Case Report | DOI: https://doi.org/10.58489/2836-497X/013
Utero-Vesical Fistula Closure After 3 Weeks Treatment with Intravenous Mesenchymal Stem Cells Infusion: Case Report
- Di Silvio Mauricio 1,2,3
- Luján-Irastorza Jesús Estuardo 1,2
- Durand-Montaño Carlos 1
- Henández-Ramos Roberto 1
- Barrón-Vallejo Jesús 1
- Ávila-Rebollar Daniela 1
- Myslabodski Julio 8
- Pariente-Fernández Maruxa 1,2
- Tagle-Rodríguez Jorge Mario 4
- Ramírez-Amezcua Miguel Ángel 4
- Paredes-Núñez María Angélica 1,2
- Vargas-Hernández Víctor Manuel 1,5
1 Hospital Bité Médica, Mexico City. México.
2 Clínica Helix, México City. México.
3 Hospital MAC Periférico Sur, México City. México.
4 Instituto de Terapia Celular (ITC), Guadalajara, Jalisco. México.
5 National Academy of Medicine México.
6 Mexican Academy of Surgery. México.
7 American College of Surgeons, International Fellow. USA.
8 Banco de Cordon Umbilical (BCU).
*Corresponding Author: Vargas-Hernández Víctor Manuel*
Citation: Di Silvio Mauricio, Luján-Irastorza Jesús Estuardo, Durand-Montaño Carlos, Henández-Ramos Roberto, Barrón-Vallejo Jesús, et.al., (2023). Utero-Vesical Fistula Closure After 3 Weeks Treatment with Intravenous Mesenchymal Stem Cells Infusion: Case Report. Archives of Gynaecology and Women Health.2(1). DOI: 10.58489/2836-497X/013
Copyright: © 2023 Vargas-Hernández Víctor Manuel, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received: 24 January 2023 | Accepted: 22 February 2023 | Published: 21 April 2023
Keywords: Utero-Vesical Fistula , intravenous, Adipose tissue Mesenchymal Stem Cells , Computarized Tomography Cystography
Abstract
Objective: To describe the evolution of Utero-Vesical Fistula (UVF) of one patient who received conservative treatment using intravenous (IV) infusion of 120x106 Adipose tissue Mesenchymal Stem Cells (ADMSCs).
Clinical case report
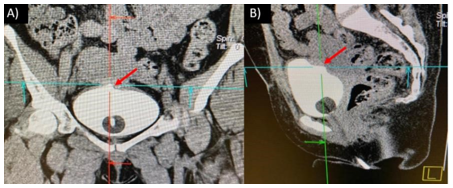
A 36-year-old female presented with post-cesarean hematuria 3 hours after an emergency c-section was performed consequently to placental abruption during labour. The primary measure was to use a transurethral Silastic 18F Foley catheter to prevent bladder expansion. The catheter remained for 21 days. Evaluation through Computarized Tomography Cystography (Cisto-CAT) revealed failure to close the fistula. The decision to inject ADMSCs as an IV single dose was done. Three weeks after this intervention no blood was seen in the urine drainage bag. Complete resolution of UVF was confirmed with a control CT urogram.
Result:
Total closure of UVF.
Conclusions:
The IV infusion of ADMSCs proved to be a plausible and effective conservative treatment of UVF.
Introduction
An abnormal communication between uterus and urinary bladder, related with surgical trauma may result in Utero-Vesical Fistula (UVF) formation. The primary symptom of patients with these fistulas is usually urinary incontinence. However, patients may present with cyclic hematuria and amenorrhea. They represent 0.5 to 10% of all urogenital fistulae. Currently, its prevalence is higher due to the increase in cesarean sections [1, 2]. UVF can have several etiologies: 1) Obstetric causes: prolonged labor, cesarean section/hysterectomy, instrumental maneuver during childbirth, traditional practices, embryotomy in abortions and symphysiotomy, 2) non-obstetric causes: trauma (intercourse, sexual violence, accident and sexual mutilation); infections (tuberculous granulomatous and HIV); as well as: pelvic surgery, radiotherapy and tumors [1, 3].
The main sign of UVF is urine loss and can be confirmed through vaginal hysterosonography with cervical instillation of methylene blue. In recent years, cystography with computerized axial tomography (Cisto-CAT) is also used [2, 4].
