Current Issue : Article / Volume 2, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-2292/006
To evaluate health-related quality of life (HRQoL) in Indian patients with COVID-19
Indubhai Patel College of Pharmacy and Research Centre, Dharmaj-388430, Gujarat, India.
Varsha J. Galani
Varsha J. Galani, Niten Patel, (2022). To evaluate health-related quality of life (HRQoL) in Indian patients with COVID-19. Journal of Hospital and Clinical Management. 2(1). DOI: 10.58489/2836-2292/006
© 2022 Varsha J. Galani, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 22-12-2022
- Accepted Date: 26-12-2022
- Published Date: 05-01-2023
respiratory and heart symptoms, neurological symptoms, digestive symptoms, joint or muscle pain, rash and changes in menstrual cycles
Abstract
The Corona virus pandemic caused by severe acute respiratory syndrome coronavirus 2 has infected more than 108 million people in over 150 countries. The vigilance around physical distancing, wearing masks, public health interventions, and social gatherings has eased off, and some countries have been hit by secondand third waves due to their hasty easing off of spatial distancing measures. COVID-19 causes symptoms range from mild to life threatening conditions. Prolonged and sustain symptoms due to COVID-19 are observed not only in high-risk population such as elder patients and individuals with comorbid conditions but also in young adults and individual with no or less chronic disease. People with post COVID-19 are experiencing general symptoms (Tiredness or fatigue that interferes with daily life, post-exertional malaise, fever), respiratory and heart symptoms (shortness of breath, cough, chest pain, fast-beating or pounding heart), neurological symptoms (brain fog, headache, sleep problems, dizziness, pins-and-needles feelings, change in smell or taste, depression or anxiety), digestive symptoms (diarrhea, abdominal pain), joint or muscle pain, rash and changes in menstrual cycles. Chances of multiple organ failure is observed in patients with respiratory symptoms like, interstitial pneumonia and respiratory distress syndrome.
Introduction
The Corona virus pandemic caused by severe acute respiratory syndrome coronavirus 2 has infected more than 108 million people in over 150 countries [1]. The vigilance around physical distancing, wearing masks, public health interventions, and social gatherings has eased off, and some countries have been hit by secondand third waves due to their hasty easing off of spatial distancing measures [2]. COVID-19 causes symptoms range from mild to life threatening conditions [3]. Prolonged and sustain symptoms due to COVID-19 are observed not only in high-risk population such as elder patients and individuals with comorbid conditions but also in young adults and individual with no or less chronic disease [4]. People with post COVID-19 are experiencing general symptoms (Tiredness or fatigue that interferes with daily life, post-exertional malaise, fever), respiratory and heart symptoms (shortness of breath, cough, chest pain, fast-beating or pounding heart), neurological symptoms (brain fog, headache, sleep problems, dizziness, pins-and-needles feelings, change in smell or taste, depression or anxiety), digestive symptoms (diarrhea, abdominal pain), joint or muscle pain, rash and changes in menstrual cycles [5]. Chances of multiple organ failure is observed in patients with respiratory symptoms like, interstitial pneumonia and respiratory distress syndrome [6].
Research of various studies indicated that medical complications were observed as a consequence of COVID-19 and long-term post COVID symptoms were observed in 11%-24% of Covid-19 patients even after three months [6-8]. Post Covid-19 symptoms may lead to very poor health-related quality of life of the patients. Impacts of post COVID illness are not only limit in terms of mortality and morbidity, but also expressed by the subjective measures of health-related quality of life [9]. Health-related quality of life is a multi-dimensional concept that includes domains related to physical, mental, social and emotional functioning [10]. Health-related quality of life (HRQoL) measurement tools like SF-36 (36-item Short-Form Health Survey), SF-6D (Short-Form 6 Dimension) and EQ-5D (Euro-Qol- 5 Dimension) are widely used to assess multi-dimensional domains of the health and well-being of different populations [11].
Research showed that patient isolation, social distancing, use of masks, local lockdown and closing borders had considerably reduced the spread of Covid-19 [12-13]. As a consequence of restriction in COVID-19, impact on economy and education occur with the concomitant loss of the physical and mental health, and quality of life of restricted patients [14-17]. Results of some research on impact of social distancing measures are associated with greater health economic, psychosocial, and physical risk [18-19]. However, data regarding the impact of Covid-19 on health-related quality of life (HRQoL) were scarcely available in the Indian population. Therefore, the aim of the present study was to evaluate HRQoL in Indian COVID-19 patients.
