Archive : Article / Volume 1, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-5127/001
Ultrasound Tomography (3D) Triage for Oculofacial emergencies- new paradigms
Casey Eye Institute, Oregon Health & Science University, Portland, Oregon, 97239, USA.
Hadi Khazaei
Hadi Khazaei, Danesh Khazaei (2022). Ultrasound Tomography (3D) Triage for Oculofacial emergencies- new paradigms. Journal of Radiology Research and Diagnostic Imaging. 1(1). DOI: 10.58489/2836-5127/001.
© 2022, Hadi Khazaei, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 12-09-2022
- Accepted Date: 27-09-2022
- Published Date: 03-11-2022
Ocular Ultrasonography, Ocular trauma, Ocular Triage, Ocular emergencies
Abstract
Background: The incidence of ocular trauma has been on the rise for the past few years. This impels the medical community to be more adroit at diagnosing and treating these injuries. An effective way to diagnose different manifestations of ocular trauma involve the use of ultrasound to visualize the anatomical details of the eye and orbit, which is vital for deciding the best management plan.
Aim: To assess the suitability of 3D Ultrasound as a first-line investigation for oculofacial emergencies resulting from projectile and blast injuries.
Methods: In this review article, the focus of discussion will be the accuracy of 3D ultrasound in diagnosing oculofacial injuries and the utility of ultrasound in triage of vision threatening emergencies in austere environments.
Results: Understanding the utility of ultrasound data for diagnosis will assist ophthalmologists in managing ocular trauma more effectively.
Conclusion: We recommend that patients with suspected eye injuries should undergo careful 3D ultrasound examination by appropriately trained ophthalmologists as a part of triage for oculofacial emergencies in austere environments.
Abbreviations
1- USCT (Ultrasound Computer Tomography)
2- ED (Emergency Department)
3- IED (improvised explosive device)
4- CT/MRI (Computed Tomography/ Magnetic Resonance Imaging)
5- BETT (Birmingham Eye Trauma Terminology)
6- OTS (Ocular Trauma Score)
Introduction
The incidence of ocular trauma has been on the rise for the past few years, afflicting more than 28% of blast survivors. Ocular injuries now account for 13% of all battlefield injuries and are the fourth most common military deployment-related injury [1].3D ultrasonography in the ambulatory and critical care setting has become an invaluable diagnostic tool for patients presenting with traumatic or atraumatic vision loss and ocular complaints. In properly trained ophthalmologist, sonographic bedside evaluation is intuitive, easy to perform, and can accurately diagnose a variety of pathologies. These include detachment or hemorrhage of the retina, choroid or vitreous, lens dislocation, or subluxation, globe rupture or scalopetaria retinae, commotio retinae, retrobulbar hematoma, ocular and orbital foreign bodies, infections, cellulitis, inflammation, tumors, orbital compartment syndrome and increased optic nerve sheath diameter that can be assessed in the setting of suspected increased intracranial pressure and many more conditions. The ocular anatomy is easy to visualize with sonography, however, orbital ultrasound remains a challenge. Over the last two decades, a large number of scientific publications have documented that 3D ultrasound in emergent or critical care settings are an accurate diagnostic tool and expands and improves emergency diagnosis and management [2].
Ocular ultrasonography is still an underutilized tool in the emergency setting. Ultrasound is generally thought to be sensitive for diagnosis in the presence of intraocular penetrating foreign bodies, but is considered a specialist driven investigation (2). CT or plain orbital X ray views are often employed instead, especially if craniofacial or brain injuries are also suspected [3]. CT scan and X ray images are sensitive to metallic foreign bodies, but in the context of an improvised explosive device (IED) injury, they may be less so [4]. A non-metallic penetrating foreign body is relatively uncommon outside this arena but does still occur.
