Current Issue : Article / Volume 3, Issue 1
- REVIEW ARTICLE | DOI:
- https://doi.org/10.58489/2836-497X/021
General complication of laparoscopic surgery, necesary review
1 First-degree specialist in general surgery and assistant professor.
2 First-degree specialist in general surgery and assistant professor.
3 Comprehensive general stomatology specialist.
4 First- and second-degree specialist in general surgery, assistant professor, assistant researcher and consulting professor.
Pedro Rolando López RodrÃguez *
Pedro Rolando López RodrÃguez, Anthony Alvarez Morales, Yosniel Lugo EchevarrÃa, Anaisa León MursulÃ, (2024). Areas and situations for the study of water sustainability. Archives of Gynaecology and Women Health. 3(1); DOI: 10.58489/2836-497X/021
© 2024 Pedro Rolando López RodrÃguez, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 28-04-2024
- Accepted Date: 01-05-2024
- Published Date: 09-05-2024
laparascopic surgery, complications, laparascopic techniques
Abstract
Introduction: âMinimal Access Surgeryâ began in animal laboratories and was later studied in selected academic centers where it was imported to community hospitals only when its benefits and safety were established. Objectives: To conduct a detailed review of Complications of laparoscopic surgery with emphasis on those related to entry into the abdominal cavity and bile duct surgery given their high frequency and lethality. Subject and methods: A detailed search of literature published in Spanish and English was carried out through PubMed/MEDLINE, Cochrane's registry of systematic reviews and randomized controlled studies, using key words such as âlaparoscopic entryâ, âtrocars injuryâ, âlaparoscopyâ. complicationsâ, âlaparoscopic injuryâ and âoptical trocarsâ. Meta-analyses, randomized clinical studies, clinical guidelines, review articles and case series were mainly selected.Conclusions: Laparoscopy is a relatively safe procedure, however, great care must be taken during access to the abdominal cavity because the majority of complications occur during entry.
Introduction
Minimal Access Surgery” began in animal laboratories and was later studied in selected academic centers where it was imported to community hospitals only when its benefits and safety were established. Low complication rates were reported by centers specialized in laparoscopic surgery, mostly academic centers. These centers were able to reduce complication rates to a minimum by developing the skills necessary for these surgeries. Unfortunately, many inexperienced surgeons developed these techniques without sufficient training and are responsible for the majority of complications obtained during laparoscopic surgery.1
The development of Laparoscopic Cholecystectomy (LC) was not designed to improve the safety of the procedure, but rather to reduce the discomfort associated with the surgical incision.
Doctors who have performed fewer than 100 such procedures have reported a complication rate of 14.7 per 1,000 patients. In contrast, expert surgeons reported having a complication rate of only 3.8 complications per 1000 procedures. The Southern Surgeons' Club reported that the survey or incidence of bile duct injuries was 2.2% when the surgeon had performed fewer than 13 procedures. As surgeons gained experience, the incidence of bile duct injuries eventually decreased to 0.1% (2,3).
Objectives
Carry out a detailed review of the Complications of laparoscopic surgery with emphasis on those related to entry into the abdominal cavity and bile duct surgery given their high frequency and lethality.
Methods
A detailed search of literature published in Spanish and English was carried out through PubMed/MEDLINE, Cochrane's registry of systematic reviews and randomized controlled studies, using key words such as “laparoscopic entry”, “trocars injury”, “laparoscopy complications”, “laparoscopic injury” and “optical trocars”. Meta-analyses, randomized clinical studies, clinical guidelines, review articles and case series were mainly selected.
Development
The use of laparoscopy to perform surgical procedures is increasing as it provides greater benefits, when compared to laparotomy, in terms of faster recovery, less postoperative pain, and shorter hospital stay. However, since it is an invasive procedure, there is a risk of complications. These are divided into Intraoperative and Postoperative, but we are going to refer to Intraoperative, which in turn can be divided into 2 large groups:4
A – General Complications of Laparoscopic Procedures:
1- Related to the Introduction of Needles, Trocars and Insufflation
2- Typical of Pneumoperitoneum
3- Related to the introduction of laparoscopic surgical materials and manipulation of instruments.
