Archive : Article / Volume 1, Issue 1
Case Report | DOI: https://doi.org/10.58489/2836-2292/003
The integration of strategic management into functional units of primary health care: the case of the health centers grouping âentre douro e vouga ii â aveiro norte
Department: EEG - Escola de Economia e Gestão â Phd Student University/Organisation: Universidade do Minho - Escola de Economia e Gestão, Portugal.
Correspondng Author: Paula Cristina de Almeida Marques
Citation: Paula Cristina de Almeida marques (2022). The Integration Of Strategic Management Into Functional Units Of Primary Health Care: The Case Of The Health Centers Grouping âEntre Douro E Vouga Ii â Aveiro Norte. Journal of Hospital and Clinical Management. 1(1). DOI:10.58489/2836-2292/003
Copyright: © 2022 Paula Cristina de Almeida Marques this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2022-10-17, Received Date: 2022-10-17, Published Date: 2022-12-12
Abstract Keywords: Strategic Management, Balanced Scorecard, Primary Care, Functional Units, Case Study
Abstract
The aim of this study is to analyze how Strategic Management is applied in Functional Units of Primary Health Care, namely, to verify the usefulness of the Balanced Scorecard (BSC) in Functional Units of Primary Health Care (PHCU).
A qualitative methodological approach was adopted using the case study method, which allows for a holistic analysis of the phenomenon in question. The work was elaborated from the bibliographical research on the health activity and on performance systems, specifically the Strategic Management, culminating with the practical application of the Strategic Map to two PHCU of the Health Centers Grouping (ACES) of Aveiro Norte.
The results observed in the five perspectives of the BSC show that there is linearity in the PHCU of São João and Calâmbria. Its application to each one can integrate the performance management process, also serving additional functions, such as the communication of priorities, the allocation of resources, the definition of goals, the performance evaluation and the strategic control. In this context, the application of the BSC will allow the crossing of key areas for the PHCU.
Introduction
Primary Health Care (PHC) is the first level of contact between the individual, the family and the community with the health system, allowing assistance as close as possible to the places where the population lives and works. This health care is a fundamental aspect of economic and social development, and is of great importance in our socio-political domain. Thus, we can say that there is a high need to strengthen the PHC, thus reducing the unnecessary demand for care in hospitals, something that entails increased costs for the National Health System (NHS).
The management of the PHC's Functional Units (FU) needs to be carefully evaluated taking into account the technical and social importance of their performance. So, despite recognizing the global complexity of the problem, let's address the Balance Scorecard more specifically. In essence, the issue is centered on the need to better correspond to the rights and duties of citizens and the effective quality of the PHC that are an integral part of the health system, as well as the global social and economic development of the community.
The challenge that we set ourselves, concerns the realization of a work of institutional scope, with the object of carrying out a case study to the ACES of Entre Douro e Vouga II – Aveiro Norte (EDVII-II), intending to assess the importance of application of the BSC to two of the FUs of the ACES adduct.
Initially, the BSC was proposed as a performance assessment tool, and as its potential became evident, the concept quickly evolved into a performance management system (Ahrens, 2017). Thus, according to Ferreira (2010), the BSC is no longer seen as a mere organizational performance assessment tool, to become an integral part of the management process of that performance, serving additional functions, particularly, the communication of priorities, resource allocation, goal setting, performance evaluation and strategic control.
That said, it became important to answer the following questions:
- What is our image to funders?;
- How should we be seen by our users?;
- What processes will we have to excel at?; and,
- How can we develop capacities for change and growth?
However, creating the cause-effect link between performances and indicators is one of the most complex aspects that must be implemented in a BSC. Once this difficulty is overcome, we will obtain a system that articulates the strategy, allows communication between all the different players and promotes a constant articulation of the strategy with the surrounding ACES environment in question.
Perhaps it presents itself as an essential tool for PHC s, the connection of the BSC with these institutions is still presented as timid and incipient since the ACES are complex systems, composed of different services, sectors and departments with a multiplicity of professional groups and, as such, where a panoply of interpersonal relationships of a complex nature occur. In this context, the PHCs must be organized and designed so that there is quality in services, cost reduction and more information and consistent results.
Although PHC management has similarities with the management of any other service company, especially at the financial level, there are key differences that distinguish one from the other. Any manager is permanently concerned with the achievement of the established objectives and, in a BSC vision, this depends on the optimisation of the four perspectives: financial, customers, internal processes, and learning.
Over time, the BSC assumed itself as the most developed tool for the promotion of performance due to its "ability to align, integrate and interact with other improvement methodologies, creating a strategic control panel adaptable to any type of organisation" (Pinto, 2007), regardless of being a company, a non-profit organisation or any public service.