The findings are relevant wherever access to a surgical center is difficult, or in cases where CT scanners are not available [5]. Also, there is a concern that probe pressure on an open globe could extrude the ocular contents. Use of a thick layer of an ultrasonically visible gel between the probe and the eyelid can allow for high quality image acquisition while avoiding any pressure on the globe when performed by an appropriately trained ophthalmologist [6-8]. Despite these limitations, there is no doubt that ultrasound shows promise in the assessment of the blast-injured globe. In the military context, where standard assessment may be difficult and dangerous, it may provide a useful triage tool [9].
Material and Methods
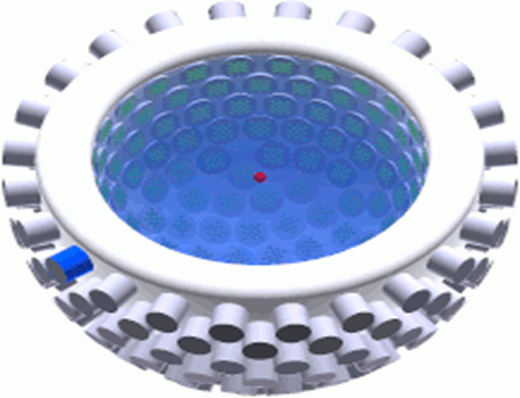
Ultrasound tomography (3D) use ultrasound waves for creating images. In the first measurement step a defined ultrasound wave is generated with typically Piezoelectric ultrasound transducers, transmitted in direction of the measurement object and received with other or the same ultrasound transducers. While traversing and interacting with the tissue, the ultrasound wave is changed and carries now information about the target. After being recorded the information from the modulated waves can be extracted and used to create an image of the object in a second step. Also, they are fast in data taking as they don't require time-costly mechanical movements. Unlike X-ray or other physical properties which provide typically only one information, ultrasound provides multiple information of the object for imaging: the attenuation the wave's sound pressure experiences indicate on the object's attenuation coefficient, the time-of-flight of the wave gives speed of sound information, and the scattered wave indicates on the echogenicity of the object (e.g. refraction index, surface morphology, etc.). Unlike conventional ultrasound sonography, which uses phased array technology for beamforming, most USCT systems utilize unfocused spherical waves for imaging. Most USCT systems aiming for 3D-imaging, either by synthesizing ("stacking") 2D images or by full 3D aperture setups. Another aim is quantitative imaging instead of only qualitative imaging (Figure 1).
Results
Ultrasound has found limited acceptance in the emergency department, despite studies showing its value for the diagnosis of globe rupture, vitreous hemorrhages, retinal detachments, retrobulbar hemorrhages [9] and raised intracranial pressure [10] . In penetrating injury, in particular, this may be due to concerns about pressure on an open globe causing further damage. An important note is that the technique must be carried out only by an eye professional” in such a way that no pressure is being applied on the globe at any time.
Many smaller medical units providing the initial management of eye casualties have no CT or MRI facilities. Injured military personnel are transferred to local emergency units whenever the infrastructure can permit. It is therefore essential that potential eye injuries are identified early so appropriate transfers can be arranged. Urgent evacuation must be reserved for those most likely to be cured when diagnosed by advanced eye care.
Blast injuries generally are categorized according to the interaction of the body with the shock wave (primary), energized particulate matter (secondary), blast wind (tertiary, includes bodily displacement and structural effects), and other effects (quaternary) [11]. Although the prognosis for visual recovery in penetrating eye trauma is poor, anatomical structures can be preserved if the retained foreign body fragment is extracted [12–14]. Also, a subgroup of patients those cannot comply with visual assessment (e.g., intubated in intensive care) and have injuries associated with ocular blast injury (e.g., penetrating eyelid injuries and orbital injuries) but no overt globe injury needs to be triaged for transfer to advance surgical facilities immediately.
Although case studies have long implicated primary blast in ocular trauma, very few experimental data have been collected to document this phenomenon. In those studies, empirical ballistic imaging and computational modeling confirm such injury was associated with globe distortion and postimpact pressure oscillations. 3D ultrasound offers a sensitive screening tool for a penetrating foreign body, or blast injury to the globe. 3D Orbital ultrasonography may provide a tool for this triage [15].