B – Specific complications of each technique: (Biliary Surgery)
General Complications of Laparoscopic Procedures:
1 - Related to the Introduction of Needles, Trocars and Insufflation
It is with the introduction of the Veress needle to create the pneumoperitoneum that any laparoscopic procedure begins. The impossibility of creating this adequately makes it impossible to place trocars correctly and will cause the surgery to fail.
Veress Needle and Trocars
Despite the advantages offered by the protection system of this needle during its introduction, different injuries can occur, such as:
- Injury to the Abdominal Wall Vessels:
This complication is relatively frequent, it occurs mainly with the introduction of trocars and especially with those that have sharp edges (they have the advantage of requiring less pressure for their introduction into the abdominal cavity) than with those with a conical tip, less causing this complication. The solution to this is usually the compression of the wall, either directly with the sheath, or with the introduction of the sheath fixing sleeve that has a larger diameter and if it is not controlled, small enlargements of the wound corresponding to the point of bleeding until they are located and hemostasis is achieved.
To avoid this, it is advisable to transilluminate the wall to visualize the larger caliber vessels in order to avoid injury.
- Large Vessel Injury:
This is usually due to injuries to the abdominal aortic bifurcation or the inferior vena cava, producing a large retroperitoneal hematoma that requires urgent laparotomy. The incidence of this complication is fortunately low, amounting to 0.05percentage in large multicenter series, but frequently fatal, which is why the introduction of the needle and the first trocar must be done with great care and with gentle maneuvers. If an injury occurred, depending on its magnitude, a laparotomy must be performed, checking for the existence of a vascular wound on the posterior face of the vessel at the level of the previous wound, and suturing it if necessary (5,6).
- Hollow Viscera Injury:
This can be in: Stomach, Small Intestine or Colon. It can occur more frequently when there is a previous abdominal surgery, which implies the possible existence of adhesions of the digestive tract to the anterior wall, which recommends puncture with the Veress needle away from the laparotomy scar, in an upper quadrant, normally the left another method of avoiding this is by placing a Hasson trocar under direct vision (open Pneumoperitoneum). This injury can go unnoticed, which increases its severity as it is diagnosed late.
- Solid Viscera Injury:
It is infrequent, it is discovered once the optic is inserted and it is not usually serious; it is usually superficial punctures of the liver, which spontaneously stop bleeding.
- Hernias in the trocar orifices:
Infrequent complication in holes of 5 and 10 mm in a lateral situation, but very common in holes greater than 10 mm, especially in the midline and in the region of the lower abdomen, although it can appear in the upper abdomen if the incision for extraction is extended. of the surgical specimen, so suturing the aponeurosis of the midline trocars is always recommended. It is also important to take into account when removing the 10 mm trocar, especially the one in the umbilical region, since it cannot be removed suddenly because the CO2 must first be emptied from the cavity otherwise evisceration occurs due to the pressure. positive intra-abdominal that forces the greater omentum, small intestine, out of the abdominal cavity and may go unnoticed at the end of the surgery (7,8,9).
An example of all of the above is that, in 2001, Bhoyrul and collaborators analyzed 629 injuries caused by trocars, reported to the Food and Drug Administration (FDA) between 1993 and 1996. 32 deaths were reported, of which 26 resulted from injury. vascular and 6 intestinal injuries, disposable trocars were used in 28 deaths, 3 by optical vision and 1 by reusable trocars, 408 injuries were vascular injuries and 182 were visceral injuries, 30 wall hematomas occurred and the other patients were not analyzed. These authors conclude that disposable trocars and direct entry do not reduce visceral complications, and an unrecognized intestinal injury can be fatal (10,11,12).
