Archive : Article / Volume 2, Issue 3
- Case Report | DOI:
- https://doi.org/10.58489/2836-5062/013
Spinal Nerve Sheath Myxoma
Department of Neurosurgery, Mustapha PACHA Hospital Algiers, Algeria
BELGACEM I
BELGACEM I, (2023). Spinal Nerve Sheath Myxoma: A Case Report. Journal of Clinical Oncology Reports.2(3) DOI: 10.58489/2836-5062/013
© 2023 BELGACEM I this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 09-04-2023
- Accepted Date: 20-04-2023
- Published Date: 24-04-2023
spinal cord; nerve sheath myxoma; teraparsec
Abstract
Nerve sheath myxoma (NSM) is a rare myxoid form of schwannoma, which is a benign tumor that usually grows in the same place. They usually arise from small cutaneous nerves in the head, neck, and extremities, but exceptionally, they have also been reported to develop in the spinal canal. Here we describe a case of spinal NSM. The patient was a 4-month-old male who presented with incomplete tetra paresis. Spine magnetic resonance imaging showed a well-demarcated small intradural extramedullary mass at the T10-L1 level. The tumor has typical histological features of myxoid type NSM with myxoid lobules that are separated by fibrous septa or bands of more compact cellular area. Nerve sheath myxomas should be included in the differential diagnosis of spinal canal tumors. Ultrastructural observation of tumor cefis with perineurial, fibroblast-like, and Schwann differentiation suggests an origin from nerve sheath precursor cefis.
Introduction
In 1969, Harkin and Reed first described nerve sheath myxoma, a rare benign tumor of nerve sheath originating from the dermis and subcutaneous tissues [1, 12]. In 2005, pathologist John Fetsch described 57 cases of nerve sheath myxomas, of which 86% occurred in the extremities, with the hands, fingers, knees, pretibial region, ankles, and feet being the most common sites. Only 12.3% of patients exhibited symptoms in the trunk or head-neck region [13]. Myxomas of the intraspinal nerve sheath are rare. Only eight cases of intraspinal nerve sheath myxoma have been reported to date, according to our knowledge [5–11]. However, no cases of nerve sheath myxoma in the cervical spinal canal have been reported. The central nervous system (CNS) [5, 13] is an unusual location for this tumor. Here, we describe an additional case of spinal NSM and include a literature review. The ultrastructural findings of the present case suggest a histogenesis from nerve sheath precursor cells.
Case Study
L.GH aged two months, is already hospitalized in the pediatric department for the exploration of an infectious syndrome with anemia. Refer to our department for the exploration of hypotonia with the abolition of osteotendinous reflexes in both legs. The admission examination found a reactive, conscious infant with an altered general condition and significant skin and mucous membrane paleness. A predominantly right flaccid Paraplegia, anesthesia in all modes of the right lower limb with areflexia, an anal gap, an umbilical hernia, and an inguinal hernia Spine magnetic resonance imaging (MRI) showed an intradural extramedullary right anterolateral mass at the Thl0-LI level (Fig. 1), 90 * 06 *27 mm, in hyperintensity 1 TI and heterogeneous T2. The mass was well-enhanced and compressed the cons medullaris without sign of infiltration, and there was also no evidence of cerebral abnormality. The results of the electromyogram examination Shows preganglionic neurogenic damage or neuropathy. Under the suspicion of schwannoma, the patient underwent an extended laminotomy from D10 to D12, and the mass was found to be contiguous with the nerve root; nevertheless, near total resection was achieved (Fig. 02). His postoperative course was uneventful, and the patient achieved a satisfactory, although partial, recovery, but a subtle numbness remains in both legs. Several control spinal MRIs have been requested and do not reveal any recurrence or tumor remnants (Fig. 3).


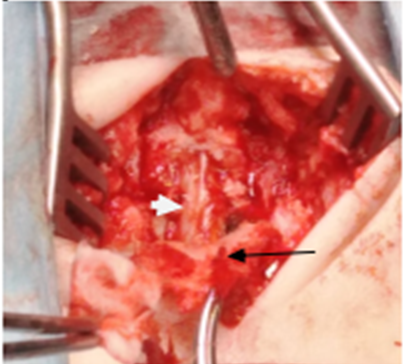

Pathological findings: An abundant myxoid matrix containing spindle-shaped cells mixed with irregularly shaped, thick, hyalinized vasculature and perivascular lymphoid infiltrates were predominantly observed in the interlobular septa and fibrous capsule.
