Archive : Article / Volume 2, Issue 1
Case Report | DOI: https://doi.org/10.58489/2836-2217/010
Intra Oral Plasma Cell Neoplasm: A Case Report
1 House # IH 130, street # 19, PAF Falcon Complex, Rawalpindi, Pakistan
Correspondng Author: Maidah Hanif
Citation: Sidra Ghayas, Nadia Zaib, Maidah Hanif, Fakeha Meraj. (2023). Intra Oral Plasma Cell Neoplasm: A Case Report. Journal of Clinical Case Reports and Trails. 2(1); DOI: 10.58489/2836-2217/010
Copyright: © 2023 Maidah Hanif, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2023-04-05, Received Date: 2023-04-05, Published Date: 2023-04-07
Abstract Keywords: Plasma cell, Neoplasm, Pathology
Abstract
Plasmacytomas are rare solitary soft tissue tumors that arise from proliferations of malignant transformed monoclonal plasma cells and can be diagnosed through biopsy and histopathologic examination. These lesions are closely associated with multiple myelomas, which should be ruled out in all these cases by necessary laboratory and radiographic examinations. A 41yrs old female came to surgery department with a complaint of slow-growing painless mass of 1.0 x0.5 x0.5cm at angle of the mandible. A diagnosis of solitary plasmacytoma was made on the basis of clinical, radiographic, and histopathological findings. Early diagnosis of plasmacytomas is of great importance. Radiotherapy is the common modality of treatment with or without adjuvant chemotherapy. Progression to plasma cell lesion is possible; thus, close follow-up of the patient is essential after the completion of the therapeutic procedure.
Introduction
Neoplasms containing irregular plasma cells or tumor-forming cells in the body's soft tissues or bones are known as plasma cell neoplasms. The plasma cells also make M protein, an antibody protein that does not aid in the body's ability to fight infection and is therefore not needed. Nevertheless, M Protein will significantly impact on the development of bone marrow, which could thicken the blood or damage the kidneys.
Less than 5 percent of plasma cell neoplasms are diagrammatic of solitary tumors, and further subcategories include solitary extra medullary plasmacytoma (SEP) and solitary bone tumor (SBP), depending on whether the affected location is in the bone or in soft tissue. The synthesis of monoclonal immunoglobulin by aberrant growth propagation of a single copy of plasma cells is frequently used to identify plasma cell neoplasms [1]. It is significant in solitary plasmacytoma to differentiate whether negligible bone marrow clonal plasmacytosis is seen or not: negative whole-body imaging for additional lesions, bone marrow plasma cells are vague, there is only one lesion of the bone or soft tissue, and there is no other organ damage: hypercalcemia, renal failure, anaemia, with multiple myeloma developing in 50% of patients, The axial skeleton, particularly the long bones and vertebrae, is most impacted by SPB [2]. Jaw involvements are uncommon, when they do occur, the mandible is more likely to be affected than the maxilla. When there are multiple tumors, it is called as multiple myeloma. It is infrequently seen in the jaws, where its most common sites are angle and ramus of the mandible [3]. The plasma cell neoplasms can damage the bones [4]. Common areas reported in most of the cases are in the bone marrow opulent zones of the mandible which include body, retro molar trigone angle and ramus. Here the author describes a situation of a patient who suffers with plasma cell neoplasm of the mandible.
Case Presentation
41-year-old lady without plausible general history, came along tender bump over the right angle of the mandible area, the symptoms were developing for past 6 months. On physical examination, swelling over the lower third area of the face was observed and it showed that it has expanded beyond mandible into the soft tissue on that side.
Orthopantomography revealed well corticated, multilocular, radiolucency at ramus and angle of right portion of the mandible (Fig 1).

A contrast enhanced CT scan was performed with 5mm thick slices. The CT scan revealed a 3.5 x 3.2 x 4.8cm heterogeneously enhancing lesion involving the proximal ramus and angle of the mandible. There were significant signs of cortical and bone expansion. The adjacent soft tissues were invaded by the extension of mass beyond the outline of the mandible. The lesion involved the masseter muscle laterally, medially involved the submandibular gland and anteriorly involved the buccal mucosa and base of the tongue. The CT also indicated significant finding of enlarged and prominent cervical lymph nodes. All other adjacent structures appeared to be normal (Fig 2, 3).