Methodology
This cross-sectional study was conducted in mild to moderate COVID-19 patients. Patients who had been diagnosed with COVID-19 approximately 6 months before the present study were included. According to the patient consent for the response, a total of 100 participants are included in systematic sampling in January 2022.
The EQ-5D-5L questionnaire, along with socio-demographic characteristics, were completed for patients by the telephonic and/ face to face interview after oral consent for participating in the study. Data for the collected health related quality of life is collected using the EQ-5D-5L tool. The first part of EQ-5D-5L divides health into five dimensions: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is divided into five levels; no problem (level 1), slight problem (level 2), moderate problem (level 3), severe problem (level 4), and extreme problem (level 5) [20]. The second part of the EQ-5D is the EQ visual Analogue scale (EQ-VAS) [21].It records the respondent’s self-reported health on a vertical visual analogue scale (VAS), where 0–100 represent the worst and best imaginable health states, respectively [22]. In the telephonic interview, participants were requested to imagine a scale of value zero to one-hundred and to describe their health state with a number between 0 and 100 to get the VAS value. A utility index of one denotes perfect health, and zero represents death. With the use of Indian data set [23], EQ-5D index (Utility index) was calculated. Data was present in the form of frequency and percentage. Mean and Median of EQ-5D-5L index score (Utility index) and VAS score was calculated using Microsoft Excel.
Results
After giving oral consent, total 100 study participants have attempted telephonic and/ face to face interview and responded to the survey.
Demographic characteristics of respondents
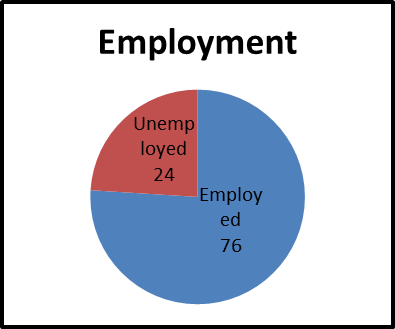
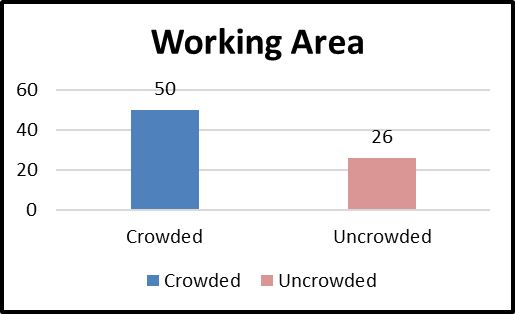
The demographic characteristics of the respondents indicated that 38 respondents were female and 62 were male (Figure 1). Participants were categorised in two age groups one is old age group (>50 years) and the other is adults (<=50 years). As shown in graphical presentation Figure 2, 68 patients had age less than 50 years while 32 patients were belonged to the old age category. Participants were categorised into 2 groups based on their education i) gradute ii) undergraduate. 72 participants were found graduated and 28 had undergraduate study qualifications (Figure 3). The employment ratio had tremendously regressionated in COVID-19 and impact was found in the study data. In the present study, 24% participants were unemployed while 76% had jobs (Figure 4). The working place can have great impact on spread of COVID-19. As shown in Fig. 4.5, 50 out of 76 employed candidates were working in crowded area and this indicated that crowding is a potential threat in spread of COVID-19.



The EuroQol 5-dimensional-5 levels (EQ-5D-5L) questionnaire results
The EQ-5D-5L includes 5 dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression). Each of the dimensions has 5 levels of response options (no problems, slight problems, moderate problems, severe problems, and unable to/extreme problems) to define all possible health states.
