Current Issue : Article / Volume 2, Issue 1
- Case Report | DOI:
- https://doi.org/10.58489/2994-2624/007
Point of care transcranial doppler guiding the efficiency of selective cerebral perfusion during extracorporeal circulation for surgical repair of aortic arch hypoplasia with ligation of patent ductus arteriosus and pulmonary artery banding: a case r
a. Hospital das ClÃnicas, Universidade Federal de Minas Gerais - Av. Alfredo Balena
Dra. Marina Ayres Delgado
F. S. Ferreira; A. C. F. de Oliveira; M. A. Delgado; L. F. A. P. de Oliveira, (2023) point of care transcranial doppler guiding the efficiency of selective cerebral perfusion during extracorporeal circulation for surgical repair of aortic arch hypoplasia with ligation of patent ductus arteriosus and pulmonary artery banding: a case report Transcranial doppler monitoring in pediatric cardiac surgery. International Journal of Anesthesiology and Practice (IJAP).2(1). DOI: 10.58489/2994-2624/007
© 2023 Marina Ayres Delgado, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 11-01-2023
- Accepted Date: 24-01-2023
- Published Date: 31-01-2023
anesthesia, transcranial doppler, intraoperative neuromonitoring, total circulatory arrest, pediatric cardiac surgery.
Abstract
The perioperative management of patients undergoing major surgery at high risk of developing neurological complications should include an individualized strategy for neuromonitoring in order to avoid potential brain insults. In this case report, we present our experience in the intraoperative management of an aortic coarctation correction surgery with pulmonary banding, where Transcranial Doppler (TCD) monitoring provided informations about cerebral blood flow. In this report we highlight the benefits of TCD in the optimization of cerebral perfusion and oxygen delivery which can be decisive in improving the postoperative outcome.
Introduction
Transcranial Doppler is an ultrasound technique that uses blood vessel flow velocities to evaluate cerebral blood flow and it is capable of not only screening but also quantitative assessment of cerebral hemodynamics and is currently being incorporated as part of multimodal strategy for neuromonitoring, particularly in patients at high risk for postoperative neurological dysfunction. TCD is non-invasive, safe and easy to perform. [1,2] We described the anesthetic management during an open-heart surgery to correct aortic arch hypoplasia and the use of a Transcranial Doppler as a way to confirm the diagnosis of cerebral hypoperfusion.
Case Report
H.G.S, one-month-old, diagnosed with a complex congenital cardiopathy, characterized by a total Atrioventricular Septum Defect (AVSD), left atrium isomerism, persistent ductus arteriosus (PDA), hypoplasia of aortic arch, aortic coarctation, interatrial communication (IAC), right ventricle hypertrophy and pulmonary hypertension (PH). Patient was scheduled for an aortic arch hypoplasia repair surgery, with ligation of patent ductus arteriosus and pulmonary artery banding.
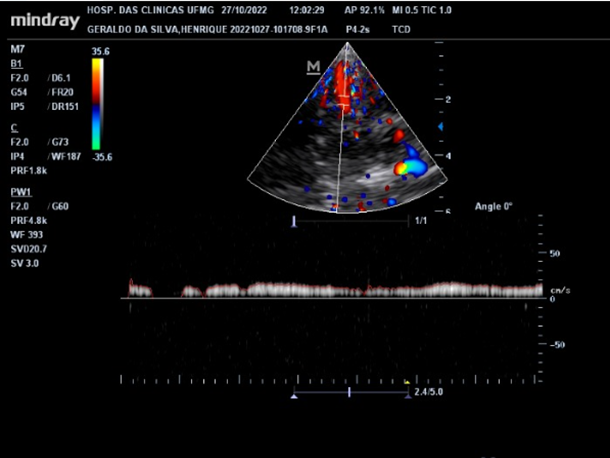
An intramuscular sedation with ketamine 1mg/kg and dexmedetomidine 1µ/kg was performed in order to puncture the right radial artery for invasive blood pressure monitoring. The right internal jugular vein catheterization was performed with a 5 Fr double lumen catheter. General anesthesia was induced with propofol 1mg/kg, fentanyl 2µ/kg, lidocaine 1.5mg/kg, rocuronium 1mg/kg and maintained with dexmedetomidine 0.4µ/kg/h, ketamine intermitent bolus 0.2mg/kg/h, and sevoflurane 0.7MAC. Intubation was achieved with a 4mm uncuffed endotracheal tube. Before the cardiopulmonary bypass (CPB), the first TCD exam was performed, which showed the absence of diastolic flow in the middle cerebral artery (MCA). These findings are compatible with a limited cerebral flow due to the aortic arch hypoplasia and consequent decrease in the flow of the carotid artery (Figure 1).
