Archive : Article / Volume 2, Issue 2
- Case Report | DOI:
- https://doi.org/10.58489/2836-3590/012
Thrombotic Thrombocytopenic Purpura as The Debut of Systemic Lupus Erythematosus
- Argentina, Buenos Aires, BahÃa Blanca, Hospital Interzonal General de Agudos, Servicio de ClÃnica Médica.
Lusich, Brunella
Lusich, Brunella (2023), Thrombotic Thrombocytopenic Purpura as The Debut of Systemic Lupus Erythematosus. Pollution and Effects on Community Health 2(1). DOI: 10.58489/2836-3590/012
© Lusich, Brunella this is an open access article distributed under the Creative Commons attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 24-03-2023
- Accepted Date: 11-04-2023
- Published Date: 14-04-2023
Thrombotic thrombocytopenic purpura- systemic lupus erythematosus- immunomodulators/ immunosuppressants
Abstract
Summary
The association between systemic lupus erythematosus (SLE) and thrombotic thrombocytopenic purpura (TTP) is a described but rare situation and usually occurs in cases with intense lupus activity and renal impairment. It may occur in less than 2% of patients with systemic lupus erythematosus. We present below a case of SLE that abruptly debuts an episode of PTT de aggressive course, treated in an interdisciplinary way with plasma exchanges and immunosuppressants and immunomodulators.
Abstract:
The association between systemic lupus erythematosus Lupus (SEL) and thrombotic thrombocytopenic purpura (TTP) is a described but infrequent situation and usually occurs in cases with intense lupus activity and renal deterioration. This can occur in less than 2% of patients with systemic lupus erythematosus. This association implies an increase in mortality and a longer remission period. We present below a case of SLE that abruptly debuted an episode of TTP with an aggressive course, treated with interdisciplinary treatment with plasma exchanges and with immunosuppressants and immunomodulators.
Introduction
Thrombotic thrombocytopenic purpura (TTP) is a rare disease characterized by episodes of thrombocytopenia and microangiopathic hemolytic anemia due to disseminated microvascular thrombosis. Studies in the 1990s independently demonstrated severe deficiency of a VWF-specific cleavage protease in the plasma of patients with recurrent TTP. This protease was identified as the thirteenth member of the ADAMTS family of metalloproteases (a disintegrant and metalloprotease with repeated thrombospondins 1), ADAMTS13. Severe ADAMTS13 deficiency may be due to mutations in the ADAMTS13 gene (congenital PTT) or anti-ADAMTS13 autoantibodies (autoimmune TTP). Severe antibody-mediated ADAMTS13 deficiency can be detected in most patients with idiopathic TTP (i.e., TTP presenting without associated clinical conditions/events), while its prevalence is much lower in secondary forms of TTP (e.g., associated with pregnancy, infections, autoimmune diseases, and the use of drugs such as ticlopidine and clopidogrel). It should also be mentioned that there are idiopathic cases of TTP with slightly deficient or even normal ADAMTS13 levels at the time of presentation.
Clinical case
A 34-year-old female patient with a history of G2 P1 C1 A0, regular menstrual cycle and aloud contraceptive, who began 15 days ago with joint pain (wrists, ankles and knees) accentuated in the morning, asthenia, holocranial headache (10/10), palpitations and low back pain. Concomitants presented an episode of abundant metrorrhagia. Due to persistence of symptoms, control laboratories are carried out and he goes to the hospital in the area, where they decide on hospitalization with subsequent referral to HIGA Penna.
On admission, the patient presented hemodynamically stable, without oxygen therapy requirements, afebrile, in regular general condition, compound facie, skin with earthy-icteric dye, presented scattered hematomas in lower limbs, right axillary adenomegaly, painless, not adhered to deep planes. Good ventilatory mechanics, regular air intake in left base and bad inlet in right base. Rest of physical examination without particularities.
Studies were received from the guard and in the Medical Clinic room deliverer for the clinical case as the attached laboratories in Table 1 and Table 2, complementary studies were also performed such as abdominal ultrasound, chest x-ray of the forehead and CT of the brain without pathological findings.
He remained hospitalized in Medical Clinic in follow-up in conjunction with Nephrology, Hematology, Infectiology and Rheumatology for thrombocytopenic microangiopathy, thrombotic thrombotic purpura secondary to systemic lupus erythematosus. During hospitalization, antibody sweeping was performed due to underlying pathology and rheumatological p-refill. Finally, but not lastly, ADAMS ANTIBODIES 13 IgG 22 IU/ml (positive >15 IU/ml) were performed. ADAMS 13 activity less than 5 IU/dl (normal: 40-130 IU/dl).