Insufflation
- Gas insufflation into the abdominal wall, mesentery, omentum or retroperitoneum:
Insufflation of CO2 into the omentum, mesentery or retroperitoneum produces emphysema that does not have great repercussions and disappears quickly, but the possibility of a vascular or visceral injury below this must be ruled out. These emphysemas often make the operating field difficult since they reduce the visual field and modify anatomical structures. (13)
If this insufflation occurs in the abdominal wall, it causes subcutaneous emphysema, which, although it has no clinical significance, can make it difficult to achieve pneumoperitoneum. It is evidenced by an asymmetrical abdominal distention of the abdominal wall, the presence of subcutaneous emphysema due to crepitus in the abdomen and high pressures marked by the insufflator and which warn us of incorrect placement of the needle.(14,15) In obese patients Gas insufflation may occur in the preperitoneal space that simulates a pneumoperitoneum since it can hold 3 to 4 liters in the preperitoneal space that occurs even with symmetrical abdominal distention, but it is quickly recognized by high pressures maintained in the laparoinsufflator, as well as the absence of negative pressure. Therefore, it is important to always perform negative pressure tests of the abdominal cavity, injection of air or liquid into the abdominal cavity with subsequent aspiration, and laparoinsufflator values below 8 mmHg. This is often detected when introducing the optic and observing that it is not in the abdominal cavity, making it necessary to communicate this space with the intra-abdominal space. (16,17,18)
2 - Typical of Pneumoperitoneum:
- Gas Embolism:
Produced by the sustained insufflation of CO2 pressures directly into a large-caliber venous vessel, it is a serious complication that requires rapid decompression of the abdominal cavity followed by cardiorespiratory recovery maneuvers, which is why it is recommended not to use flows at the establishment of pneumoperitoneum greater than 1 or 1.5 liters per minute. (19,20)
It is recognized by the appearance of profuse sweating, sustained arterial hypotension, jugular engorgement, tachycardia, cardiac arrhythmias and distal cyanosis, as well as the recording of arterial O2 desaturation and hypercapnia raise the suspicion of this complication.
- Pain in the shoulders:
It seems to be related to the irritation of the diaphragms by CO2 and the rupture of its myofibrils. So, an inflation pressure of 1 – 1.5 liters/min. prevents sudden distension of the diaphragm. This pain is easily combatable with analgesics and disappears in the first 48 hours after surgery.
- Iatrogenic Pneumothorax:
Its mechanism of appearance is not clear but barotrauma is invoked due to the sudden insufflation of the pneumoperitoneum, as well as possible congenital diaphragmatic defects that establish a pleuropulmonary communication that makes its establishment possible by increasing intra-abdominal gas pressures. Generally this is resolved in the same surgical procedure, being very complicated if a hypertensive pneumothorax occurs where there is an increase in intrapulmonary pressures and O2 desaturation that is resolved with a Pleurostomy.
- Pneumomediastinum:
This generally occurs in esophageal hiatus surgeries when the abdominal cavity comes into contact with the lower mediastinum, so it is recommended to work with pressures less than 12 mmHg to avoid cardiac arrhythmias and cardiac tamponade that sometimes accompany this complication.
- Respiratory problems:
The hypercapnia that occurs during laparoscopic surgery is due to the sum of two factors: the increase in dead space (well-ventilated but poorly perfused alveoli) and the absorption of CO2 by pneumoperitoneum. The measurement of expired CO2 (ETCO2) will be a good non-invasive control method; on the other hand, O2 saturation does not seem to be altered by pneumoperitoneum, but peak pressure (maximum pressure produced in the airway at each time) is elevated. ventilatory cycle, also producing a discrete metabolic acidosis, which becomes more evident the greater the hemodynamic impact. (21,22,23)
- Hemodynamic Repercussions:
At the beginning of insufflation, there is an increase in Central Venous Pressure (CVP), mean arterial pressure and cardiac output, but once the mean working pressure (12-14 mmHg) is established, it is higher than that of the vena cava, which decreases CVP as well as cardiac output. Hypoxia, hypercapnia and decreased cardiac output may be the most important factors in the development of cardiac rhythm disorders.
3- Related to the introduction of laparoscopic surgical materials and manipulation of instruments:
The use of instruments inside the abdominal cavity must always be carried out under optical vision, to avoid injuries to the different abdominal organs, so we will follow their entire journey from their entry into the cavity. The design of this type of instruments such as scissors, aspiration cannulas and forceps are long, so perforation can occur at any level if these instruments are not entered under endoscopic vision. Injuries caused by incorrect use or uncontrolled mobilization of surgical instruments can go unnoticed, increasing their severity. (24,25,26)
Electrocoagulation deserves a separate comment, which is used with the dissector, scissors or hemostasis forceps. Its improper use can cause thermal injuries in unwanted places (diaphragm, digestive tract, bile duct, etc.). (26)
The high intensity of the light produced by the xenon source is capable of providing burns if the contact between the tip of the endoscope and the tissue or organ is prolonged. Inadvertent burns at the gastrointestinal level can cause perforation peritonitis, which generally appears on the 4th day. postoperative period, which is why the laparoscope must always be removed inside the trocar in the event of loss of pneumoperitoneum. (27)
Specific complications of each technique: (Biliary Surgery)
The risk of bile duct injury during laparoscopic cholecystectomy has increased due to the position and exposure of the anatomical structures of the extrahepatic bile ducts.