During CPB, sevoflurane was discontinued and total intravenous anesthesia was maintained with propofol infusion titrated to maintain BIS = 0 and SR = 100, and 0.6mg/kg rocuronium bolus.

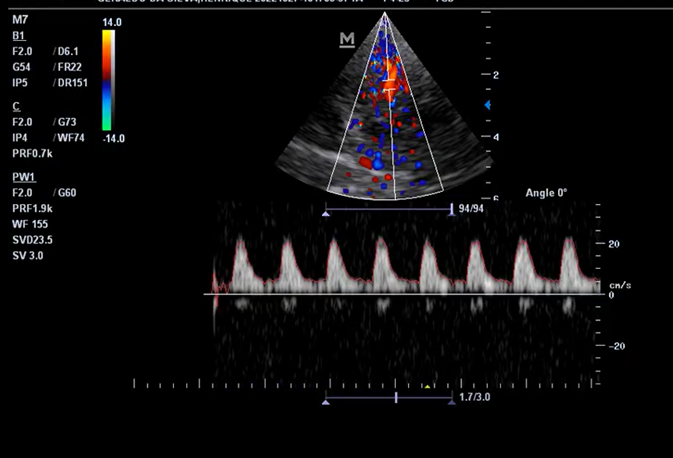
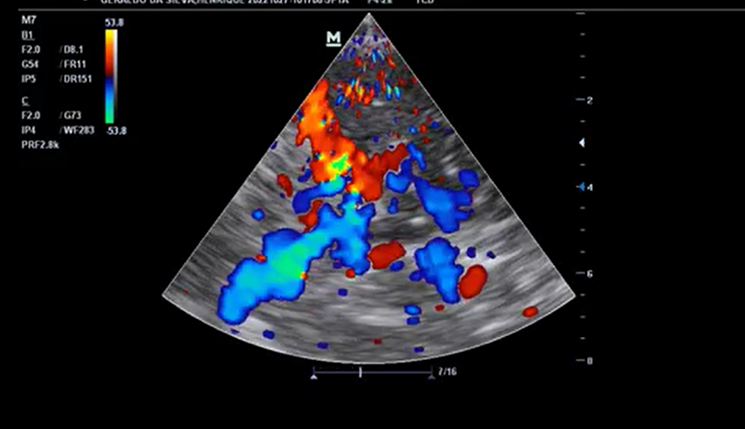
The patient was maintained in moderate hypothermia (20.1 to 28 degrees C) and a selective antegrade perfusion through the brachiocephalic trunk with flow of 12ml/kg/min) was initiated. TCD showed poor cerebral blood flow, with flow velocity less than 20cm/s in the right middle cerebral artery and intermittent flow interruptions (figure 2). During CPB, the selective antegrade blood flow was increased to 15ml/kg/min in order to normalize the MCA flow velocity. (Figure 3)
CPB was terminated with 115 min aorta cross-clamp time and 140 min of CPB. Adrenaline 0.05µg/kg/min and milrinone 0.5µg/kg/min were initiated to maintain macrohemodynamic parameters within established values for the patient’s age. New MCA flow velocity exams showed the appearance of diastolic flow, which is compatible with a successful repair of the aortic arch.

