Article In Press : Article / Volume 3, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/2836-3604/013
COVID-19 in a hemodialysis center
1Nephrology department Beni Messous hospital Algiers.
2Epidemiology department Beni Messous hospital Algiers.
Samia ZITOUNI*
Samia ZITOUNI, Ghania BRAHIMI, Messaoud SAIDANI. (2024). COVID-19 in a hemodialysis center. Covid Research and Treatment. 3(1); DOI: 10.58489/2836-3604/013
© 2024 Samia ZITOUNI, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 01-07-2024
- Accepted Date: 10-07-2024
- Published Date: 20-07-2024
Acute kidney disease, Chronic kidney disease, Chronic hemodialysis, Mortality, COVID-19
Abstract
Background: Acute renal failure in hospitalized patients with SARS-CoV-2 infection was associated with high in-hospital mortality. Chronic renal failure (CRF) was a risk factor for a more severe form of COVID-19 disease. Our work investigated mortality in the renal failure population with COVID19 and the course of renal function.
Methods: A single-center retrospective study of 231 patients with COVID-19 who required dialysis was conducted. 3 groups of patients were constituted according to the type of renal failure, Group 1: acute renal failure (ARF), Group 2: CRF with deteriorating renal function (ARF+CRF) and Group3: chronic hemodialysis (HD), all required hemodialysis sessions. Overall mortality and in each group were calculated. Finally, the evolution of renal function among the survivors was studied.
Results: An overall mortality rate of 52.4% was found. The age of the deceased patients was higher than
the age of survivors (64.67±13.19 years vs 57.68±15.58 years). Male sex and the degree of pulmonary involvement of COVID-19 lung disease were significant risk factors (p=0.0006, p=0.00003 respectively) Type II diabetes and underlying respiratory pathology were the main comorbidities related to mortality with rates of 63.21% and 60.90% respectively.
Group1 had the highest mortality rate (75.6%) compared to 46.5% in Group3. Mortality in the Group 2 and 3 was 47.4% and 46,5% respectively. The recovery of renal function in Group1 was 24.44%. In Group2 100% of patients with creatinine clearance above 30ml/min returned to baseline function compared to only 9.09% when clearance was below 30ml/min.
Conclusion: Renal failure requiring dialysis is a risk factor for COVID-19-related mortality
Introduction
The new coronavirus (SARS-CoV-2) was responsible for a life-threatening pandemic disease. Most published studies describe acute kidney injury (AKI) in patients with no history of renal failure. Data on the prevalence of AKI in hospitalized patients with COVID-19 range from 0.5% to 46%【3,4,5】. Available data indicate a strong association between AKI and mortality【6,7】.
There are far fewer reports on the evolution of COVID-19 in patients with chronic renal failure (CRF) on admission to the hospital, but the risk of developing severe COVID-19 in patients with chronic kidney disease (CKD) is high, according to several studies【8,9】
With regard to chronic hemodialysis, studies carried out in China, Italy, the United Kingdom, and the United States (New York and Southern California) indicate that chronic dialysis patients suffering from COVID-19 have a higher mortality rate and a more severe form of the disease than the general population【10,11】.
The aim of our study was to determine the mortality of patients with COVID-19 who required hemodialysis in our center (COVID-19 unit). These patients were either chronic hemodialysis patients with chronic kidney disease (CKD) or patients who developed AKI within the hospital. We also monitored the evolution of renal function in survivors.
Materials and Methods
This is a retrospective observational monocentric study which included 231 patients requiring dialysis in our hemodialysis center, COVID-19 unit, over a two-year period from March 2020 to February 2022.
These were COVID-19 patients hospitalized in our hospital who required hemodialysis sessions due to severe acute kidney injury (AKI), severe AKI on a background of chronic kidney disease (CKD), or they were chronic hemodialysis (HD) patients.
Our population was divided into three distinct groups of patients:
Group 1: Patients with acute kidney injury (AKI).
Group 2: Patients with chronic kidney disease (CKD) who experienced worsening renal function (AKI on CKD).
Group 3: Chronic hemodialysis (HD) patients.
The diagnosis of COVID-19 was confirmed either by a positive Polymerase Chain Reaction (PCR) test and/or a positive antigen (Ag) test and/or the presence of lung lesions on a chest CT scan suggestive of COVID-19 pneumonia.
The risk factors for mortality studied were age, sex, history of hypertension (HTN), type I and type II diabetes, cardiovascular disease, underlying respiratory pathology, obesity, and current cancer.
Creatinine clearance was calculated using the MDRD (Modification of Diet in Renal Disease) formula.
Mortality in this study was directly related to COVID-19 either through the severity of pulmonary involvement or thrombo-embolic complications.
Renal function in survivors was monitored by a renal check-up performed every 3 days.
