2.35 | 1.268 |
Whole blood | 15 | 209558.45 | 47542.014 |
PRP | 15 | 1931008.10 | 276244.256 |
PRF | 15 | 2506691.50 | 355532.141 |
I-PRF | 15 | 3130957.50 | 265201.795 |
Out of an overall sample size of 45 patients, 15 were healthy. The mean pocket probing depth was 1.38 with a standard deviation of 619, whereas the mean bleeding during probing was.00 with a standard deviation of.000. According to Table 4, the mean of whole blood was 1572781.25 with a standard deviation of 466820.523 and the mean of CAL was 1.13 with a standard deviation of.719
According to Table 4, the mean for PRP was 2187260.63 with a standard deviation of 696143.908; for PRF, it was 2665323.75 with a standard deviation of 762564.486; and for I-PRF, it was.89 with a standard deviation of.248.
Table-5 Evaluation of Healthy patients
Healthy Patients | ||||
Parameters | N | Mean | Std. Deviation | |
BOP | 15 | .00 | .000a | |
PPD | 15 | 1.38 | .619 | |
CAL | 15 | 1.13 | .719 | |
Whole blood | 15 | 1572781.25 | 466820.523 | |
PRP | 15 | 2187260.63 | 696143.908 | |
PRF | 15 | 2665323.75 | 762564.486 | |
I-PRF | 15 | .89 | .248 | |
Discussion
Periodontal regeneration requires a variety of biological processes, including coordinated cell adhesion, migration, proliferation, and differentiation. To achieve periodontal rehabilitation, regenerative operations using both soft- and hard-tissue grafts are carried out. Platelets are essential for the healing of wounds. Once engaged, they start to release growth factors such insulin-like growth factor, tgf, and platelet-derived growth factor (PDGF). Additionally, fibrin, fibronectin, and vitronectin are secreted by platelets; these molecules serve as a connective tissue matrix and adhesion molecules for more effective cell migration. As a result, they are essential for osteoid development, collagen synthesis, and cell proliferation. As a result, many autologous platelet concentrate procedures, including PRP and PRF, were developed over time. [4,5,6]
Despite becoming an autologous formulation, PRP needs to be activated with thrombin and calcium. These chemicals have the potential to both cause an immunological response and the production of antibodies against the clotting factors V, XI, and thrombin, which would negatively impact the coagulation procedure. Choukron's second-generation platelet concentration is called PRF (2001). It is simple to prepare and has excellent handling qualities. Because no bovine thrombin or anticoagulant is used, there are far fewer hazards involved in treating blood biochemically and using any supplements. An advantageous physiologic framework for wound healing is created by the gradual polymerization of fibrinogen into fibrin, which is caused by the physiologically accessible thrombin found in PRF. The proteolysis of the growth factors is prevented by this fibrin network. Additionally, PRF encourages the growth of microvascularization, which results in more effective cell movement.[7]
I-PRF was created with the extra benefit of being in injectable form, built on a principle identical to that of PRF. This parenteral version of PRF can easily mixed with different biomaterials or used alone. The foundation of its technique is the idea that a slower, quicker centrifugation spin produces a larger presence of regeneration cells with a greater level of growth factors. [8]
In a new analysis, it was found that whereas PRP gradually disintegrated over time, i-PRF created a tiny clot because of fibrin elements that functioned as a dynamic gel with cells probably retained within its hydrogel. Thus, despite the fact that PRP was discovered to have been destroyed by that point, it was anticipated that an additional release of growth factors from i-PRF could be expected after 10 days.[ 9]
Several automated technologies are capable of evaluating platelet counts. Nevertheless, it was shown that there was no discernible difference between the two approaches in a research published by Bajpai et al. to estimate the platelet count using the automated cell counting and the peripheral smear technique. The method of platelet estimation by peripheral smear, according to the researchers, is effective as a quick and affordable way to determine platelet count. [10]
With the exception of PRF, all of the substances used in this investigation were liquids that could be easily smeared on glass slides and stained. Since PRF was only available as clots, the platelet count of the remaining serum was used to estimate PRF's platelet count. For the determination of the platelet count in the PRF clot, Suchetha et al. conducted a comparable analysis. [11] In the current investigation, the highest platelet count was seen in the i-PRF group, and this difference was statistically significant. This might be explained by the longer centrifugation time and slower centrifugation speed. The "low-speed idea" for blood centrifugation was developed by Ghanaati et al., who found that slower centrifugation rates resulted in increased concentrations of cells, particularly leukocytes, prior to the development of clots.8
In the latest research, it was found that the number of platelets increased in both i-PRF and PRP by 503% and 464%, respectively. As contrasted to all of the blood, the PRF clot had a platelet concentration of roughly 87%. Additional growth factors have been proven to be released from preparations with greater platelet counts. Miron et al. revealed that whereas i-PRF showed significantly higher levels of total long-term release of these factors, PRP generally had higher levels of early release of growth factors. The results showed that i-PRF can release larger levels of different signaling pathways, increase fibroblast migration, and increase the expression of PDGF, TGF-, and collagen1.[12].
