Archive : Article / Volume 1, Issue 1
Case Report | DOI: https://doi.org/10.58489/2833-0951/004
Gall bladder polyp in a bodybuilder with symptomatic uremia: An educational ultrasound image
Advisor doctor, Baghdad Medical City and the National Training and Development Center.
Correspondng Author: Aamir Jalal Al-Mosawi
Citation: Aamir Jalal Al-Mosawi (2022). Gall bladder polyp in a bodybuilder with symptomatic uremia: An educational ultrasound image. Biomedical and Biotechnological Sciences. 1(1). DOI: 10.58489/2833-0951/004
Copyright: © 2022 Aamir Jalal Al-Mosawi, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2022-07-14, Received Date: 2022-07-14, Published Date: 2022-08-04
Abstract Keywords: Symptomatic uremia, gall balder poly, an educational ultrasound image.
Abstract
Background: Gallbladder polyps are generally small benign lesions that do not enlarge for years. However, follow-up with ultrasound examination is initially recommended to detect unexpected malignancy. The diagnosis of a gallbladder polyp is generally made with ultrasound examination, and in many instances the polyp is detected while performing the ultrasound examination in the diagnostic work-up of a condition not related to the gallbladder.
Introduction
Gallbladder polyps are generally small benign lesions that do not enlarge for years. However, follow-up with ultrasound examination is initially recommended to detect unexpected malignancy. The diagnosis of a gallbladder polyp is generally made with ultrasound examination, and in many instances the polyp is detected while performing the ultrasound examination in the diagnostic work-up of a condition not related to the gallbladder [1-7].
Patients and methods
The occurrence of a gallbladder polyp in a bodybuilder with symptomatic uremia is described, and an educational ultrasound image is provided.
Results
At about the age of 50 years (March, 2022), a professional bodybuilder presented with progressive symptomatic uremia associated with nausea, vomiting, pruritus, and mild anemia. He was not havening reduction in urine output, edema or hypertension. His weight was about 100 Kg, and before his current illness he reported that his bench press single maximum repetition was 140Kg. On the 19th of March, blood urea level was 162 mg /dL and serum creatinine was 6.2 mg /dL.
Urinalysis showed 2 plus albuminuria and one plus amorphous urate. Blood calcium and serum electrolytes were within normal ranges, but he had mild hyperphosphatemia with serum phosphorus of 4.9 mg/dL (Normal range 2.4-4.4mg/dL). Hemoglobin was 10.7 mg/dL (Normal ranges: 11.5-16.5 g/dL).
Liver function tests were normal (Total serum bilirubin 0.8 mg/dL, Aspartate aminotransferase (SGOT) 25 iu/L, alanine aminotransferase (SPOT) 21 iu/L, alkaline phosphatase 284 iu/L).
He reported history of episodes of hyperglycemia that in the case of bodybuilders is generally attributed to growth hormone administration in excessive doses. However, the patient was reluctant to provide details about the performance enhancing medications such as anabolic steroids and growth hormone, and he was not confirming or denying the use of such agent. He was simply saying that he was taking protein supplements.
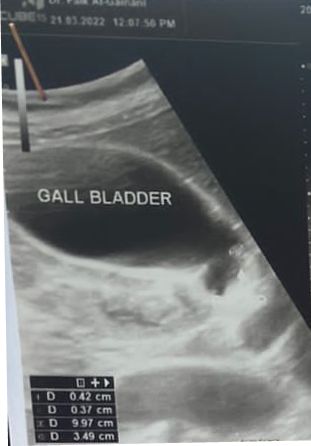
Renal ultrasound (Figure-1) confirmed the chronicity of renal failure and showed small kidneys (RK: 8 x 4, cortex 6 mm, LK: 8.2 x 4, cortex 6 mm). The kidneys had hyper-echoic texture with reduced cortical thickness and loss of the cortico-medullary differentiation. There were small cysts on both kidneys, not more than 1, 5 cm in diameter. Abdominal ultrasound also showed small polyp in the gall bladder (Figure-2) and mild enlargement of the prostate with a volume of 27 cm3 (Normally up to 25).

The patient initially required oral prochorperazine 5 mg for two days control the nausea and vomiting, and oral antihistamine plus topical crotamiton 10% to control pruritus. The conservative dietary (Acacia gum supplementation plus very low protein diet) and pharmacological managements were prescribed according to the latest published intestinal dialysis guidelines and included oral iron and folic acid capsule, and calcium carbonate [8-22].
He also received oral finasteride 5 mg daily for the prostatic enlargement.
After two weeks, the patient was asymptomatic and blood urea was lowered to 126.4 mg/dL, and the hemoglobin was increased to 11g/d. Ultrasound showed normal prostate size of 20 cm3.