Table 1
Laboratory | Income | Exit |
Hto. Y Hb | 21% and 6 Anisocytosis and megaloblast | 29% and 9.4 |
G. White | 4,200 (17% N 41% L) | 4.910 (87% N y 10% L) |
Platelets | 18.000 | 250.000 |
Coagulograma | TP: 14 (95%)/ KPTT 30.4/ RIN 1.04 |
|
LDH | 872 | 415
|
Ferritina(13-150 ng/ml) | 454 |
|
Dimer D (menor at 250 ng/ml) | 505 |
|
Urea (0.15 - 0.4 g/l) and creatinine (6 - 11 mg/l) | 0.4/7.3 | 0.45/9.2 |
Fibrinógeno (1.8 – 4 g/l) | 3,16 |
|
Direct Coombs | REFUSAL |
|
Table 2
Peripheral blood smear | Reticulocytes 17%, then 1.1% and schytococytes |
Hapetoglobina (30/200 mg/dl) | 5 |
Vitamin B12 (pg/ml) | 448 |
Serologías (HIV/VDRL/TOXO/CMV/EBV/HEPATITIS/PARGOVIRUS B19/CHAGAS/MICOPLASMA) | Negative |
C3(79-172 mg/dl)/C4(16-38 mg/dl)/FR (<20> | 68 / N /16/ - / 1/ 640 + /+ |
Shiga toxin in fecal matter | refusal |
SAF Profile | Negative |
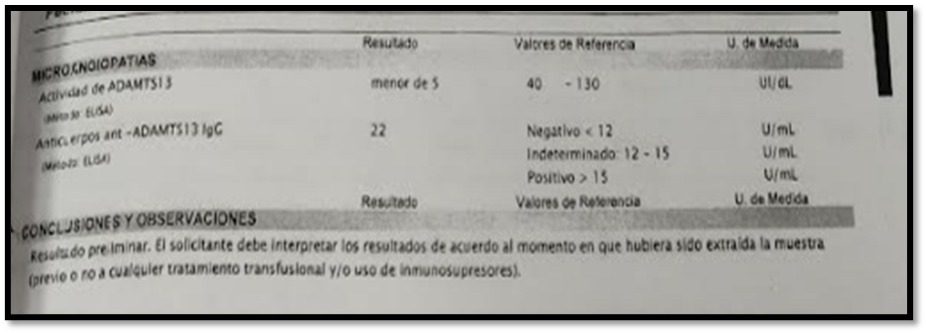
Image 1 (Chest X-rayof Image 2 (CT of the brain without contrast versus without pathological findings) sin findings of bleeding) & Image 3 (ADAMS 13 Result)
Multiple therapeutic behaviors were performed considering the diagnosis of thrombotic thrombocytopenic microangiopathysecondary to SLE with vitamin B12 1 ampoule/24 hours VE. Folic acid mg/day VO. Cook's catheterfor plasmapheresis was placed on the 2nd day of hospitalization (8 cycles in total one per day) with 2,500 ml of fresh frozen plasma exchange. By presenting in the 5th cycle an anaphylactic reaction, it is decided to perform from the 6th cycle without fresh plasma and with albumin solution plasmapheresis. 22days of corticosteroid therapy were performed: 13 days with doses of 40/30mg / day, modified to60 mg / day orally, to date 12 days. Treatment with vitamin D 1 ampoule/month, calcium citrate 1 tablet/day, Trimethoprim/ Sulfamethoxazole 800/160 mg 1 tablet Monday, Wednesday and Friday.
During hospitalization he presented febrile records so cultures were performed with PCR mycoplasma andchlamydia negative and isolated in blood cultures x2 and catheter tip Staphylococcus aureus andempirical treatment was started with vancomycin and then rotatedto cefazolin reported as sensitive in the antibiogram to complete 10 days.A transthoracic echocardiogram was performed to evaluate endocarditis, which gave negative results for vegetation. Also, fundus prior to the start of hydroxychloroquine and rituximab, which reports cataractsin the left eye. He completed2weekly EV doses of Rituximab 675 mg c/24hs and then completed two more cycles in the outpatient clinic. In treatment with hydroxychloroquine 200 mg c / 24 hs VO.
At clinical discharge, outpatient follow-up is performed by Hematology and Rheumatology, who confirm the absence of schistocytes in the peripheral blood smear with remission of the thrombotic thrombocytopenic microangiopathy with control laboratory that highlights Hto: 22 and Hb: 6, platelets: 244,000, GB: 7,300, LDH: 412. Treatment continues with hydroxychloroquine 400 mg/day VO, alendronate 70 mg/week VO, TMS forte Monday, Wednesday and Friday, omeprazole 20 mg/day and future evaluation of rituximab doses.
Discussion
TTP is characterized by microangiopathic hemolytic anemia, thrombocytopenia, fluctuating neurological manifestations, and renal disorders. The occlusion of arterioles and capillaries by microthrombi composed mainly of platelets is typical of this disorder and a consequence of the greater platelet aggregation associated with the presence of large multimers of von Willebrand factor (Vf W), presumably due to the decrease in the activity of the enzyme ADAMTS13, responsible for cleaving these multimers. It has been suggested that the pathogenesis of TTP in SLE could be related to the inhibition of the action of the metalloproteinase ADAMTS13 by autoantibodies but there is no unanimous agreement in this regard.