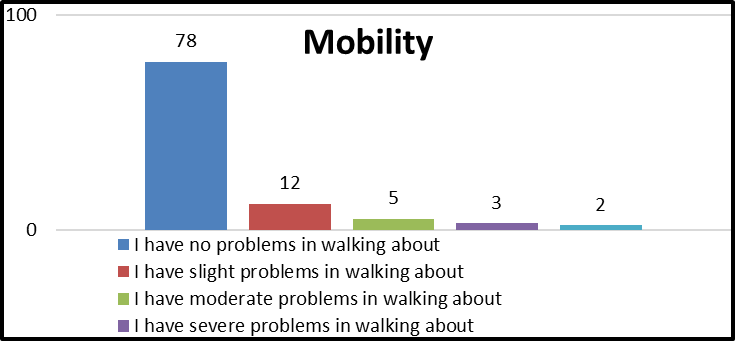
Mobility
As shown in the Figure 6, 78 participants had no problem in walking, 12 had slight problem, 5 participants with moderate and 3 with severe problem in mobility. However, only 2 participants were unable to walk.
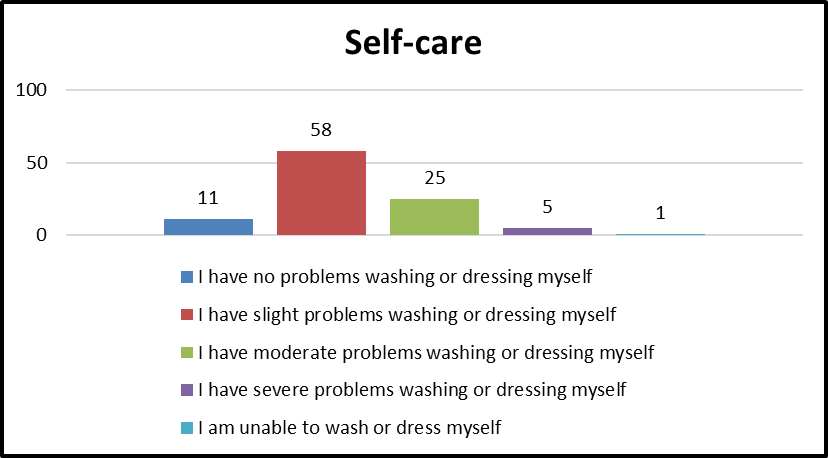
Self-care
As shown in Figure 7, 11 participants had no problems in their self-care in which mainly washing and dressings. Majority of the participant (58) had a slight problem, while 25 participants had moderate problem. Few particiants had problems (5 with severe and 1 with extreme) in their selfcare.
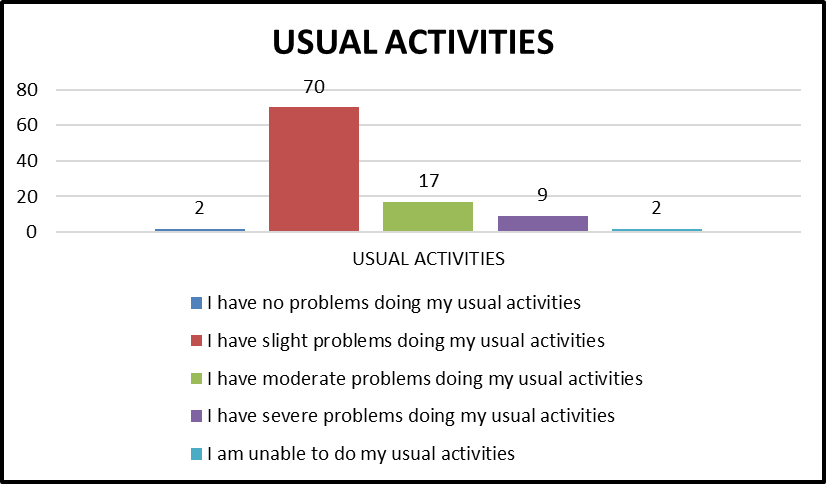
Usual Activities
As shown in the Figure 8, only 2 participants had reported no problems while doing their usual activity. Majority of study participants (70) experienced slight problem in doing their usual activity. 17 participants had moderate problems while few (9) participants had severe problem. Moreover, 2 participants were unable to do their usual activities.