Discussion
Tambourine et al. reported paravertebral muscle myxomas eroding the spine and causing spinal cord compression [6 and 12]. Only one case of an epidural has been reported in the literature [2], and ours is the second. Two cases have also been reported of an extramedullary intradural seat [11].
Nerve sheath myxomas are dermal tumors that usually occur in the upper extremities, the head and neck region [11, 12], and the orthodontic trunk, with a peak incidence in the fourth decade. A study involving a combination of morphological, immunohistochemical, and ultrastructural examinations showed that nerve sheath myxomas are a myxoid variant of schwannoma. Nerve sheath myxoma is diagnosed on the basis of histological structure, and there is no useful antibody for immunohistochemical differentiation between nerve sheath myxoma [4, 8] and conventional schwannoma. Although nerve sheath myxomas are often classified as dermal tumors, some have been reported to occur in the spinal canal [5, 6]. The most common presenting symptoms of a spinal nerve sheath myxoma in adults are sciatic pain, muscle weakness, and paranesthesia [7]. Differential diagnoses on MRI include meningioma, schwannoma, neurofibroma, paraganglioma, and leptomeningeal metastases. As the radiological findings of our case were identical with those of schwannoma, the preoperative diagnosis of nerve sheath myxoma was difficult. It is debatable whether there are any clinicopathological differences between dermal and spinal nerve sheath myxomas. Because a study of the prognosis of dermal nerve sheath myxoma revealed relatively high local recurrence after incomplete resection, careful follow-up was regarded as necessary in our case [9, 10, 11 and 13].
Conclusion
We have reported a rare case of nerve-stem myxoma that arose in unusual locations, i.e., the spinal canal. The tumors arose as intradural extramedullary tumors, and microscopic examination revealed characteristic myxoid lobular structures. Nerve-stem myxomas should be included in the differential diagnosis of spinal canal tumors.
References
- Ariel IM. Tumors of the peripheral nervous system. Semin Surgi Oncol. 1988;4(1):7 12.
- Paulus W, Warmuth-Metz M, Sörensen N. Intracranial neurothekeoma (nerve-sheath myxoma). Case report. J Neurosurgeon. out 1993;79(2):280 2. 3.
- Cohen NA, Samadi DS, Pawel BR, Kazahaya K. Cellular neurothekeoma of the maxilla. Ann Otto Rhino Larnagol. mai 2004;113(5):384 7.
- Goldstein J, Lifshitz T. Myxoma of the nerve sheath. Report of three cases, observations by light and electron microscopy and histochemical analysis. Am J Dermatopathie. oct. 1985;7(5):423 9.
- Paulus W, Jellinger K, Perneczky G. Intraspinal neurothekeoma (nerve sheath myxoma). A report of two cases. Am J Clin Pathol. aver 1991;95(4):511 6.
- Lee D, Suh Y-L, Han J, Kim E-S. Spinal nerve sheath myxoma (neurothekeoma). Pathol Int. mars 2006;56(3):144 9.
- Rickert CH, Schwering E-M, Siebers J, Hartmann C, Von Deimling A, Paulus W. Chromosomal imbalances and NF2 mutational analysis in a series of 10 spinal nerve sheath myxomas. Histopathologies. janv. 2007;50(2):252 7.
- Abul-Kasim K, Thurnher MM, McKeever P, Sundgren PC. Intradural spinal tumors: current classification and MRI features. Neuroradiology. aver 2008;50(4):301 14.
- Struffert T, Grunwald I, Roth C, Reith W. [Spinal intradural tumors]. Radio. déc. 2004;44(12):1211 27; quiz 1228.
- Fletcher CD, Chan JK, McKee PH. Dermal nerve sheath myxoma: a study of three cases. Histopathologies. févr. 1986;10(2):135 45.
- Yamato M, Ikuta H, Hanita J, Iizuka Y, Nakazato Y. Intradural extramedullary spinal nerve sheath myxoma: a report of two cases. Brain Timor Pathol. janv. 2014;31(1):57 61.
- Harkin JC, Reed RJ. Tudors of the périphérie nerves system, editor Rosai J. Atlas of Timor Pathologie Vol 2nd séries Fascicule Washington DC : Armes Forces Institute of Pathologie (1969), p.29-6.
- Fesch JF, Laskine WB, Mettiez M. Nerve Sheth myxome: a clinicopathologic and immunohistochemical analyses of 57 morphologically distinctive. S-100 prottien and GFAP-positive myxine peripherical nerve Sheth tumors with predilection with extremities and high local récurrence rate.Am J Surg Pathol (2005)29: 1615-24.