"Post-surgical or Iatrogenic Bile Duct Injury" is defined as any change secondary to surgery that causes bile leak from the biliary tree before the duodenal papilla, difficulty or impossibility of the passage of bile to the duodenum, or combinations of these. Vascular lesions of the biliary tree are also included, and can be of the hepatic, common, right or left arteries, as well as the portal vein. (28)
The annual incidence of bile duct injuries increased from about 0.2percentage in the open cholecystectomy era to approximately 0.5 after laparoscopic cholecystectomy became widely available. (29)
Imaging is vital for initial diagnosis, evaluation of the extent of the injury, and planning prior to the surgical procedure. The use of percutaneous cholangiography, endoscopic retrograde cholangiopancreatography and magnetic resonance cholangioresonance allows establishing the site of the lesion. For the diagnosis of bile leaks and post-surgical biliary strictures, percutaneous cholangiography is considered the reference technique.
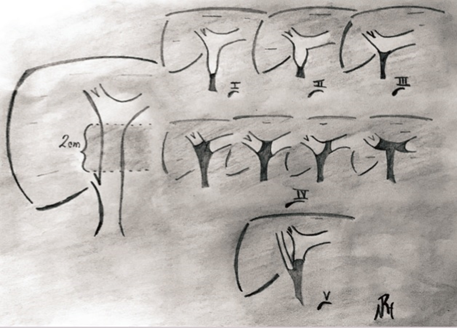
Bismuth Classification:
In 1982, Bismuth proposed a classification for Benign Primary Bile Duct Stenosis that is based on the anatomical pattern of the lesion. They are classified into five grades according to the relationship they acquire with the confluence of the right and left hepatic ducts, not only defining postoperative strictures specifically, but also allowing comparisons of different therapeutic modalities with respect to the extent of the affected bile duct.
In turn, benign biliary strictures are subdivided according to the degree of suprastenotic dilation.
Type I: Lesion greater than 2 cm from the confluences of the hepatic ducts (18 – 36percentage)
Type II: Lesion less than 2 cm from the confluences of the hepatic ducts (27 – 38percentage)
Type III: Lesion that coincides with the confluence of the hepatic ducts (20 – 33percentage)
Type IV: Destruction of the confluence, separated right and left hepatic duct (14-16percentage)
Type V: Involvement only of the right sectoral branch or in the common bile duct (0-7percentage)
Strasberg classification
This in turn defines Laparoscopic Injuries of the portal bile duct, which can be applied in the management of said injuries:
A - Leakage from the stump of the cystic duct or leakage from a canaliculus in the liver bed.
B - Occlusion of a part of the biliary tree, almost invariably an aberrant right hepatic duct.
C - Transection without ligation of the aberrant right hepatic duct.
D - Lateral damage to a major hepatic duct.
E - Subdivided by Bismuth classification into E1-E5.

Complications of cholecystectomy:
The female sex is the one that has presented the most iatrogenic lesions of BPV since it is the one that undergoes the most surgery for benign diseases of the Gallbladder, this corresponds to what is reported by the world literature which indicates that the female sex is the most affected by gallbladder lithiasis as well as secondary stones in the common bile duct, which is why they are at greater risk of suffering from acute biliopancreatic conditions and, therefore, having this procedure performed(30).
- Injury to the main bile duct.
Injuries to the main bile duct have been the greatest concern since the emergence of the laparoscopic era. It is undoubtedly the most serious complication that can occur when performing a cholecystectomy and the mechanism by which it occurs can be diverse:
1. Clipping and total or partial section of the common bile duct: This complication occurs by excessively pulling on the cystic duct, angulating the common bile duct and placing the clip so that the main bile duct is cut instead of the cystic duct. Sometimes the clip affects the cysticocholedochal junction, partially occluding the common bile duct lumen. Other times, the cystic duct is confused with the distal common bile duct in the dissection, clipping and sectioning it in its entirety.