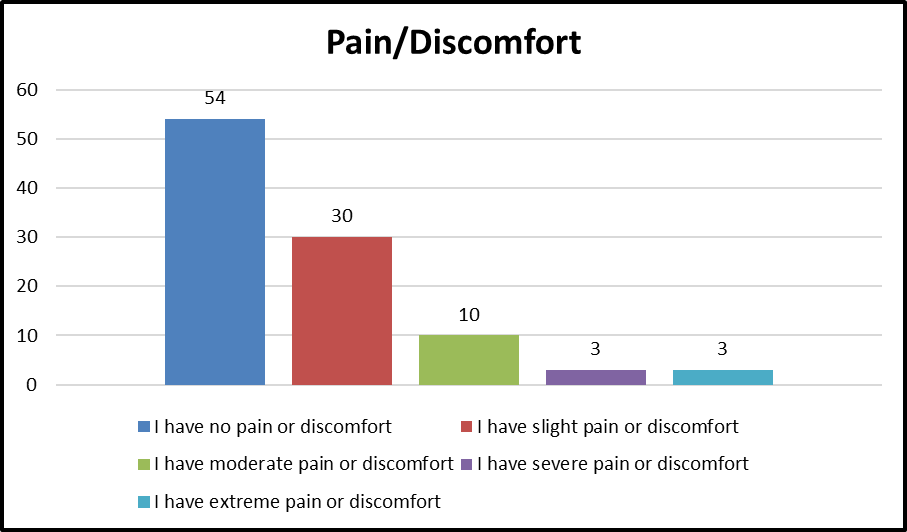
Pain/Discomfort
As shown in the Figure 9, 54 participants had reported no pain or discomfort. 30 participate had reported slight pain, 10 participants with moderate, 3 with severe and 3 with extreme pain were reported.
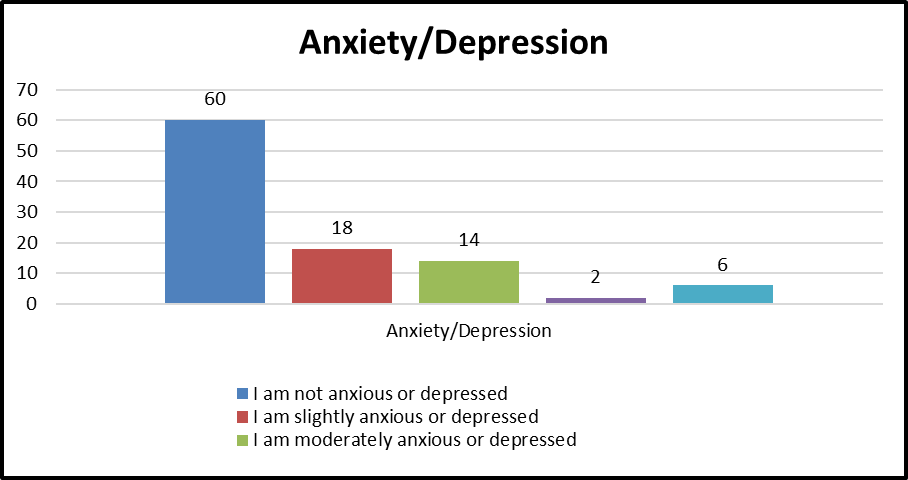
Anxiety/Depression
As shown in the Figure 10, 60 participants showed no symptoms of anxiety or depression. Problem of anxiety and depression was slight in 18 participants. The other participants had moderate, severe, and extreme problem which are 14, 2, and 6 in numbers.
EQ-5D Index Score and VAS Score
A utility index of one denotes perfect health, and zero represents perfect inequality. With the use of Indian data set, EQ-5D index (Utility index) was calculated. Data were present in the form of frequency and percentage. Mean and Median of EQ-5D-5L index score (Utility index) and VAS score was calculated using Microsoft Excel. The average EQ-5D-5L Index score of 100 participants were calculated and found to be 0.734 with median 0.816. The average VAS score was found to be 72.83 with median 80.
Table 1: Result of EQ-5D Index Score and VAS Score
| EQ-5D Index Score (Utility index) | VAS Score |
Mean | 0.734 | 72.83 |
Standard Deviation | 0.23 | 19.4 |
Standard Error of Mean | 0.023 | 1.9 |
Median | 0.816 | 80 |
Discussion
The COVID-19 pandemic has led to a dramatic loss of human life worldwide and presents an unprecedented challenge to public health, food systems and the world of work [24]. The imposition of lockdown or movement restrictions to stop the virus spread has disproportionately affected the population. The impact of the COVID-19 pandemic on health, psychosocial behaviour, lifestyle changes, livelihood, sustainability of quality of life and social and human interactions have been reported worldwide [25-27]. Measures like identification of cases, isolation, quarantine, contact tracing, and community interventions imposed considerable burden on health of people. Standard measure of the quality of health status is a universally accepted and the comparable outcome tool require to describe the health of the population affected by COVID-19 and would be of immense value. Health-related quality of life refers to the impact of disease and treatment on patients’ function and overall life satisfaction [28]. Clinicians and policymakers are recognizing the importance of measuring health-related quality of life (HRQL) to inform patient management and policy decisions [29].