A differential Diagnosis was made based on the radiographic findings. The D/D included:
- Ameloblastoma
- Odontogenic keratocyst
- Aneurysmal bone cyst
- Giant cell lesion
Baseline blood investigations were advised and patient was scheduled and called for biopsy after 2 days. An incisional biopsy was performed through right lower buccal vestibule. During the biopsy procedure, profuse intra-lesional bleeding was noted which led to addition of venous malformation in the D/D.
On gross examination a single soft tissue piece measuring 1.0x0.5x0.5 cm was obtained that was embedded as such in a cassette and processed.
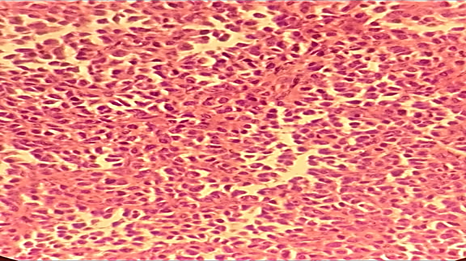
Histopathological findings of the incisional biopsy specimen revealed tissue fragments lined by stratified squamous epithelium showing squamous hyperplasia. Underlying connective tissue showed infiltration by a tumor composed of sheets of hyperchromatic and atypical plasmacytoid cells. Individual cells also had moderate degree of nuclear atypia. Findings were suggestive of a plasma cell neoplasm.
Further D/D were drawn based on the Histopathological findings. The D/Ds included:
- Myoepithelial carcinoma
- Plasma Cell tumor
- Alveolar rhabdomyosarcoma
Next, immunochemistry was advised for detailed evaluation. Tissue blocks and slides were sent to Armed Forces Institute of Pathology (AFIP) for immunohistochemical analysis. The findings were consistent with previous histological findings and also suggested a plasma cell neoplasm. The immunohistochemistry revealed:
- CD38 - diffuse positive
- CD138 - positive
- LCA -negative
- Desmin - negative
- S100 - negative
- Calponin - negative
- Ki67 - 2 %
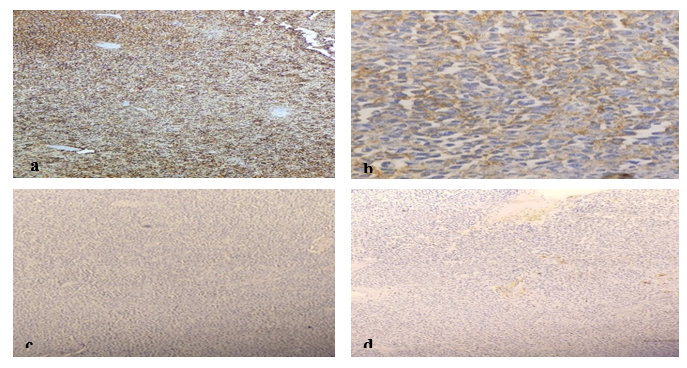
Fig 4: Immunohistochemical evaluation (a) diffuse positivity of CD38 at 4x. (b) Positive expression of CD138 at 40x (c) Negative expression of Desmin (d) low reactivity of ki67 at 4x
The patient was informed of the immunohistochemistry findings and was referred to consultant oncologist at Fauji Foundation hospital, Islamabad. Urine electrophoresis, kappa & lambda light chain restriction studies and systemic radiologic investigations were advised. The patient, however, did not return for the follow up visits and was unable to comply with further diagnostic evaluations advised. Therefore, it could not be concluded whether the mass was multiple myeloma or plasmacytoma. It was only confirmed that this was a case of plasma cell neoplasm.
Discussion
Abnormal growth of plasma cells was elaborated in detail by Dalrymple et al in 1846 [5]. Defined in literature as “a collection of clinical abnormalities identified significantly by a rigorous and without control clonal collection and growth of plasma cells”. It can be further investigated below 3 major clusters: “as Extra medullary Plasmacytomas”, or “as a significant part of Multiple Myeloma” and “as Medullary Plasmacytomas”. Plasmacytomas are abnormal growth and collection of plasma cells in a specific local area giving rise to a tumor mass of that very area, that can be further divided into two more categories based on the type.