2. Hemorrhage in Calot's triangle. An uncontrolled attempt at hemostasis, without good visualization of the bleeding vessel and with the placement of countless clips, can result in total or partial occlusion of the bile duct.
3. Injury with electrocautery. Areas of necrosis or retractions may occur that subsequently lead to a stenosis of the bile duct.
- Hemorrhage:
The two most frequent causes of hemorrhage during laparoscopic cholecystectomy are: injury to the cystic artery and bleeding from the gallbladder bed. These are usually overcome when the surgeon has experience.
Hemorrhage from the gallbladder bed can be very annoying, with the risk and difficulty of hemostasis being greater in cirrhotic patients, so we recommend sticking as much as possible to the wall of the gallbladder even at the cost of producing small gallbladder perforations that have no greater importance, and that only require a correct washing of the subhepatic and subphrenic spaces.
In case of Cystic Artery Injury, hemostasis must be performed with a clamp temporarily, so that it allows us to aspirate the blood and perfect visualization of the vessel that we are going to clip.
When hemorrhage occurs in the immediate postoperative period, the indication for surgical revision is imposed, starting with the laparoscopic route that allows us to wash-aspirate clots and blood from the abdominal cavity. Once it is confirmed that there is no active bleeding, a penrouse drainage tube is placed in the Winslow Hiatus.
- Forgotten Calculations:
Relatively frequently, stones fall into the peritoneal cavity, this can be complicated if the stones are not easily visualized. For this reason, on some occasion’s stones remain in the abdominal cavity that only exceptionally cause problems in the form of an abscess, which is why these must be removed either with the aspirator if they are small in size or with tweezers through the 10 mm pods.
Coleperitoneum:
The treatment is laparoscopic reintervention, with cavity washing, new transcystic cholangiograms and after verifying the existence of a leak, the subhepatic space is drained with a silicone tube, leaving the probe used for the cholangiographies and extracting it through another contracture for the subsequent checking the bile duct.
Complications in choledocholithiasis surgery:
Laparoscopic management of choledocholithiasis, as in laparotomic surgery, involves correct exposure of the main bile duct and this is where the most frequent intraoperative problems can occur.
- Hemorrhage:
It occurs as a consequence of injury to the pericholedochal vessels, and although it is not usually important, it does hinder correct visualization of the common bile duct, which requires its hemostasis with a suture, or very carefully with the use of electrocautery. so as not to produce thermal injuries that cause subsequent stenosis.
Bilirhagia:
Bile loss through subhepatic drainage does not usually cause problems. It is common for patients undergoing primary choledochorrhaphy to have a flow of 300-400 ml of bile through the subhepatic drainage during the first 24-48 hours, reducing drastically in the following hours.
- Residual Lithiasis:
This is undoubtedly the complication that most affects the patient, since it will give rise to a new procedure that will have to be undergone, whether surgical, endoscopic or radiological depending on the time of diagnosis and whether or not the patient is a carrier of the disease. a Kehr T-tube.
The complications associated with ERCP and EE are hemorrhage, pancreatitis, perforation and infection. ERCP, more than any other endoscopic procedure, has risk factors for complications depending on the patient, the procedure and the endoscopist (6).
Preventive Measures to avoid Iatrogenic Bile Duct Injury: (LIVB)
There are multiple techniques for the prevention of LIVB: use of a 30-degree chamber, avoidance of the use of thermocoagulation near the main VB, meticulous dissection, and conversion to open surgery when the anatomy is uncertain. In the CL, the reference point is the Rouviere Groove. Since the main cause of LIVB is misidentification of the main VB or an aberrant duct as CC, the surgeon must use an artery and CC identification method. Among the methods used we highlight:
1. Tristructure Method: We must identify during LC: CC, common hepatic duct and common bile duct.
2. Fischer method: It consists of separating the gallbladder completely from the gallbladder bed from the bottom towards the infundibulum as in open surgery, until it hangs from the artery and the CC. This is especially difficult in the case of intrahepatic or highly inflamed vesicles.
3. Infundibular Technique: It consists of identifying the CC when it joins the gallbladder infundibulum. It is the technique most currently used in most centers. It has the disadvantage of not preventing LIVB in patients with occult cystic duct syndrome. For this reason, different groups systematically recommend the use of intraoperative cholangiography (IOC) with this type of technique.