Literature review suggested that the addition of essential amino acids and ketoanalogues in the management of chronic renal failure with intestinal dialysis can contribute to its enhancement [24, 25, 26, 27]. Therefore, Ketosteril (Fresenius), was prescribed in a low initial dose of three tablets, and was ordered to be brought to the patient from Turkey.
Discussion
Gallbladder polyp has been recognized as a medical condition as early as the 1911. Sand and Mayer reported eight patients with gallbladder polyps who had histopathological diagnosis of papilloma, and seven of them had gallstones [1].
In 1923, Abell reviewed 283 cholecystectomies, and found 8 cases of gallbladder polyps with histopathological diagnosis of adenoma [2].
In 1933, Kirklin reported the initial cholecystographic diagnosis of gallbladder polyps which had histopathological diagnosis of papilloma [3].
In 1934, Wellbrock, reviewed 9550 cholecystectomies, and found 69 cases of gallbladder polyps with histopathological diagnosis of adenoma [4].
However, in 1940, Walters and Snell reported finding gallbladder polyps with histopathological diagnosis of papilloma associated with eholesterolosis in about 8% of cholecystectomies [5].
In 1957, Kozoll and Meyer suggested that gallbladder polyps appear initially an inflammatory reaction to irritating cholesterol and infection. Thereafter, a superficial epithelialadenomatoid hyperplasia ensues within a cholesterol and macrophages-filled stroma with (Cholesterotoma). The occurrence of a significant glandular hyperplasia leads to the formation of a papilloma [6].
Until now, there is no evidence to support that high protein diet per se can cause chronic renal failure. However, nephrocalcinosis caused exogenous vitamin D intoxication was reported to cause renal failure in a bodybuilder athlete [23]. Therefore, an accurate causation of the chronic renal failure can not be determined.
Carrero et al (2020) emphasized the importance and benefits of fruits and vegetables in patients with chronic renal failure. The intake of fruits and vegetables is associated with a higher fiber intake which can cause a shift in the gut microbiota towards reduced production of uremic toxins. The intake of fruits and vegetables is also associated with lower intake phosphorus, and thus help in controlling hyperphosphataemia [28]. However, the latest published intestinal dialysis guidelines have already suggested intake of fruits and vegetables [22].
The use of Keto-analogues of essential amino acids in the management of chronic renal failure has been reported as early as the 1970s (Walser, 1978; Bauerdick and colleagues, 1978, Giovannetti et al, 1980) [24, 25, 26].
In 1981, Barsotti et al emphasized that treatment of chronic renal failure a very low protein diet plus essential amino acids and ketoanalogues is not associated with reduction of creatinine clearance, while treatment with hemodialysis and free protein intake is associated with reduction of creatinine clearance [27].
Conclusion
The rare association of a gallbladder polyp in a bodybuilder with symptomatic uremia is reported.
Conflict of interest
None.
References
- Sand R, Mayer L., (1911), Transformation de las Vesicule Biliare tout entiere en un Ky te Papillifere. Arch de Med. Exper et d'anat Path 23:523.
- Abell I. Papilloma and Adenoma of Gallbladder. Ann Surg 1923; 77:276.
- Kirklin BR. Cholecystographic diagnosis of neoplasms of the gallbladder. Am J Roentgenol (1933); 29:8?
- Wellbrock WLA. Occurrence and possible significance of adenoma of gallbladder. Am J Surg 1934; 23:358.
- Walters W, Snell AM. Diseases of Gallbladder and Bile Ducts, Philadelphia. WB Saunder, 1940.
- Kozoll DD, Meyer KA. Gallbladder polyps. Q Bull Northwest Univ Med Sch 1957; 31(3):225-32.
- Lee KF, Wong J, Li JC, Lai PB. Polypoid lesions of the gallbladder. Am J Surg 2004 Aug; 188(2):186-90. Doi: 10.1016/j.amjsurg.2003.11.043
- Al-Mosawi AJ. The challenge of chronic renal failure in the developing world: possible use of acacia gum. Pediatr Nephrol 2002 May; 17(5):390-1. Doi: 10.1007/s00467-001-0755-4. PMID: 12042902.
- Al-Mosawi AJ. Acacia gum supplementation of a low-protein diet in children with end-stage renal disease. Pediatr Nephrol. 2004 Oct; 19(10):1156-9. Doi: 10.1007/s00467-004-1562-5.PMID: 15293039.
- Al-Mosawi AJ. The use of acacia gum in end stage renal failure. J Trop Pediatr 2007 Oct; 53(5):362-5. Doi: 10.1093/tropej/fmm033. PMID: 17517814.
- -Al-Mosawi AJ. Six-year dialysis freedom in end-stage renal disease. Clin Exp Nephrol 2009 Oct; 13(5):494-500. Doi: 10.1007/s10157-009-0181-7. PMID: 19479191.