- “Extra medullary plasmacytoma (EMP) with soft tissue involvement”
- “Solitary plasmacytoma with single bone involvement (SPB)”
Multiple Myeloma, which denotes the most significant and often occurring plasma cell dyscrasia, can also include this site-specific collecting and development of monoclonal plasma cells [6]. A single immunoglobulin is produced by highly categorized lymphocytes through a high collection and abnormal growth, categorically in multiple myelomas. So, it is identified by the greatly spread monoclonal excessive formation of immunoglobulins in the blood or by noticing Bence Jones proteins in urine. Multiple myeloma eventually manifests in 80- 85 % of the patients, who have a history of medullary plasmacytomas whereas the extra medullary plasmacytoma remains bounded to the place of initial occurrence. Plasmacytoma commonly presents in age groups 0f 50-80 years [7]. Such cases can present clinically as, pain in the bones, restricted bulge of the involved part or distinguishable density on the side lying structures. Solitary bone plasmacytomas typically seem in the bones of pelvis, ribs, vertebrae and pectoral girdle while extra medullary plasmacytomas usually seem on the mucosal surfaces e.g. oropharynx, nasal sinuses, larynx etc [8]. These tumors appear to have well-defined plasma cells with tiny eccentric nuclei and coarse chromatin that is reduced to the sides on histological slides. Immature plasma cells screening excellently detached nuclear chromatin in eccentric nuclei obligating prominent nucleoli and copious cytoplasm can also be seen in these tumor presentations. The occurrence rate of plasma cell neoplasm’s is approximately 2.59 to 3.31 per lac populace and complex incidences are identified in population of African- American foundation. About three to ten percent of plasma cell neoplasms are solitary bone plasmacytomas [9]. Plasmacytomas very rarely occur in mandible/jaws as a probable area in the head and neck. Plasmacytomas happen owing to clonal collection of plasma cells that look like myeloma cells cytologically and immunophenotypically. These disease symptoms present differently in diverse groups of patients with regard to location, spread of the tumor and general existence percentage; though these patients have countless alike biologic aspects of other plasma cell diseases. Plasma cells form osteoclasts triggering factor which leads to bone resorption due to growth and excessive formation of osteoclasts [10]. Hence, radiographically, these pasmacytoma’s seem as multi-locular radiolucency deprived of any significant hard tissue production. Clinical signs of skeletal plasmacytomas include radiolytic lesions covering any part of the skeleton, clonal plasma cell infiltrates, and the absence of diffuse bone marrow involvement [11]. An existing criterion for diagnosis of solitary plasmacytoma is:
- “Destructed area of bone which is isolated due to clonal plasma cells”
- “Nucleated cells Absence of further osteolytic lesion or other tissue involvement”
- “Bone marrow plasma cell infiltration not exceeding 5% of all”
- “No anemia”
- “No hypocalcaemia or renal involvement”
- “A bone solitary plasmacytoma is a distinct type of plasma cell neoplasm”.
The possible sites might be the bone or the extra medullary area within the bone. Extra medullary plasmacytomas accounts below 3 percent of cancer of all the plasma cell. Approximately eighty to ninety percent of extra medullary plasmacytoma’s appear in the head and neck section. Of these almost twenty percent advanced to become multiple myeloma. Only 4.5% of solitary plasmacytoma’s endure bound to the mandibular area/jaw particularly in the bone marrow rich parts which are angle, the body and ramus of the mandible. Plasma cell tumors generally happen in the age group of fifty -eighty years. Patients spotted at age below Sixty years had ominously improved survival of five years (90% for patient’s aged 0-thirty years & 80% for patient’s thirty-fifty-nine years). When associated to patients identified at age more than sixty years (5 year existence rate is 45%) [12]. Skeletal plasmacytoma patients had an overall survival rate of 57% in 5 years and 37% in 10 years.
The Differential and Provisional diagnosis measured due to the obliteration & wide tissue mass were Peripheral Neuroectodermal tumors, Lymphomas, Ewing’s sarcomas, Histocytomas, Rhabdomyosarcomas and Neruoblastomas. Although there is no known initial lesion that implies a malignant lesion however, Histocytomas and Sarcomas often grow in younger people [13]. But the possibility of the violent presence could not be omitted due to the hostile presence of the lesion. Plasmacytomas are clinical objects where it is very problematic to authorize the analysis deprived of supportive undercover modalities.
In the current case along with histopathological, radiological conclusions, support of immunohistochemistry (IHC) positivity for CD138 aided in reaching the final diagnosis. Solitary plasmacytomas are extremely radiosensitive lesions. Radical extensive surgery or radiation therapy, or a combination of these both is suggested as primary treatment [14]. Radical radiation of 40 to 50 Gy has demonstrated 80% local disease control.