4. Strasberg's Critical View Technique: It is the preferred method by most surgeons, it consists of dissecting and releasing the Calot triangle until exposing the artery, the cystic duct (CC) and exposing the base of the gallbladder. observing the liver without any structure that interferes with the visualization of this organ. Once this view is achieved, these structures can only correspond to the duct and the cystic artery. (31)
VCS is a method described in 1992 and published by Dr. Steven M. Strasberg. Later in 2013, Stanford and Strasberg proposed photographic documentation of VCS with the aim of increasing safety in laparoscopic cholecystectomies. This photodocumentation consists of qualifying the anterior and posterior vision of the SVC using an established score, using the term double view, constituting an excellent method for preventing bile duct injury and perhaps the next step. With greater importance in the lists presented by the 2018 Tokyo Guidelines for the surgical management of Acute Cholecystitis, the partial diffusion that SVC has had in surgical practice may be one of the main limitations in the development of the so-called culture of safe cholecystectomy. In 2017, Dr. Strasberg noted that he had detected that after 20 years many surgeons have little understanding of the criteria required to achieve SVC, especially those who did not have training in implementing SVC in laparoscopic cholecystectomies during their residency, so who opt for simpler methods such as the Infundibular technique, which represent a greater risk of injury to the Biliary Tract. Other obstacles mentioned are that when SVC is carried out, photographic documentation is generally not carried out with the qualification of the “pair vision.” Cholangiography: Since the Argentine Pablo Mirizzi introduced the first intraoperative cholangiography in 1932 until today, its benefit in preventing LIVB is debated since IOC can help avoid LIVB for at least 3 reasons:
. Shows the diversity of the biliary tree and its abnormalities.
. Helps the surgeon identify patients at risk for LIVB due to abnormal anatomies.
. If LIVB has occurred, it allows for its identification and repair.
6. Intraoperative laparoscopic ultrasound: In a recent multicenter study, its advantages for the prevention of LIVB are highlighted, although it is a very expensive method and sometimes not available in all hospitals, which does not completely replace IOC but which opens a hopeful future. (32)
Conclusions
Laparoscopy is a relatively safe procedure, however, great care must be taken during access to the abdominal cavity because most complications occur during entry.
Cholangiography continues to be, above cholangioresonance, the ideal imaging method to visualize and stage bile duct lesions since it allows percutaneous derivation to control, leak or obstruction of the biliary tree (5).
Biliary Tract Injuries have increased considerably in the last two decades, due to the predominance of laparoscopic cholecystectomy over open surgery, which has been correlated with an increase in the incidence of bile duct injuries. Overall, the frequency of bile duct injuries ranges from 0.1 to 0.6%. These injuries are three to four times more frequent during laparoscopic cholecystectomy (0.3-0.6%) than open cholecystectomy (0.1-0.3%). Strasberg's review is very significant, since in 124,433 patients studied in 22 case series, a percentage of 0.52 is reported with a range of 0 - 2.35%(7).
Bile duct injuries produced during cholecystectomy can be avoided, almost without exception, if several aspects are taken into account, although it seems that the surgeon's good judgment, experience and expertise usually have the greatest weight.
The main Iatrogenic Biliary Tract Injury (LIVB) is undoubtedly the most disastrous accident that a patient could suffer during a laparoscopic cholecystectomy. This is an operation from which “everyone comes out well” and yet Suddenly the panorama has changed radically, the “easy” surgery has become a nightmare. By injuring a patient's bile duct we will have completely changed his life and his future, since the serious consequences of this fact can range from prolonged open surgery with the permanent possibility of repeated cholangitis, restenosis and therefore reoperations to cirrhosis. gallbladder and death.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Contribución de los autores
Anthony Alvarez Morales: conducted the surveys and searched the bibliography. He chose the sampling method by selecting the study population and analyzed and discussed the content of the tables.
Yosniel Lugo Echevarría: he posed the objectives of the study, selected and triangulated the variables and carried out the translation into English and the final revision of the manuscript.
Anaisa León Mursuli: she helped fill out surveys and search for bibliography, performed statistical processing, calculated the arithmetic mean and standard deviation of the quantitative variables. She applied the Family Functioning Perception Test or FF-Sil Test.