Currently, the treatment of UVF can be done conservatively. After a cesarean section or other pelvic intervention, prolonged bladder catheterization is used for 4 to 6 weeks in order to allow the injured area to heal [3]. If the fistula is already formed, tube therapy offers little chance of spontaneous closure and instead increases inflammation and the risk of infection [3]. Despite the fact that in many cases the fistulas are already formed, doctors rather choose conservative treatment over surgical treatment [3]. The main reasons are the complications that may arise as a consequence of surgical repair (infections or urinary incontinence) and the complexity of the recovery process. As a consequence of this, less invasive alternatives are being sought in order to improve the success rates of UVF repair. Mesenchymal Stem Cells (MSCs) are being proposed in a diversity of studies as an alternative treatment [5, 6]. Due to their high proliferation rate, regeneration capacity and their increased capability of cell differentiation into different cell types through asymmetric divisions [7, 8]. Adipose tissue Mesenchymal Stem Cells (ADMSCs) have been considered, in recent years, as an innovative option to be used in regenerative medicine. ADMSCs are obtained from embryonic and extra-embryonic tissue, as well as from adult organs such as: bone marrow, peripheral blood, umbilical cord, and adipose tissue, among others. In addition, they can be autologous or donor (allogeneic). Its application —in clinical research— has been carried out as cell therapy for degenerative diseases such as Alzheimer's, Amyotrophic Lateral Sclerosis, Huntington's disease, Parkinson's disease, brain and myocardial infarctions, spinal cord damage, immune disorders, osteoarthritis and restoration of ovarian function. It has been also shown animal studies that MSCs increase sperm motility and the number of spermatogonia. In addition, they release a wide selection of cytokines, chemokines, and growth factors, with antiapoptotic, anti-inflammatory, proangiogenic, and immunomodulatory characteristics, making them highly attractive for a variety of medical applications [9, 10, 11, 12, 13, 14, 15].
Therefore, the objective of this study was to describe the case report of a patient who’s UVF was repaired with conservative treatment using ADMSCs IV injection, as an adjuvant.
Case presentation
A 36-year-old woman with a history of cesarean section in 2003 (38 weeks pregnant) due to entangled umbilical cord and cesarean section in 2017 (40 weeks pregnant) due to placental abruption. She was admitted with active labor in the Labor, Delivery and Recovery (LPR) guard of the Bité Médica Hospital at 40.2 weeks pregnant. Cervical dilation was confirmed to be 5 cm by her medical practitioner, Fetal Heart Rate was 140 bpm. Whilst spontaneous rupture of membranes during active uterine contractions presented, blood-stained amniotic fluid was seen and placental abruption was diagnosed. Fetal tachycardia was also observed. It was decided to perform an emergency cesarean section. Live and healthy newborn (3.975 grams weight, 53 cm length and APGAR score of 9/10).
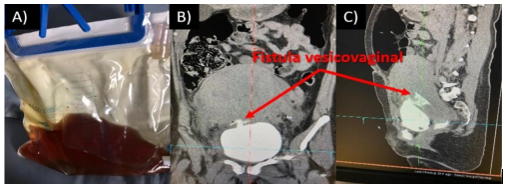
Three hours after cesarean delivery, macroscopic hematuria was observed. Permanent transurethral catheterization with a 18F Silastic Foley catheter was indicated (figure 1). Hematuric urine was still seen in spite of lessening stress on the bladder. Evaluation through Computarized Tomography Cystography (Cisto-CAT) was performed [Emotion16(2010) CT 78883, Somaris/5 syngo CT 2014A]. A defect was detected in the fundus of urine bladder, confirming abnormal communication between uterus and bladder, of approximateley 7.5 mm. (Figure 2). Conservative treatment was chosen.
A) Foley catheter in which hematuria could be observed, B and C) Cysto- CT showed the passage of contrast from the bladder to the uterus, through a 7.5 mm fistula.
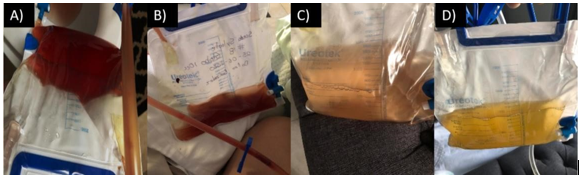
Three weeks after starting treatment, hematuria was still observed and no decrease in UVF was observed. Therefore, intravenous injection of Adipose Tissue Stem Cells (ADMSCs) was proposed to the patient and her partner. The positive results that we have obtained using ADMSCs as an adjuvant for the repair of placental hematomas was explained to them, and thus, the plausibility of this measure. After the patient had accepted the treatment, the application of 120 million ADMSCs (homologous) was injected as a intravenous infusion.
After the application of ADMSCs, outpatient daily follow up using photographs of urine drainage bag was carried out for three weeks. Progressive clearing of urine color was taken as evidence of UVF narrowing and complete repair of the fistula was confirmed with Cysto CT control image. (Figure 2 and 3).