Prior research has been done to assess the antibacterial effectiveness of platelet concentrates like PRP and PRF. The recently unveiled i-PRF is not extensively studied. It was found in the current investigation that i-PRF displayed a maximal zones of inhibition around oral microbiota, measuring 1.42 0.25 (in cm). i-PRF > PRF > PRP was the sequence of the zone of inhibition from highest to lowest. In one investigation, Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans were subjected to PRP and PRF's antibacterial activity. P. gingivalis and A. actinomycetemcomitans were observed to be suppressed by PRP but not PRF. [13] In a different investigation, PRF showed a distinct zone of inhibition against a subgingival plaques sample, and colorimetric result reveals that PRF caused the least amount of turbidity. [14]
Even though a clear zone of inhibition was established with all test samples in the current study, only i-PRF and PRF had significant zones of inhibition. The secretion of a wide variety of potent antimicrobial peptides, as well as the production of oxygen metabolites like superoxide, hydrogen peroxide, and hydroxyl free radicals, adhesion, aggregation, and internalisation of microorganisms, have all been proposed as possible mechanisms for the antibacterial effect of platelet-derived preparations. 53 Yeaman suggested that direct bacterial killing could occur as a consequence of platelet contact with pathogens, involvement in antibody-dependent cell cytotoxicity, and entrapment of white blood cells within PRF. Along with this myeloperoxidase production, it has also been proposed that the immune system's antigen-specific responses and antioxidant responsive components are activated. [15]
Conclusion
In the present study, although a distinct zone of inhibition was obtained with all test samples, it was significant with only i-PRF and PRF.
References
- Kour P, Pudakalkatti PS, Vas AM, Das S, Padmanabhan S. Comparative evaluation of antimicrobial efficacy of platelet-rich plasma, platelet-rich fibrin, and injectable platelet-rich fibrin on the standard strains of Porphyromonas gingivalis and Aggregatibacter actinomycetemcomitans. Contemporary Clinical Dentistry. 2018;9(2):325-30.
View at Publisher | View at Google Scholar - Karde PA, Sethi KS, Mahale SA, Khedkar SU, Patil AG, Joshi CP. Comparative evaluation of platelet count and antimicrobial efficacy of injectable platelet-rich fibrin with other platelet concentrates: An in vitro study. Journal of Indian Society of Periodontology. 2017;21(2):97-9.
View at Publisher | View at Google Scholar - Armitage GC. Development of a classification system for periodontal diseases and conditions. Annals of Periodontol. 1999;4(1):1-6.
View at Publisher | View at Google Scholar - Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. 2006;Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod.101:e37–44,
View at Publisher | View at Google Scholar - Pradeep AR, Shetty SK, Garg G, Pai S. 2009;Clinical effectiveness of autologous platelet-rich plasma and Peptide-enhanced bone graft in the treatment of intrabony defects. J Periodontol. 80:62–71.
View at Publisher | View at Google Scholar - Lucarelli E, Beretta R, Dozza B, Tazzari PL, O'Connel SM, Ricci F, et al. A recently developed bifacial platelet-rich fibrin matrix. Eur Cell Mater. 2010;20:13–23.
View at Publisher | View at Google Scholar - Preeja C, Arun S. 2014; Platelet-rich fibrin: Its role in periodontal regeneration. Saudi J Dent Res. 5:117–22.]
View at Publisher | View at Google Scholar - Ghanaati S, Booms P, Orlowska A, Kubesch A, Lorenz J, Rutkowski J, et al. 2014;Advanced platelet-rich fibrin: A new concept for cell-based tissue engineering by means of inflammatory cells. J Oral Implantol.40:679–89
View at Publisher | View at Google Scholar - Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, et al. 2017;Injectable platelet rich fibrin (i-PRF): Opportunities in regenerative dentistry? Clin Oral Investig.2:1–9
View at Publisher | View at Google Scholar - Bajpai R, Rajak C, Poonia M. Platelet estimation by peripheral smear: Reliable, rapid, cost-effective method to assess degree of thrombocytopenia. Int J Med Sci Res Pract. 2015;2:90–3.
View at Publisher | View at Google Scholar - Suchetha A, Lakshmi P, Bhat D, Mundinamane DB, Soorya KV, Bharwani GA. 2015; Platelet concentration in platelet concentrates and periodontal regeneration-unscrambling the ambiguity. Contemp Clin Dent. 6:510–6.
View at Publisher | View at Google Scholar - Miron RJ, Fujioka-Kobayashi M, Hernandez M, Kandalam U, Zhang Y, Ghanaati S, et al. 2017;Injectable platelet rich fibrin (i-PRF): Opportunities in regenerative dentistry? Clin Oral Investig.;2:1–9
View at Publisher | View at Google Scholar - Badade PS, Mahale SA, Panjwani AA, Vaidya PD, Warang AD. 2016;Antimicrobial effect of platelet-rich plasma and platelet-rich fibrin. Indian J Dent Res. 27:300–4.
View at Publisher | View at Google Scholar - Joshi CP, Patil AG, Karde PA, Khedkar SU, Mahale SA, Dani NH, et al. 2016;Autologous platelet rich fibrin as a potential antiperiopathogenic agent: An in-vitro study. Int J Periodontol Implantol 1:50–4.
View at Publisher | View at Google Scholar - Yeaman MR. The role of platelets in antimicrobial host defense. Clin Infect Dis. 1997;25:951–68.
View at Publisher | View at Google Scholar