Pedro Rolando López Rodríguez: Performed the statistical processing, calculated and interpreted the chi-square and associated variables according to Duncan's twelfth. He wrote the document.
References
- libro_de_cirugia_laparoscopica_practica_2ed_[Librosmedicospdf.net].pdf> [cited 2021 Dec 30].
- Gomis, F. D., Masson, F. B., Abril, S. G., Aznar, J. R., & Juan, R. T. (2001). Complicaciones de la cirugía laparoscópica. Cirugía española, 69(3), 330-336.
- Avci, C., & Schiappa, J. M. (Eds.). (2015). Complications in Laparoscopic Surgery: A Guide to Prevention and Management. Springer.
- Sepúlveda-Agudelo, J. (2011). Complicaciones laparoscópicas asociadas a la técnica de entrada. Revista colombiana de Obstetricia y Ginecología, 62(1), 88-93.
- Ríos-Hernández, N., & Guadalupe, M. G. A. (2018, June). Lesiones de la vía biliar más frecuentes caracterizadas por colangiografía percutánea. Experiencia en un año en el servicio de radiología intervencionista. In Anales de Radiología, México (Vol. 17, No. 1, pp. 46-52).
- Olazábal García, E. A., Brizuela Quintanilla, R. A., Roque González, R., Barrios Osuna, I., Quintana Pajón, I., & Sánchez Hernández, E. C. (2011). Complicaciones de la colangiopancreatografía retrógrada endoscópica en las urgencias digestivas. Revista Habanera de Ciencias Médicas, 10(4), 465-475.
- lesiones_iatrogenicas_de_la_via_biliar.pdf>[cited 2022 Jan 4].
- Pacheco, S., Tejos, R., Rodríguez, J., Briceño, E., Guerra, J. F., Martínez, J., & Jarufe, N. (2017). Tratamiento quirúrgico de las lesiones iatrogénicas de la vía biliar poscolecistectomía. Revista chilena de cirugía, 69(3), 202-206.
- Barrera González, J. E., Ruiz Torres, J., Torres Peña, R., Martínez Alfonso, M. Á., Martínez López, R., Brizuela Quintanilla, R., ... & Olivé González, J. B. (2012). Tratamiento laparoscópico y endoscópico de la coledocolitiasis. Nuestra experiencia. Revista Habanera de Ciencias Médicas, 11(1), 104-111.
- Barreras González, J. E., Ruiz Torres, J., Torres Peña, R., Martínez Alfonso, M. A., Faife Faife, B. C., Hernández Gutiérrez, J. M., & Brizuela Quintanilla, R. (2010). Coledocolitiasis: Opciones actuales de tratamiento laparoscópico y endoscópico. Revista Habanera de Ciencias Médicas, 9(3), 374-384.
- Pardo Gómez G. Litiasis Biliar. En: García Gutiérrez A, Pardo Gómez G, (2007)editores. Cirugía. La Habana: Editorial Ciencias Médicas;. pp. 1193-1216..
- Bland, K. I., Sarr, M. G., Büchler, M. W., Csendes, A., Garden, O. J., & Wong, J. (Eds.). (2008). General surgery: principles and international practice. Springer Science & Business Media.
- Di Carlo, A., & McFadden, D. W. (2012). Choledocholithiasis and cholangitis. Zinner MJ, Ashley SW. Maingot's Abdominal Operations. Twelfth Edition. United States of America: The McGraw-Hill Companies, Inc.
- Doherty, G. M., & Way, L. W. (Eds.). (2010). Current diagnosis & treatment: surgery (Vol. 493, p. 498). New York, NY, USA:: Lange Medical Books/McGraw-Hill.
- González, J. E. B., & Peña, R. T. (2012). La colangiopancreatografía retrógrada con esfinterotomía endoscópica intraoperatoria como modalidad de tratamiento para la colédocolitiasis. Editorial Universitaria.
- Noble, H., Tranter, S., Chesworth, T., Norton, S., & Thompson, M. (2009). A randomized, clinical trial to compare endoscopic sphincterotomy and subsequent laparoscopic cholecystectomy with primary laparoscopic bile duct exploration during cholecystectomy in higher risk patients with choledocholithiasis. Journal of Laparoendoscopic & Advanced Surgical Techniques, 19(6), 713-720.