Many centers describe several different immunosuppressive drugs (corticosteroids, cyclosporine, azathioprine, and, recently, rituximab) to plasma exchange, arguing that these drugs help stop the production of antibodies in autoimmune cases. In addition to these treatments, new drugs have been developed or are in preclinical development for potential use in idiopathic TTP in conjunction with plasma exchange. First, it is possible to reduce or suppress the production of anti-ADAMTS13 autoantibodies with anti-CD20 monoclonal antibodies that target B lymphocytes (e.g., rituximab, but other, more potent compounds are being developed). Second, in principle, it might be possible to restore VWF excision in patients with severe ADAMTS13 deficiency with the use of recombinant ADAMTS13. Third, new compounds have been developed that inhibit the binding of VWF toplatelet glycoprotein Ib-alpha and could block VWF-mediated platelet activation. However, the availability of these new options implies a burden of new challenges for clinicians during an acute episode and in patient subgroups (idiopathic, secondary, TTP with significant renal impairment, etc.). Who could benefit from treatment. All these treatments were used in the patient of the successfully developed case.
Conclusion
As a first conclusion we must establish thatat the epidemiological level, although there are still no official studies, itis estimated that in Argentina it affects 1/2,000 people. Withinthe "Rare diseases": they represent 3.75% of the 8,000 identified by the WHO, this percentage takes greater representativeness since it corresponds to only 0.03% of the population that is estimated affected (8% of the population = to 3.2 million Argentines). According to: Report "Rare Diseases in Argentina", February 2018. On the other hand,TTP may occur in ≤ 2% of patients with SLE. Estimated incidence of 2-10 cases per million inhabitants, with predominance in women in the 3rd and 4th decades of life. The incidence of TTP due to anti-ADAMTS13 autoantibodies is higher in adults (2.9 cases per million/year), more frequently between 18 and 50 years.It should also be noted that it belongsto a Hematological Emergency, with immediate need for high diagnostic clinical suspicion, due to a mortality of 90% if an immediate timely treatment is not started. Finally, it is considered that the treatment with plasma exchanges has greatly improved the prognosis and mortality (90%) has decreased from 85-100% to 10-30% today. However, there are refractory cases and relapses in 40% of patients. Treatment with immunosuppressants, including rituximab (RTX).
References
- G.A. Rock, K.H. Shumak, N.A. Buskard, V.S. Blanchette, J.G. Kelton, R.C. Nair, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. N Engl J Med, 325 (1991), pp. 393-397.
- J. De la Rubia, E. Contreras, J. Del Río-Garma. Thrombotic thrombocytopenic purpura. Med Clin (Barc), 136 (2011), pp. 534-540
- J. Evan Sadler. Thrombotic thrombocytopenic purpura: a moving target. Haematology, (2006), pp. 415-420.
- F. Peyvandi, R. Palla, L.A.Lotta. Pathogenesis and treatment of adquired idiopatic thrombotic thrombocytopenic purpura.Haematologica, 95 (2010), pp. 1444-1447.
- J.N. George. How I treat patients with thrombotic thrombocytopenic purpura. Blood, 116 (2010), pp. 4060-4069 http://dx.doi.org/10.1182/blood-2010-07-271445 |Medline
- D. Caramazza, G. Quintini, I.Abbene, A. Malato, G.Sacullo, L. Lo Coco, et al.Relapsing or refractory idiopathic thrombotic thrombocytopenic purpura-hemolytic uremic syndrome: the role of rituximab.Transfusion, 50 (2010), pp. 2753-2760
- S. Kivity, N. Agmon-Levin. Rituximab for thrombotic thrombocytopenic purpura. Isr Med Assoc J, 13 (2011), pp. 436-437 Medline.
- P. Letchumannan, H.J. Ng, L.H. Lee, J. Thumboo. A comparison of thrombotic thrombocytopenic purpura in an inception cohort of patients with and without systemic lupus erythematosus. Rheumatology, 48 (2009), pp. 399-403
- Y. Fujimura, M. Matsumoto. Registry of 919 patients with thrombotic microangiopathies across Japan: database of Nara Medical University during 1998-2008. Int Med, 49 (2010), pp. 7-15.
- A. Hundae, S. Peskoe, E. Grimsley, S. Patel.Rituximab therapy for refractory thrombotic thrombocytopenic purpura and autoimmune-mediated thrombocytopenia in systemic lupus erythematosus. South Med J, 101 (2008), pp. 943-944
- F.A. Siaz, A.Aleem. Response to rituximab in a refractory case of thrombotic thrombocitopenic purpura associated with systemic lupus erythematosus.Saudi J Kidney Dis Traspl, 21 (2010), pp. 109-112
- Ramirez Duque, J.S. García Morillo, J. Andreu Alvarez, M.L. Martino Galiana. Thrombotic thrombocytopenic purpura, systemic lupus erythematosus, and rescue treatment with cyclophosphamide. Rev Clin Esp, 205 (2005), pp. 518-522.