Ultrasound tomography (3D) may even be more sensitive than a CT scan in cases of non- metallic foreign bodies or traumatic optic neuropathy. 3D ultrasound is portable, economical, and easy to interpret by trained ophthalmologists. Careful assessment in selected cases allows a high-yield, low-risk examination [16].
Discussion
We are planning to investigate and validate the use of USCT method for oculofacial emergencies. This method will include a broad array of oculofacial injuries that would seriously compromise visual function.
Reimaging using 3D ultrasound allows to investigate the course of treatments and visual outcome. A notable strength of this study is the evaluation of the blast injuries with the complimentary methods, including 3D scan, CT/MRI scan, gross dissection, and histopathology if deemed necessary.
Current ocular trauma scores, like the ‘Birmingham Eye Trauma Terminology" (BETT) [17] or the "Ocular Trauma Score" (OTS) [18] subdivide open globe injuries between lacerations and ruptures, while subdividing closed globe injuries between contusions and lamellar lacerations. There is a need for the development of a universal parlance in describing blast-related ocular injuries. Such a scale must account for the full range of ocular injuries extending from the subtle, closed-globe nature of primary blast injuries observed here up to and including globe rupture.
The practical application of these new findings will require a meaningful composite scoring algorithm for severity of injury. Scaled algorithms for the severity of the damage to the individual component tissues of the eye and the classic anatomic subsections of the eye have been devised for forthcoming analyses of the association of blast overpressure with the extent of ocular injury. Ultimately, it will be necessary to collate these individual focal injury data into a proposed clinically relevant Composite Injury Scale that addresses the practical needs of those engaged in the treatment of ocular injury or development of protective eyewear (Table 1) [19].
Continued experimentation in this area will allow more robust correlation between the blast wave characteristics and frequency of trauma response. Ultimately, a probabilistic regression model predicting the likelihood of a specific type of injury similar to the Bowen curves could be combined with data from novel battlefield pressure sensors to enable informed treatment by medical staff [19].
| TABLE 1. Composite Injury scoring system |
0 The eye is undamaged 1 The eye has some damage, but should heal fully on its own 2 The eye has damage that will require surgery to repair, leaving chronic pathology 3 The eye has damage that might be repairable with surgery, with severe visual loss 4 The eye is likely damaged beyond meaningful functional repair |
Conclusions
It is apparent from the present study that primary blast overpressure can produce injuries that conform to each of these proposed categories. For example, many of the isolated smaller peripheral choroidal detachments would be Category 1 injuries. Many of the isolated angle recession injuries would lead to chronic glaucoma, requiring filtering or tube shunt surgery (Category 2). The posterior peripapillary stellate retinal detachments would all require timely vitreoretinal surgical intervention to avert blindness, with inevitable functional loss in even the most successful cases (Category 3).
Eyes with extensive peripapillary axonal rupture would be expected to develop blinding levels of traumatic optic neuropathy unlikely to respond sufficiently to any current therapy to avert functional blindness in the affected eye (Category 4). When injuries to multiple ocular tissues coexist, the likelihood of therapeutic failure increases: therefore, the integration of the focal and composite injury scales would tend to elevate an eye with multiple Category 2 injuries to Category 3, and any combination of Categories 3 and 2 injuries to Category 4.
Declaration of Helsinki
This review is adhered to the ethical principles outlined in the Declaration of Helsinki as amended in 2013. (https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/).
Funding
None
Conflict of interest
None
Authors’ contribution Acknowledgement
All the concerned authors jointly edited and approved the final manuscript.
References
- Morley MG, Nguyen JK, Heier JS, Shingleton BJ, Pasternak JF, Bower KS. (2010), Blast eye injuries: a review for first responders. Disaster Med Public Health Prep. 4:154–160.