The analytical study of the results was conducted using EpiDATA and all experimental protocols and procedures followed comply with international standards for ethical research.
Results
We collected data from 231 patients, of whom 45 (19.5%) were in Group 1, 57 (24.7%) were in Group 2, and 129 (55.8%) were in Group 3, all requiring hemodialysis sessions at our center. All patients were adults (>18 years old), with a mean age of 61.34 ± 14.76 years and ranging from 18 to 90 years. Among them, there were 140 males and 91 females (sex ratio 1.5:1).
75% of the patients were hypertensive, 44.6% had type II diabetes, 6.92% had type I diabetes, 26.5% had underlying cardiovascular disease, 20.4% were obese, underlying respiratory pathology was present in 10%, and cancer was present in 6.1% of the patients. Lung involvement on chest CT scan was mild (10-25%) in 35.70% of the patients; moderate (25-50%) in 32.40%; severe (50-75%) in 18.70%; and critical (>75%) in 13.20%. The overall mortality rate was 52.4%.
The average age of deceased patients was 64.67 ± 13.19 years compared to 57.68 ± 15.58 years for survivors.
We calculated the mortality rate in the 3 groups of patients, which was 75.6% in Group 1, 47.4% in Group 2, and 46.5% in Group 3 (Figure 1)
Regarding the evolution of renal function in Group 1, where we noted the survival of 11 patients (24.44%) (Table 1), it was favorable with complete recovery in 8 out of 11 patients (72.72% of cases). Only one patient (postpartum vascular NP) transitioned to chronic hemodialysis after the failure of specific treatment. The two patients with cardiorenal syndrome progressed to chronicity.
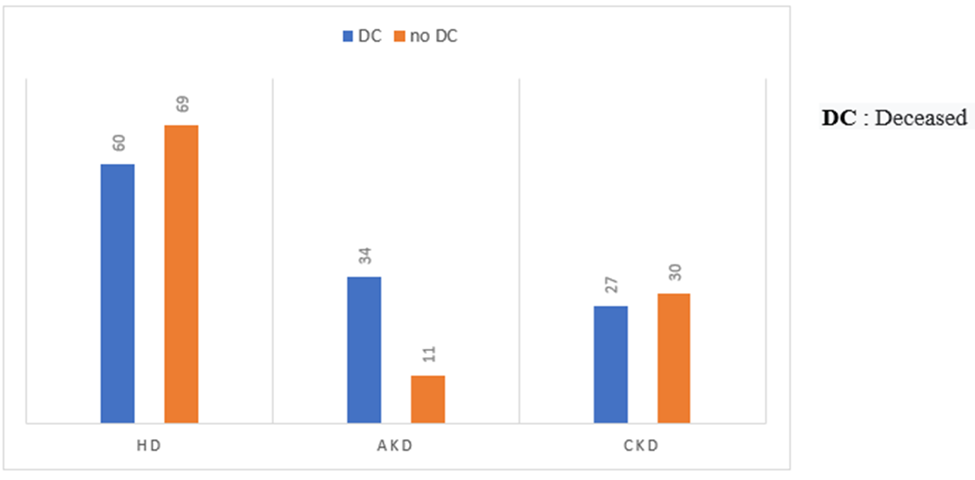
Fig 1: the mortality rate in the 3 groups of patients
Table 1: Characteristics of Group 1 patients who survived
| Sex | Age | Atecedants | Covid-19 Diagnosis | AKD etiology |
| F | 65 | HTN DII DR leg ulcer | 10% | Severe sepsis |
| M | 45 | cardiac decompensation DCM | 25% | CRS I |
| M | 60 | BPH | 10% | Obstructive |
| M | 68 | HTN COPD | 10-25% | Functional |
| M | 87 | HTN BPH | 10-25% | Obstructive+ APN |
| M | 60 | HTN stented heart disease | 10-25% | CRS I |
| F | 85 | Hypothyroidism | Ag Test + | Obstructive |
| M | 22 | DI Fulminant hepatitis | Ag Test+ | Uremic cholangitis |
| M | 77 | Metastatic prostate neoplasia | Ag Test + | Obstructive |
| M | 52 | Urinary tract infection on malformative uropathy | Ag Test + | Obstructive |
| F | 38 | Post-partum AKD | Ag Test+ | Vascular NP before COVID-19 |
AKD : Acute kidney disease HTN:Hypertension DII: Type II diabetes DR :Diabetic retinopathy DCM :Dilated cardiomyopathy CRS I Type I cardiorenal syndrome BPH: Benign prostatic hypertrophy COPD: Chronic obstructive pulmonary disease APN:Acute pyelonephritis Ag test: Antigenic test DI: Type I diabetes NP:Nephropathy
In Group 2, 30 out of 57 patients survived; among them, 18 patients with a baseline creatinine clearance greater than 30 ml/min all regained their baseline renal function. In contrast, among the 12 patients with a baseline creatinine clearance less than 30 ml/min, only 1 patient showed partial recovery, and hemodialysis was discontinued for him. The remaining patients were all diagnosed with end-stage renal disease.