Discussion
Conservative treatment of UVF has been followed up for years and various methods have been detailed that allow a fistula to be spontaneously repaired. Such is the case of continuous bladder drainage, catheterization with fulguration of the fistula tract, glue injection, platelet-rich plasma, and the administration of anticholinergics [16]. Most conservative methods have a reported success rate ranging from 3% to 100%. In addition, conservative methods should be used in carefully selected patients, since clinical scenarios vary. Therefore, the choice of a conservative method depends on the physician's experience, always bearing in mind that surgical intervention will be required if conservative treatment would fail [5]. Conservative treatment is even used as a strategy to give fistula closure an opportunity and as a measure to deflate the tissues prior to intervention, since in the immediate postsurgical or postpartum period, the structures are modified, frequently found friable and edematous. All of these implies the possibility of fistula recurrence if surgery is performed in this acute phase [17].
Regarding ADMSCs as an adjuvant treatment for UVF, there are studies in laboratory animals (such as the one carried out by Mardiyan E. et al., 2020), where they observed in NZW rabbits that the application of mesenchymal stem cells, obtained from amniotic membrane directly into the fistula, reduced TNFα concentrations and inflammatory cell infiltration, enhancing the reduction of UVF. Similarly, in this case report, the application of 120 million ADMSCs intravenously was able to help reduce and fully repair a 7.5 mm UVF over the course of 3 weeks. In the case of humans (Dietz A. et al., 2017), in a clinical trial that included 12 patients with Crohn's disease, they applied ADMSCs in a bioabsorbable matrix for perianal fistula repair, observing clinical repair in 83% of patient cases. In the investigation performed by Aho J. et al., 2016, a graft seeded with autologous ADMSCs was used to repair recurrent bronchopleural fistula (BPF) and showed that, follow-up at 3, 6 and 18 months after application of Ad-MSCs did not present recurrence of BPF. The review by Borycka K. et al., 2019, concluded that the application of directly injected ADMSCs could be a promising tool for the management of perianal fistulas resistant to treatment.
Currently, there are few clinical trials that evaluate the efficacy of ADMSCs as an adjuvant treatment for UVF; in addition, the studies that can be found have only been carried out in laboratory animals. In a systematic analysis in the Cochrane database, no related articles were found. ADMSCs may be an innovative, safer, therapeutic field of study for the treatment of fistulas, although it needs more clinical studies to fully understand the nature and therapeutic scope of ADMSCs.
Conclusions
The intravenous injection of ADMSCs as an adjuvant in conservative treatment of UVF helped to its completely closure and repair.
Due to the aforementioned, we propose to carry out prospective, multicenter and randomized studies, using conservative management with the intravenous application of autologous MSCs as the first therapeutic option and perform detailed follow up during the next 3 weeks in addition to lifestyle medicine measures to reduce inflammation and promote the repairing activity of mesenchymal stem cells.
References
- G. Shafqat, A. Khan, S. Azam and R. Murad, (2021) Multipara with utero-vesical fistula following repeat cesarean section: a rare iatrogenic complication, Radiology Case Reports, vol. 16, pp. 3940-3944.
View at Publisher | View at Google Scholar - M. Bettez, G. Breault, L. Carr and L. Mai, (2011) Early versus delayed repair of vesicouterine fistula, Canadian Urological Association, vol. 5, no. 4, pp. e52-e55.
View at Publisher | View at Google Scholar - A. Jilaveanu, B. Socea, R. Bohiltea, O. Stiru, A. Aloul, B. Ursut, C. Savu, A. Filipescu, I. Balescu, N, Bacalbasa, (2023) Uterovesical fistulas as obstetric complications: Diagnosis, management and prognosis (Review), Experimental and Therapeutic Medicine, vol.25, no.105, pp.1-4.
View at Publisher | View at Google Scholar - R. Machada, L. Machado and L. Lourenço, (2018) Vesicouterine fistula (youssef syndrome): Case report and literature review, Revista Brasileira de Ginecologia e Obstetrícia , vol. 40, no. 9, pp. 563-569.
View at Publisher | View at Google Scholar - E. Mardiyan and N. Anisah, (2021) The Role of Regenerative Medicine in Wound Healing in Cases of Vesicovaginal Fistulae, Journal of Drug Delivery and Therapeutics, vol. 114, no. 4-S, pp. 5-8.
View at Publisher | View at Google Scholar - E. Buscail, G. Le, F. Gross, M. Lebrin, L. Bugarel, C. Deraison, N. Vergnolle, B. Bournet, C. Gilletta and L. Buscail, (2021) Adipose-Derived Stem Cells in the Treatment of Perianal Fistulas in Crohn’s Disease: Rationale, Clinical Results and Perspectives, International Journal Molecular Sciences, vol. 22, no. 18, pp. 1-22.
View at Publisher | View at Google Scholar - L. Frese, P. Dijkman y S. Hoerstrup, (2016) Adipose Tissue-Derived Stem Cells in Regenerative Medicine, Transfus Med Hemother, vol. 43, nº 4, pp. 268-274.