The EQ-5D-5L questionnaire is a five level five-dimensional (mobility, selfcare, usual activities, pain/discomfort, and anxiety/depression) preference-based tool for the observation and quantification of HRQoL. The majority of the Covid-19 cases in the present study were male (62%) and less than 50 years of age (68%). In the present study, data were collected and EuroQol utility index value was calculated as per Indian data set [23] for COVID-19 recovered Indian population after 6 months of confirmation of COVID-19. Index score value 0 denote for the death and 1 for the perfect health while negative value indicates life worse than death [30,31]. In the present study, the mean EQ-5D index score among COVID-19 patients on 6 months after discharge was 0.734 (SD = 0.228). This means that patients who suffered from COVID-19 lost an average of 26.6% of their HRQoL. This finding is similar to a study in Iran that reports an EQ-5D index score of 0.612 [32] and a Belgian study with an EQ-5D index score of 0.620 [33], but our findings are substantially lower than those of studies from Norway (EQ-5D index score: 0.820) [34], China (EQ-5D index score: 0.949) and Hong Kong (EQ-5D index score: 0.897). [35,36]. Variations in the HRQOL evaluation method employed (i.e., health utility tariff, tools, scale, study participant sampling) may also, to some extent, contribute to the discrepancy. Visual Analog Scale (VAS) is a most widely used simple and practical approach to elicit patient health value functions, through evaluating their own health-related quality of life [37-39]. The overall mean VAS score was 72.83 (median = 80) in our study. This was similar with study from Egypt (72.2) [35], Peru (76) [36], Spain (66.36) [32], China (85.52) [35]. and Addis Ababa, Ethiopia (69.44)[40].
However, our study has some limitations. First, because the study collected HRQoL data based on patient preferences, the patients might over or underestimated their health status during the interview. Moreover, due to the study’s cross-sectional design, we could not compare the HRQoL of patients before the Covid-19 infection.
Conclusion
The Covid-19 disease substantially impaired the HRQoL of Indian patients for a sustained period. Therefore, close clinical follow up and psychological treatment should be encouraged. This study helps policymakers and other authorities to develop policy for overcoming issues affecting quality of life of Covid-19 patients.
References
- World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. Available from: https://covid19.who.int. (Accessed on 15 Feb2021).
- Han E, Tan MMJ, Turk E, Sridhar D, Leung GM, Shibuya K, Asgari N, Oh J, García-Basteiro AL, Hanefeld J, Cook AR, Hsu LY, Teo YY, Heymann D, Clark H, McKee M, Legido-Quigley H. Lessons learnt from easing COVID-19 restrictions: An Analysis of countries and regions in Asia Pacific and Europe. Lancet, 396: 1525-1534.
- Kakodkar P, Kaka N, Baig M. A comprehensive literature review on the clinical presentation, and management of the pandemic coronavirus disease 2019 (COVID-19). Cureus, 2020;12(4): e7560.
- Tenforde MW, Kim SS, Lindsell CJ, Rose EB, Shapiro NI, Files DC, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with COVID-19 in a multistate health care systems network—United States, March–June 2020. Morb Mortal Wkly Rep, 2020; 69 (30):993.
- Centres for Disease Control and Prevention. Long COVID or Post-COVID Conditions. Available at https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html (Accessed on 15 Feb2021)
- World Health Organisation. What we know about Long-term effects of COVID-19 (coronavirus update 36). 2020. Available at https://www.who.int/publications/m/item/update-36-long-term-effects-of-covid-19.
- Ding H, Yin S, Cheng Y, Cai Y, Huang W, Deng W. Neurologic manifestations of nonhospitalized patients with COVID-19 in Wuhan, China. Med Comm, 2020;1(2):253-256.
- Cirulli E, Barrett KMS, Riffle S, Bolze A, Neveux I, Dabe S, Grzymski JJ. Long-term COVID-19 symptoms in a large unselected population. Medrxiv, 2020 https://doi.org/10.1101/2020.10.07.20208702.