Recently researches are being going on for the role of thalidomide, protease inhibitors angiogenesis inhibitors, or inhibitors of vascular endothelial growth factors in plasma cell neoplasm’s as substitute method of treatment [15].
Conclusion
In order to reach a definitive diagnosis about the type of plasma cell neoplasm, systemic investigations and urine electrophoresis are required. In our case patient was referred for further investigations but unfortunately, she did not return for the follow up.
Plasma cell neoplasm barely occur in maxillofacial areas affecting mandible. It is nearly impossible to reach a diagnosis based solely on clinical presentation or examination. Histopathologists may play an integral role effectively providing the foundation on which definitive diagnosis is structured.
References
- Marotta S, Di Micco P. Solitary plasmacytoma of the jaw. J Blood Med. 2010;1:33.
- Kaur H, Parhar S, Kaura S, Bansal S, Jawanda M, Madhushankari GS, et al.( 2013) A large painless swelling of the posterior mandible. Oral Surg Oral Med Oral Pathol Oral Radiol. 115(2):152–6.
- Souza LN, Farias LC, Santos LAN, Mesquita RA, Júnior HM, De-Paula AMB. (2007)Asymptomatic expansile lesion of the posterior mandible. Oral Surgery, Oral Med Oral Pathol Oral Radiol Endodontology. 103(1):4–7.
- Rapidis AD, Givalos N, Gakiopoulou H, Stavrianos SD, Faratzis G, Lagogiannis GA, et al. (2007)Mucoepidermoid carcinoma of the salivary glands.: Review of the literature and clinicopathological analysis of 18 patients. Oral Oncol. 43(2):130–6.
- An SY, An CH, Choi KS, Heo MS. (2013)Multiple myeloma presenting as plasmacytoma of the jaws showing prominent bone formation during chemotherapy. Dentomaxillofacial Radiol. 42(4):20110143.
- Boffano P, Viterbo S, Barreca A, Berrone S. (2011)Pathologic mandibular fracture as the presenting manifestation of multiple myeloma. J Craniofac Surg.22(4):1312–5.
- Elias HG, Scott J, Metheny L, Quereshy FA. (2009)Multiple myeloma presenting as mandibular ill-defined radiolucent lesion with numb chin syndrome: a case report. J oral Maxillofac Surg. 67(9):1991–6.
- Ho CL, Chen YC, Yiang YT, Kao WY, Chao TY. (1999)Mandibular mass as the presenting manifestation of IgM myeloma in a 22-year-old man. Ann Hematol. 78(2):93–5.
- Nofsinger YC, Mirza N, Rowan PT, Lanza D, Weinstein G. (1997)Head and neck manifestations of plasma cell neoplasms. Laryngoscope. 107(6):741–6.
- Baad R, Kapse SC, Rathod N, Sonawane K, Thete SG, Kumar MN. (2013)Solitary plasmacytoma of the mandible–a rare entity. J Int oral Heal JIOH. 5(3):97.
- Sher T, Miller KC, Deeb G, Lee K, Chanan‐Khan A. (2010)Plasma cell leukaemia and other aggressive plasma cell malignancies. Br J Haematol. 150(4):418–27.
- Lorsbach RB, Hsi ED, Dogan A, Fend F. Plasma cell myeloma and related neoplasms. Am J Clin Pathol. 2011;136(2):168–82.
- Kyriazidou A, Brown PJ, Lucke VM. (1989)An immunohistochemical study of canine extramedullary plasma cell tumours. J Comp Pathol. 100(3):259–66.
- Vasef MA, Medeiros LJ, Yospur LS, Sun NC, McCourty A, Brynes RK. (1997)Cyclin D1 protein in multiple myeloma and plasmacytoma: an immunohistochemical study using fixed, paraffin-embedded tissue sections. Mod Pathol an Off J United States Can Acad Pathol Inc. 10(9):927–32.
- Boo K, Cheng S. (1992)A morphological and immunohistochemical study of plasma cell proliferative lesions. Malays J Pathol. 14(1):45–8.
- Nowrousian MR, Brandhorst D, Sammet C, Kellert M, Daniels R, Schuett P, et al. (2005;)Serum free light chain analysis and urine immunofixation electrophoresis in patients with multiple myeloma. Clin cancer Res. 11(24):8706–14.