- De Silva, S. L., Pathirana, A. A., Wijerathne, T. K., Gamage, B. D., Dassanayake, B. K., & De Silva, M. M. (2019). Transabdominal Ultrasonography in Symptomatic Choledocholithiasis–Usefulness in Settings with Limited Resources. Journal of Clinical Imaging Science, 9.
- Fadahunsi, O. O., Ibitoye, B. O., Adisa, A. O., Alatise, O. I., Adetiloye, V. A., & Idowu, B. M. (2020). Diagnostic accuracy of ultrasonography in adults with obstructive jaundice. Journal of Ultrasonography, 20(81), 100-105.
- Chapron, C., Fauconnier, A., Goffinet, F., Breart, G., & Dubuisson, J. B. (2002). Laparoscopic surgery is not inherently dangerous for patients presenting with benign gynaecologic pathology. Results of a meta-analysis. Human Reproduction, 17(5), 1334-1342.
- Ahmad, G., Duffy, J. M. N., & Watson, A. J. S. (2007). Laparoscopic entry techniques and complications. International Journal of Gynecology & Obstetrics, 99(1), 52-55.
- Molloy, D., Kaloo, P. D., Cooper, M., & Nguyen, T. V. (2002). Laparoscopic entry: a literature review and analysis of techniques and complications of primary port entry. Australian and New Zealand journal of obstetrics and gynaecology, 42(3), 246-254.
- Parrilla Paricio P, Luján Monpean JA, Robles Campos R. Complicaciones en la cirugía laparoscópica. En: (1993) Laporte Roselló, E, editor. Cirugía laparoscópica. Barcelona: Pulso,.
- Lasnier, C., & Paineau, J. (2005, January). Bile duct injuries at laparoscopic cholecystectomy: early repair results. In Annales de chirurgie (Vol. 130, No. 4, pp. 218-223).
- Lasnier, C., & Paineau, J. (2005, January). Bile duct injuries at laparoscopic cholecystectomy: early repair results. In Annales de chirurgie (Vol. 130, No. 4, pp. 218-223).
- Barrat, C., Champault, A., Matthyssens, L., & Champault, G. (2004, February). Iatrogenic perforation of the gallbladder during laparoscopic cholecystectomy does not influence the prognosis. Prospective study. In Annales de chirurgie (Vol. 129, No. 1, pp. 25-29).
- Seeliger, H., Fürst, A., Zülke, C., & Jauch, K. W. (2002). Surgical management of bile duct injuries following laparoscopic cholecystectomy: analysis and follow-up of 28 cases. Langenbeck's Archives of Surgery, 387, 286-293.
- Stewart, L., Robinson, T. N., Lee, C. M., Liu, K., Whang, K., & Way, L. W. (2004). Right hepatic artery injury associated with laparoscopic bile duct injury: incidence, mechanism, and consequences. Journal of Gastrointestinal Surgery, 8, 523-531.
- Nuzzo, G., Giuliante, F., Giovannini, I., Murazio, M., D'Acapito, F., Ardito, F., ... & Di Stasi, C. (2008). Advantages of multidisciplinary management of bile duct injuries occurring during cholecystectomy. The American journal of surgery, 195(6), 763-769.
- Bektas, H., Schrem, H., Winny, M., & Klempnauer, J. (2007). Surgical treatment and outcome of iatrogenic bile duct lesions after cholecystectomy and the impact of different clinical classification systems. Journal of British Surgery, 94(9), 1119-1127.
- Csendes, A., Navarrete, C., Burdiles, P., & Yarmuch, J. (2001). Treatment of common bile duct injuries during laparoscopic cholecystectomy: endoscopic and surgical management. World journal of surgery, 25, 1346-1351.
- Fields, R. C., Heiken, J. P., & Strasberg, S. M. (2008). Biliary injury after laparoscopic cholecystectomy in a patient with right liver agenesis: case report and review of the literature. Journal of Gastrointestinal Surgery, 12(9), 1577-1581.
- De Reuver, P. R., Grossmann, I., Busch, O. R., Obertop, H., Van Gulik, T. M., & Gouma, D. J. (2007). Referral pattern and timing of repair are risk factors for complications after reconstructive surgery for bile duct injury. Annals of surgery, 245(5), 763-770.