- Guo L, Lin J, Ying W, Zheng C, Tao L, Ying B, Cheng B, Jin S, Hu B. Correlation study of short-term mental health in patients discharged after coronavirus disease 2019 (COVID-19) infection without comorbidities: A prospective study. Neuropsychiatr Dis Treat, 2020;16:2661-2667.
- Office of Disease Prevention and Health Promotion (ODPHP). Health-related quality of life and well- being. 2020. Available at https://www.healthypeople.gov/2020/about/foundation-health-measures/Health-Related- Quality-of-Life-and-Well-Being.
- Pequeno NPF, Cabral NLA, Marchioni DM, Lima SCVC, Lyra CO. Quality of life assessment instruments for adults: a systematic review of population-based studies. Health Qual Life Outcomes, 2020;18(1):208.
- Courtemanche C, Garuccio J, Le A, Pinkston J, Yelowitz A. Strong Social Distancing Measures in The United States Reduced The COVID-19 Growth Rate. Health Aff (Millwood), 2020;39(7):1237-1246.
- Qian M, Jiang J. COVID-19 and social distancing. Z Gesundh Wiss, 2022;30(1):259-261.
- de Matos DG, Aidar FJ, Almeida-Neto PFd, Moreira OC, Souza RFd, Marçal AC, Marcucci-Barbosa LS, Martins Júnior FdA, Lobo LF, dos Santos JL, Guerra I, Costa e Silva AdA, Neves EB, Tinoco Cabral BGdA, Reis VM, Nunes-Silva A. The Impact of measures recommended by the government to limit the spread of Coronavirus (COVID-19) on physical activity levels, quality of life, and mental health of Brazilians. Sustainability, 2020;12(21):9072.
- Samrah SM, Al-Mistarehi AH, Aleshawi AJ, Khasawneh AG, Momany SM, Momany BS, Abu Za'nouneh FJ, Keelani T, Alshorman A, Khassawneh BY. Depression and coping among COVID-19-infected individuals after 10 days of mandatory in-hospital quarantine, Irbid, Jordan. Psychol Res Behav Manag, 2020;13:823-830.
- Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, Pham LV, Tran KV, Duong TT, Tran TV, Duong TH, Nguyen TT, Nguyen QH, Hoang TM, Nguyen KT, Pham TTM, Yang SH, Chao JC, Duong TV. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: The potential benefit of health literacy. J Clin Med, 2020;9(4):965.
- Tran BX, Nguyen HT, Le HT, Latkin CA, Pham HQ, Vu LG, Le XTT, Nguyen TT, Pham QT, Ta NTK, Nguyen QT, Ho CSH, Ho RCM. Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. Front Psychol, 2020;11:565153.
- Tull MT, Edmonds KA, Scamaldo KM, Richmond JR, Rose JP, Gratz KL. Psychological outcomes associated with stay-at-home orders and the perceived impact of COVID-19 on daily life. Psychiatry Res, 2020;289:113098.
- Hamadani JD, Hasan MI, Baldi AJ, Hossain SJ, Shiraji S, Bhuiyan MSA, Mehrin SF, Fisher J, Tofail F, Tipu SMMU, Grantham-McGregor S, Biggs BA, Braat S, Pasricha SR. Immediate impact of stay-at-home orders to control COVID-19 transmission on socioeconomic conditions, food insecurity, mental health, and intimate partner violence in Bangladeshi women and their families: an interrupted time series. Lancet Glob Health, 2020;8(11):e1380-e1389.
- Whitehead SJ, Ali S. Health outcomes in economic evaluation: the QALY and utilities. Br Med Bull, 2010;96:5-21
- Emrani Z, Akbari Sari A, Zeraati H, Olyaeemanesh A, Daroudi R. Health-related quality of life measured using the EQ-5D-5 L: population norms for the capital of Iran. Health Qual Life Outcomes, 2020;18(1):108.
- Yin S, Njai R, Barker L, Siegel PZ, Liao Y. Summarizing health-related quality of life (HRQOL): development and testing of a one-factor model. Popul Health Metr, 2016;14:22.