- Al-Mosawi AJ. Continuous renal replacement in the developing world: Is there any alternative. Therapy (Clinical practice) [p-ISSN: 2044-9038, e-ISSN: 2044-9046] Mar 2006:3(2): 265-272. Doi: 10.2217/ 14750708.3.2.265
- Al-Mosawi AJ. Intestinal dialysis: A new therapy for chronic renal failure. 1st ed., Saarbrücken; LAP Lambert Academic Publishing: 2011 (ISBN: 9783847304470).
- Al-Mosawi AJ. Advances in peritoneal dialysis. In, Ed, Peritoneal Dialysis: Types, Procedures and Risks. Nova Science Publisher, New York, 1st Edition, January, 2013 (ISBN-10:1622578961, ISBN-13:978-1622578 962).Doi:10.13140/rg.2.1.4315.1120
- Al-Mosawi AJ. A new dietary therapy for chronic renal failure .1st ed., Saarbrücken; LAP Lambert Academic Publishing: 2013 (ISBN: 978-3-659-51436-4).
- Al-Mosawi AJ. Advances of peritoneal dialysis in the developing world: Combined intermittent peritoneal dialysis and intestinal dialysis (Chapter 3).In Marcia Bell, Ed, Peritoneal Dialysis: Practices, Complications and Outcomes. Nova Science Publisher, New York, 2017 (ISBN: 978-1-53610-515-5).Doi:10.13140/rg.2.1. 4315.1120
- Al-Mosawi AJ. Dietary dialysis with acacia gum: Intestinal dialysis technology. Advancements in Journal of Urology and Nephrology (ISSN 2689-8616) 2019 Nov 18; 2(1): 1-8. Doi:10.33140/AJUN.01.01.05
- Al-Mosawi AJ.A New Dietary Therapy for Chronic Renal Failure: Intestinal Dialysis Technology. Journal of medical and surgical urology Jan 2020; 1(1): 8-16. Doi: 10.5281/ zenodo.3878418
- Al-Mosawi AJ. Intestinal (Dietary) Dialysis: A Practical Nutritional Guide. Journal of Urology and research (ISSN: 2379-951X) Aug 2020; 7 (1): 1118 [1-3].
- Al-Mosawi AJ. Intestinal dialysis in a uremic patient with diabetic nephropathy: A challenging case and a unique experience. Journal of Pharmaceutical Research and Development Aug 2020; 20; 1 (1):1-4 Doi: 10.5281/zenodo.3977265
- Al-Mosawi AJ. History of Medicine: The Emergence of Intestinal Dialysis. SunKrist Nephrology and Urology Journal 2020 August 22; 2 (1): 1-8. Doi: 10.46940/snuj.01.1002
- Al-Mosawi AJ. Intestinal dietary dialysis: A practical treatment guide. 1st ed., Saarbrücken; LAP Lambert Academic Publishing: 2020 (ISBN: 978-3-659-87697-4).
- Libório AB, Nasserala JC, Gondim AS, Daher EF. The case: renal failure in a bodybuilder athlete. Diagnosis: Nephrocalcinosis secondary to exogenous vitamin D intoxication. Kidney Int 2014 May; 85(5):1247-8. Doi: 10.1038/ki.2013.230
- Walser M. Keto-analogues of essential amino acids in the treatment of chronic renal failure. Kidney Int Suppl 1978 Jun ;( 8):S180-4.
- Bauerdick H, Spellerberg P, Lamberts B. Therapy with essential amino acids and their nitrogen-free analogues in severe renal failure. Am J Clin Nutr 1978 Oct; 31(10):1793-6. Doi: 10.1093/ajcn/31.10.1793
- Giovannetti S, Barsotti G, Morelli E, Ciardella F, Mariani G, Molea N, Panicucci F, Rossi B. Insufficienza renale cronica. Dieta ipoproteica supplementata con aminoacidi essenziali e chetoanaloghi [Chronic renal insufficiency. Low-protein diet supplemented with essential amino acids and ketoanalogues]. Minerva Med 1980 Sep 19; 71(34):2415-30. [Article in Italian].
- -Barsotti G, Guiducci A, Ciardella F, Giovannetti S. Effects on renal function of a low-nitrogen diet supplemented with essential amino acids and ketoanalogues and of hemodialysis and free protein supply in patients with chronic renal failure. Nephron 1981; 27(3):113-7. Doi: 10.1159/000182036
- Carrero JJ, González-Ortiz A, Avesani CM, Bakker SJL, Bellizzi V, Chauveau P, et al. Plant-based diets to manage the risks and complications of chronic kidney disease. Nat Rev Nephrol 2020 Sep; 16(9):525-542.Doi:10.1038/s41 581-020-0297-2