- Khazaei H, Khazaei D, Ashraf D, Mikkilineni S, Ng JD. (2022), Overview of Orbital Ultrasonography. Ann Ophthalmol Vis Sci. 5(1): 1028.
- Arey ML, Mootha VV, Whittemore AR, Chason DP, Blomquist PH. (2007), Computed tomography in the diagnosis of occult open globe injuries. Ophthalmology; 114: 1448–52.
- Turkcuer I, Atilla R, Topacoglu H, et al: (2006), Do we really need plain and soft-tissue radiographies to detect radiolucent foreign bodies in the IED. Am J Emerg Med; 24(7): 763–8.
- Bray PW, Mahoney JL, Campbell JP: (1995), Sensitivity and specificity of ultrasound in the diagnosis of foreign bodies in the hand. J Hand Surg Am; 20(4): 661–6.
- Oikarinen KS, Nieminen TM, Makkarainen H, Pyhtinen J: (1993), Visibility of foreign bodies in soft tissue in plain radiographs, computed tomography, magnetic resonance imaging and ultrasound. An in vitro study. Int J Oral Maxillofac Surg; 22(2): 119–24.
- Aras MH, Miloglu O, Barutcugil C, Kantarci M, Ozcan E, Harorli A: (2010), Comparison of the sensitivity for detecting foreign bodies among conventional plain radiography, computed tomography and ultrasonography. Dentomaxillofac radiol; 39(2): 72–
- Blaivas M, Theodoro D, Sierzenski P: (2002), ocular ultrasonography in the emergency department. Acad Emerg Med; 9: 791–
- Blaivas M: (2000), Bedside emergency department ultrasonography in ocular pathology. Acad Emerg Med; 7(8): 947–50.
- Soldatos T, Chatzimichail K, Papathanasiou M, Gouliamos A: (2009), Optic nerve sonography: a new window for the non-invasive evaluation of intracranial pressure in brain injury. Emerg Med J; 26:630–4.
- Garner JP, Brett SJ. (2007), Mechanisms of injury by explosive devices. Anesthesiol Clinic North Am. 25:147–160.
- Weichel ED, Colver MH: (2008), Combat ocular trauma and systemic injury. Curr Opin Opthalmol; 19(6): 519–25.
- Colyer MH, Chun DW, Bower KS, Dick JS, Weichel ED: (2008), Perforating globe injuries during operation Iraqi Freedom. Ophthalmology; 115(11): 2087–93.
- Colyer MH, Weber ED, Weichel ED, et al: (2007), Delayed intraocular foreign body removal without endophthalmitis during operations Iraqi Freedom and Enduring freedom. Ophthalmology; 114: 1439–47.
- Sawyer N: (2009), Ultrasound imaging of penetrating ocular trauma. J Emerg Med; 36(2): 181–2.
- Khazaei H, Khazaei D, Brundage D, Mikkilineni S, Dailey A. (2022), “Facial Ultrasonography in acquired facial lipoatrophy” Inter J. Research and Scientific Innovation (IJRSI) vol.9 issue5, pp.48-51 May DOI: https://dx.doi.org/10.51244/IJRSI.2022.9504
- Kuhn F, Morris F, Witherspoon CD, Mester V. (2004), Birmingham Eye Trauma Terminology / J Fr Ophthalmol. 27:206–210.
- Kuhn F, Masisiak R, Mann L, Mester V, Morris R, Witherspoon D. (2002), OTS. Ophthalmol Clin N Am. 15:163–165.
- Daniel Sherwood, William E. Sponsel, Brian J. Lund, Walt Gray, Richard Watson et al; (2014), Anatomical Manifestations of Primary Blast Ocular Trauma Observed in a Postmortem Porcine Model. Invest. Ophthalmol. Vis. Sci.;55(2):1124-1132
- Khazaei H, Khazaei D, Ashraf D, Mikkilineni S, Ng JD. (2022), Ultrasonographic Characteristics of the Facial Nerve in Patient with Bell’s Palsy. Ann Ophthalmol Vis Sci. 5(1):1029.