- Computing EQ-5D-5L index values with SPSS using the Indian (Jyani et al) value set Version 1.1 (Updated 05/01/2022) Available on http:/euroqol.org /wp-content/uploads/2022/03/India_valaue_SPSS.txt. (accessed 21 April 2022)
- Joint statement by ILO, FAO, IFAD and WHO. Impact of COVID-19 on people's livelihoods, their health and our food systems. 13 October 2020 https://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people%27s-livelihoods-their-health-and-our-food-systems
- Azizi A, Achak D, Aboudi K, Saad E, Nejjari C, Nouira Y, Hilali A, Youlyouz-Marfak I, Marfak A. Health-related quality of life and behavior-related lifestyle changes due to the COVID-19 home confinement: Dataset from a Moroccan sample. Data Brief, 2020;32:106239.
- Qu G, Zhen Q, Wang W, Fan S, Wu Q, Zhang C, Li B, Liu G, Yu Y, Li Y, Yong L, Lu B, Ding Z, Ge H, Mao Y, Chen W, Xu Q, Zhang R, Cao L, Chen S, Li H, Zhang H, Hu X, Zhang J, Wang Y, Zhang H, Liang C, Sun L, Sun Y. Health-related quality of life of COVID-19 patients after discharge: A multicenter follow-up study. J Clin Nurs, 2021;30(11-12):1742-1750.
- El Keshky MES, Basyouni SS, Al Sabban AM. Getting Through COVID-19: The Pandemic's Impact on the Psychology of Sustainability, Quality of Life, and the Global Economy - A Systematic Review. Front Psychol, 2020;11:585897.
- Kharshiing KD, Kashyap D, Gupta K, Khursheed M, Shahnawaz MG, Khan NH, Uniyal R, Rehman U. Quality of Life in the COVID-19 Pandemic in India: Exploring the Role of Individual and Group Variables. Community Ment Health J, 2021;57(1):70-78.
- Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med, 1993 Apr 15;118(8):622-9.
- Herdman M, Gudex C, Lloyd A, Janssen M, Kind P, Parkin D, Bonsel G, Badia X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual Life Res, 2011;20(10):1727-36.
- McCaffrey N, Kaambwa B, Currow DC, Ratcliffe J. Health-related quality of life measured using the EQ-5D-5L: South Australian population norms. Health Qual Life Outcomes, 2016;14(1):133.
- Arab-Zozani M, Hashemi F, Safari H, Yousefi M, Ameri H. Health-related quality of life and its associated factors in COVID-19 patients. Osong Public Health Res Perspect, 2020;11(5):296-302.
- Meys R, Delbressine JM, Goërtz YMJ, Vaes AW, Machado FVC, Van Herck M, Burtin C, Posthuma R, Spaetgens B, Franssen FME, Spies Y, Vijlbrief H, Van't Hul AJ, Janssen DJA, Spruit MA, Houben-Wilke S. Generic and respiratory-specific quality of life in non-hospitalized patients with COVID-19. J Clin Med, 2020;9(12):3993.
- Garratt AM, Ghanima W, Einvik G, Stavem K. Quality of life after COVID-19 without hospitalisation: Good overall, but reduced in some dimensions. J Infect, 2021;82(5):186-230.
- Ping W, Zheng J, Niu X, Guo C, Zhang J, Yang H, Shi Y. Evaluation of health-related quality of life using EQ-5D in China during the COVID-19 pandemic. PLoS, One 2020;15(6):e0234850.
- Wong EL, Ho KF, Wong SY, Cheung AW, Yau PS, Dong D, Yeoh EK. Views on Workplace Policies and its Impact on Health-Related Quality of Life During Coronavirus Disease (COVID-19) Pandemic: Cross-Sectional Survey of Employees. Int J Health Policy Manag, 2022 Mar 1;11(3):344-353.
- Lundberg L, Johannesson M, Isacson DGL, Borgquist L: Health state utilities in a general population in relation to age, gender and socioeconomic factors. Eur J Pub Health, 1999, 9:211-217.
- Shmueli A: Subjective health status and health values in the general population. Med Decis Making, 1999, 19:122-127.
- EuroQol–A new facility for the measurement of health-related quality of life. The EuroQol Group. Health Policy 1990, 16:199-208.
- Kastien-Hilka T, Rosenkranz B, Sinanovic E, Bennett B, Schwenkglenks M. Health-related quality of life in South African patients with pulmonary tuberculosis. PLoS, One 2017 ;12(4): e0174605.