View at Publisher | View at Google Scholar - W. Tsuji, J. Rubin y K. Marra, (2014) Adipose-derived stem cells: Implications in tissue regeneration, World J Stem Cells, vol. 6, nº 3, pp. 312-321.
View at Publisher | View at Google Scholar - M. Edessy, H. Hosni, Y. Shady y Y. Waf, (2016) Autologous Stem Cells Therapy, the First Baby of Idiophatic Premature Ovarian Failure, Acta Medica Internacional, vol. 3, pp. 19-23.
View at Publisher | View at Google Scholar - A. Elfayomy, S. Almasry, S. El-Tarhouny y M. Eldomiaty, (2016) Human Umbilical Cord Blood-Mesenchymal Stem Cells Transplantation Renovates the Ovarian Surface Epithelium in a Rat Model of Premature Ovarian Failure: Possible Direct and Indirect Effects, Tissue and Cell, vol. 48, pp. 1-13.
View at Publisher | View at Google Scholar - M. Ghadami, E. El-Demerdash, E. Zhang, S. Salama, A. Binhazim, A. Archibong, X. Chen, B. Ballard, M. Ram y A. Al-Hendy, (2012) Bone Marrow Transplantation Restore Follicular Maturation and Steroid Hormones Production in a Mouse Model for Primary Ovarian Failure, PLOS ONE, vol. 7, p. e32462.
View at Publisher | View at Google Scholar - R. Shammaa, A. El-Hakim, J. Abusarah y M. Rafei, (2020) Mesenchymal Stem Cells Beyond, Frontiers in Cell and Developmental Biology, vol. 8, nº 72, pp. 1-17.
View at Publisher | View at Google Scholar - A. Afflerbach, M. Kiri, T. Detinis y B. Maoz, (2020) Mesenchymal Stem Cells as a Promising Cell Source for Integration in Novel In Vitro Models, biomolecules, vol. 10, nº 1306, pp. 1-30.
View at Publisher | View at Google Scholar - H. Chi, A. Tung, C. Chih, C. Ming, L. Liang and J. Hui, (2019) Mesenchymal stem cells restore the sperm motility from testicular torsion-detorsion injury by regulation of glucose metabolism in sperm, Stem Cell Research & Therapy, vol. 10, no. 270, pp. 1-12.
View at Publisher | View at Google Scholar - M. Monsefi, B. Fereydouni, L. Rohani y T. Talaei, (2013) Mesenchymal stem cells repair germinal cells of seminiferous tubules of sterile rats, Iranian Journal of Reproductive Medicine. - NCBI, vol. 11, nº 7, pp. 537-544.
View at Publisher | View at Google Scholar - S. Rajaian, M. Pragatheeswarane and A. Panda, (2019) Vesicovaginal fistula: Review and recent trends, Indian Journal of Urology, vol. 35, no. 4, pp. 250-258.
View at Publisher | View at Google Scholar - E. Mardiyan, A. Nur, B. Santoso, H. Parathon, Widjiati, F. Rantam and T. Hastomo, (2020) Effect of amniotic membrane-derived mesenchymal stem cells on TNF-α expression and inflammatory cells infiltration during vesicovaginal fistule repair healing process, Department of Obstetrics and Gynecology Clinic, vol. 14, no. 2, pp. 1518-1522.
View at Publisher | View at Google Scholar - A. Dietz, E. Dozois, J. Fletcher, G. Butler, D. Radel, A. Lightner, M. Dave, J. Friton, A. Nair, E. Camilleri, A. Dudakovic, A. Van Wijnen and W. Faubion, (2017) Autologous Mesenchymal Stem Cells, Applied in a Bioabsorbable Matrix, for Treatment of Perianal Fistulas in Patients With Crohn's Disease, Gastroenterology, vol. 153, no. 1, pp. 59-62.e2.
View at Publisher | View at Google Scholar - J. Aho, A. Dietz, D. Radel, G. Butler, M. Thomas, T. Nelson, B. Carlsen, S. Cassivi, Z. Resch, W. Faubion and D. Wigle, (2016) Closure of a recurrent bronchopleural fistula using a matrix seeded with patient-derived mesenchymal stem cells, Stem Cells Translational Medicine, vol. 5, no. 10, pp. 1375-1379.
View at Publisher | View at Google Scholar - K. Borycka, A. Pietrzak, M. Kielar and W. Tarnowski, (2020) Mesenchymal stem cells for the treatment of complex perianal fistulas in patients with Crohn disease, Polski Przeglad Chirurgiczny, vol. 92, no. 1, pp. 34-47.
View at Publisher | View at Google Scholar