Discussion
During our study, we found an overall mortality rate of 52.4%, which was higher compared to the overall mortality rate in the general population in Algeria, which was 2.5% during the same period [12]. This suggests that renal failure requiring dialysis is a significant risk factor for COVID-19-related mortality. This finding is consistent with several published studies that have found that chronic kidney disease and acute kidney injury increase the risk of mortality in patients with COVID-19 [2].
Age was a significant risk factor for mortality. We found that the age of deceased patients (64.67 ± 13.19 years) was significantly higher than the average age of the studied population (61.34 ± 14.76 years) and the average age of survivors (57.68 ± 15.58 years).
Male sex and the degree of lung involvement of COVID-19 on thoracic CT scan were also significant risk factors with p-values of 0.0006 and 0.00003, respectively. Medical history of type II and type I diabetes, cardiovascular disease, hypertension (HTN), respiratory disease, current cancer, as well as obesity, all constituted mortality factors with significance levels of p=0.01, p=0.02, p=0.21, p=0.23, p=0.39, p=0.35, p=0.15, respectively.
Several published studies have analyzed the same risk factors for mortality in patients with COVID-19 and have found a strong association between comorbidities and mortality. A meta-analysis of 42 studies, including 423,117 patients, found that acute kidney injury, underlying respiratory disease, diabetes, hypertension, cardiovascular disease, cancer, elevated D-dimers, as well as male sex, advanced age, current smoking, and obesity are clinical risk factors for a fatal prognosis associated with coronavirus [13].
Furthermore, the highest mortality was found in Group 1 at 75.6%. Acute kidney injury (AKI) is a major factor in mortality found in several studies. A study conducted in the United States on 9,657 patients in 13 hospitals compared in-hospital mortality rates among patients without AKI, with AKI stages 1 to 3 not requiring dialysis, and AKI stage 3 requiring dialysis, with mortality rates of 7.3%, 46.4%, and 79.3%, respectively [14]. The development of AKI is associated with disease severity, longer hospital stays, and high mortality [15].
The analysis of results from our AKI patients who survived (11 out of 45) revealed that there was another cause, other than COVID-19, that could explain this AKI (see Table 2), and in fact, 100% of patients who experienced AKI directly linked to COVID-19 all died. It is noteworthy that among the survivors in this group, the lung involvement of COVID-19 was either mild or absent (see Table 2), which could explain the better prognosis of these patients.
Group 2 exhibited a mortality rate of 47.4%. No published study has calculated this mortality rate to compare our results, but according to a study conducted in China, hypertension (HTN) and type II diabetes, which are the main causes of chronic kidney disease (CKD), along with the cardiovascular risk they pose, are risk factors for exacerbating COVID-19 pathology [16]. Acute kidney injury (AKI) superimposed on CKD is a significant predictor of poor prognosis in COVID-19 patients, more so than the baseline level of CKD [17].
Among the survivors in Group 2, all 18 patients who had a baseline creatinine clearance > 30 ml/min were successfully weaned off hemodialysis, compared to only one patient out of the 12 patients with a baseline creatinine clearance < 30>
Finally, among the chronic hemodialysis patients (Group 3), we noted a mortality rate of 46.5%, comparable to that of Group 2. A study in Turkey found that the difference in mortality between CKD and HD was not significant when comorbidities and the severity of COVID-19 were comparable [18]. However, this rate is high compared to previous study results. A study in the United States found a mortality rate of 24.9% [19], while another study in China found a mortality rate of 25.5% [20]. Further studies are therefore necessary to explain this difference.
Conclusion
Our study found that patients with kidney disease requiring dialysis are at a high risk of mortality associated with COVID-19 regardless of the type and/or stage of their kidney disease, but this risk is particularly pronounced in cases of severe acute kidney injury (AKI). The baseline creatinine clearance of CKD patients is a determining factor for renal function evolution in chronic kidney disease patients post-COVID-19.
References
- Ahmadian, E., Hosseiniyan Khatibi, S. M., Razi Soofiyani, S., Abediazar, S., Shoja, M. M., Ardalan, M., & Zununi Vahed, S. (2021). Covid‐19 and kidney injury: Pathophysiology and molecular mechanisms. Reviews in medical virology, 31(3), e2176.
- Kellum, J. A., van Till, J. O., & Mulligan, G. (2020). Targeting acute kidney injury in COVID-19. Nephrology Dialysis Transplantation, 35(10), 1652-1662.