After surgical procedure, a bilateral superficial parasternal block was performed as part of the multimodal analgesia plan and the patient was transferred to the intensive care unit (ICU). The patient had good progress in the ICU with reduction of adrenaline and milrinone doses and extubation.
Discussion
The incidence of postoperative cognitive dysfunction in cardiac surgery has been estimated up to 25%, one of the contributing risk factors is hypoperfusion because of impaired autoregulation. Without the autoregulation of cerebral vessels, the range of CPP values that prevents cerebral hypoperfusion is narrow and difficult to determine without proper monitoring. The TCD also has good sensitivity for detecting emboli, another major risk factor for neurological complications.[1]
The repair of aortic arch hypoplasia associated with coarctation of the aorta was performed through the construction of a neo-aorta with reimplantation of the aortic arch vessels, ligature of the patent ductus arteriosus (DA) and a pulmonary banding. A previous TCD showed a patent polygon of Willis, which could contribute to perfusion of the contralateral cerebral hemisphere during anterograde perfusion.[1] (Figure 5).
During an open-heart surgery with circulatory arrest, the main concern is the cerebral perfusion. It is estimated that, with a deep hypothermic circulatory arrest (DHCA, nasopharyngeal temperature 14.1–20.0 ℃), the brain is adequately preserved for approximately 30 minutes. In moderate hypothermia (MHCA, nasopharyngeal temperatures 20.1–28.0 ℃), this period is reduced to approximately 10 minutes.[3] In this way, anterograde or retrograde cerebral perfusion could be used to preserve brain tissue through a longer period.[4]
During the procedure, TCD has been used at different stages to avoid neurological complications related to cerebral malperfusion, aiming at an attempt to decrease the potential for cerebral damage related to Aortic repair techniques extending to the transverse aortic arch. Throughout antegrade selective perfusion, TCD showed that the programmed flow of 12ml/kg/min was insufficient to maintain adequate cerebral flow, demonstrated by the interruption of the flow wave on the RMCA Doppler and flow velocity less than 20cm/s (figure 2). Both morphology and velocity normalized after increasing the selective perfusion flow to 15ml/kg/min (figure 3), suggesting that even selective perfusion flow values within the established in the literature could result in low cerebral flow, highlighting the need of monitoring to titrate selective perfusion flow.[5] In addition, progressive improvement of cerebral circulation was evidenced as cerebral blood flow was increased after CPB. The appearance of a diastolic flow occurred because surgical repair of the aorta improved the elasticity of the vessel as evidenced by the appearance of diastolic flow in the cerebral vessels, which depends on the physiological recoil of the aorta during diastole.
This report showed the importance of a neuromonitoring modality in the perioperative period and in this context and the role of the TCD in improving outcomes.
References
- Polito A, Ricci Z, Di Chiara L, Giorni C, Iacoella C, Sanders SP, Picardo S(2006). Cerebral blood flow during cardiopulmonary bypass in pediatric cardiac surgery: the role of transcranial Doppler--a systematic review of the literature. Cardiovasc Ultrasound. Dec 13; 4:47.
- https://janesthanalgcritcare.biomedcentral.com/articles/10.1186/s44158-022-00082-3
- Yan TD, Bannon PG, Bavaria J, Coselli JS, Elefteriades JA, Griepp RB, Hughes GC, LeMaire SA, Kazui T, Kouchoukos NT, Misfeld M, Mohr FW, Oo A, Svensson LG, Tian DH (2013). Consensus on hypothermia in aortic arch surgery. Ann Cardiothorac Surg. Mar;2(2):163-8.
- https://www.sciencedirect.com/science/article/pii/S1053077020312702
- Spielvogel D, Kai M, Tang GH, Malekan R, Lansman SL(2012). Selective cerebral perfusion: a review of the evidence. J Thorac Cardiovasc Surg. 2013 Mar;145(3 Suppl):S59-62. doi: 10.1016/j.jtcvs.2012.11.073. Epub 2012 Dec 22. PMID: 23266253.replacement procedure: a pilot study. ASAIO J. Mar-Apr;58(2):122-6.