- Liakopoulos, V., Roumeliotis, S., Papachristou, S., & Papanas, N. (2022). COVID-19 and the kidney: time to take a closer look. International Urology and Nephrology, 54(5), 1053-1057.
- Chan, L., Chaudhary, K., Saha, A., Chauhan, K., Vaid, A., Zhao, S., ... & Nadkarni, G. N. (2021). AKI in hospitalized patients with COVID-19. Journal of the American Society of Nephrology, 32(1), 151-160.
- Bowe, B., Cai, M., Xie, Y., Gibson, A. K., Maddukuri, G., & Al-Aly, Z. (2021). Acute kidney injury in a national cohort of hospitalized US veterans with COVID-19. Clinical Journal of the American Society of Nephrology, 16(1), 14-25.
- Marques, F., Gameiro, J., Oliveira, J., Fonseca, J. A., Duarte, I., Bernardo, J., ... & Lopes, J. A. (2021). Acute kidney disease and mortality in acute kidney injury patients with COVID-19. Journal of Clinical Medicine, 10(19), 4599.
- Rahimzadeh, H., Kazemian, S., Rahbar, M., Farrokhpour, H., Montazeri, M., Kafan, S., ... & Razeghi, E. (2021). The risk factors and clinical outcomes associated with acute kidney injury in patients with COVID-19: data from a large cohort in Iran. Kidney and Blood Pressure Research, 46(5), 620-628.
- Brogan, M., & Ross, M. J. (2022). The impact of chronic kidney disease on outcomes of patients with COVID-19 admitted to the intensive care unit. Nephron, 146(1), 67-71.
- Henry, B. M., & Lippi, G. (2020). Chronic kidney disease is associated with severe coronavirus disease 2019 (COVID-19) infection. International urology and nephrology, 52, 1193-1194.
- Xiong, F., Tang, H., Liu, L., Tu, C., Tian, J. B., Lei, C. T., ... & Zhang, C. (2020). Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. Journal of the American Society of Nephrology, 31(7), 1387-1397.
- Sim, J. J., Huang, C. W., Selevan, D. C., Chung, J., Rutkowski, M. P., & Zhou, H. (2021). COVID-19 and survival in maintenance dialysis. Kidney medicine, 3(1), 132-135.
- Bulletin N°262 de l’Institut National de Santé publique Algérie publié 25 Février 2022.
- Dessie, Z. G., & Zewotir, T. (2021). Mortality-related risk factors of COVID-19: a systematic review and meta-analysis of 42 studies and 423,117 patients. BMC infectious diseases, 21(1), 855.
- Ng, J. H., Hirsch, J. S., Hazzan, A., Wanchoo, R., Shah, H. H., Malieckal, D. A., ... & Uppal, N. N. (2021). Outcomes among patients hospitalized with COVID-19 and acute kidney injury. American Journal of Kidney Diseases, 77(2), 204-215.
- Lowe, R., Ferrari, M., Nasim-Mohi, M., Jackson, A., Beecham, R., Veighey, K., ... & Dushianthan, A. (2021). Clinical characteristics and outcome of critically ill COVID-19 patients with acute kidney injury: a single centre cohort study. BMC nephrology, 22, 1-9.
- Zhou, Y., Ren, Q., Chen, G., Jin, Q., Cui, Q., Luo, H., ... & Li, X. (2020). Chronic kidney diseases and acute kidney injury in patients with COVID-19: evidence from a meta-analysis. Frontiers in medicine, 7, 588301.
- Kilis-Pstrusinska, K., Akutko, K., Braksator, J., Dancewicz, A., Grosman-Dziewiszek, P., Jamer, T., ... & Jankowska, E. A. (2021). Kidney dysfunction and its progression in patients hospitalized duo to COVID-19: Contribution to the clinical course and outcomes. Journal of Clinical Medicine, 10(23), 5522.
- Ozturk, S., Turgutalp, K., Arici, M., Odabas, A. R., Altiparmak, M. R., Aydin, Z., ... & Ates, K. (2020). Mortality analysis of COVID-19 infection in chronic kidney disease, haemodialysis and renal transplant patients compared with patients without kidney disease: a nationwide analysis from Turkey. Nephrology Dialysis Transplantation, 35(12), 2083-2095.
- Hsu, C. M., Weiner, D. E., Aweh, G., Miskulin, D. C., Manley, H. J., Stewart, C., ... & Lacson Jr, E. (2021). COVID-19 among US dialysis patients: risk factors and outcomes from a national dialysis provider. American Journal of Kidney Diseases, 77(5), 748-756.
- Fisher, M., Yunes, M., Mokrzycki, M. H., Golestaneh, L., Alahiri, E., & Coco, M. (2020). Chronic hemodialysis patients hospitalized with COVID-19: short-term outcomes in the Bronx, New York. Kidney360, 1(8), 755-762.