Thus, we intend with a study of Family Health Units (FHU) ─ Study of two cases - to understand the performance trends in order to assess this new management model and its repercussion on healthcare provision. The two FHUs used in this study are the FHU model B - São João, in São João da Madeira, and the FHU model A - USF Calâmbria in Vale de Cambra.
1. Theoretical Foundation
1.1. Evolution of Health Centers in Portugal
In 2005, the start was signalled for the change in PHC based on the focus on the citizen, the connection to the reality of the country, autonomy, multidisciplinarity and integration. In that year, the Council of Ministers created the Mission for Primary Health Care (MCSP) "with the nature of a mission structure, to conduct the overall project of launching, coordinating and monitoring the strategy of reconfiguring health centres and implementing family health units" (Marques, 2015).
The main objectives of the Mission for PHC were to improve the healthcare provided, its quality and continuity, as well as the efficiency and increased satisfaction of professionals and users. To this end, it was considered necessary to modernise and reconfigure the PHCs following certain principles, namely: community orientation, organisational and management flexibility, debureaucratisation, teamwork, autonomy and accountability, continuous quality improvement, and contractualisation and assessment (Gonçalves et al., 2006).
In this sense, the ACES became a vehicle to achieve this goal and are defined as public health services, with administrative autonomy, decentralised from the respective Regional Health Administrations (ARS), but under their management power, and composed of several units. Thus, their mission is to guarantee the provision of PHC to the population of a given geographical area and they comprise several functional units: the Functional Public Health Units (PHUs), the Shared Resources Units (PUs), the Community Care Units (CCUs), the Personalized Health Care Units (PHCUs) and the Family Health Units (FHUs). There are also Management Support Units (MUAG) to support the Executive Director, the Executive Board, the Clinical Board and the Community Council of the Health Centre Cluster (ACES) (Biscaia & Heleno, 2017).
This reorganization implied a profound change in the structure and operation of services and, consequently, in the management of their human resources. Currently, the paradigm of Person-Centred Medicine (PCM) has gained special status, a concept that fully takes into account the needs, concerns and experiences of each user in his/her relationship with health and is starting to be assumed as central to clinical practice. These facts imply the need for a more integrative and comprehensive model that fills gaps in the relationship between the user and the professionals, beyond the aspects essentially related to the disease, which opens a more effective way to fight against the dehumanisation of medicine.
The degree of satisfaction of all parties involved clearly improves, since better adherence to therapy, reduced anxiety and complaints about malpractice, and lower health costs are presented as very positive consequences (Branco & Ramos, 2001). It is not surprising, therefore, that better results are obtained due to greater efficiency in the provision of health care provided to the population.
1.1.1. Family Health Units
The process of change to the "new health centres" would include the establishment of FHUs, the creation of ACESs, the introduction of a new management model, the establishment of clinical governance and the reorganisation of support services, namely the deactivation of health sub-regions.
As basic individual and family healthcare units, FHUs are based on multiprofessional teams made up of doctors, nurses and administrative staff. The classification of a FHU at a given level is determined by the fulfilment of criteria in the following areas of differentiation: the degree of organisational autonomy, the differentiation of the professionals' remuneration and incentives model, and the financing model and respective legal status.
According to Decree Law no. 298/2007, 22 August, which approves the organic structure of the FHU, the models are characterised as follows:
- Model A: corresponds to a learning and improvement phase of the work in family health teams; comprises FHUs in the public administrative sector with rules and remunerations defined by the Public Administration, applicable to the sector and to the respective careers of the professionals that integrate them and with the possibility of contracting an additional portfolio of services, paid on an overtime basis, as well as contracting the fulfilment of goals, which translates into institutional incentives to revert to USFs;
- Model B: indicated for teams with greater organisational maturity, where family health teamwork is an effective practice, and should be willing to accept a more demanding level of performance contractualisation and a participation in the FHU accreditation process, within a maximum period of three years; covers FHUs in the public administrative sector; They have a special remuneration scheme for physicians integrating a base remuneration, supplements and compensation for performance and financial incentives for nurses and clinical secretaries, according to the results obtained by the respective professional team; like model A, they contract incentives related to institutional incentives and the possibility of contracting an additional portfolio of services is foreseen;
- Model C: experimental model, to be regulated by a specific statute, with a supplementary nature in relation to possible shortcomings demonstrated by the NHS, with the FHU to be created being defined according to quotas established by the regional health administrations and in view of the existence of citizens without an allocated family doctor; it covers FHU in the social, cooperative and private sectors, in articulation with the health centre, but without any hierarchical dependence on the latter, basing its activity on a programme-contract established with the Regional Health Administration.
However, currently, there are only FHU models A and B.
FHUs are, therefore, an integral part of the ACES, and their activity is developed with organizational, functional and technical autonomy, integrated in a network with other functional units of the health centre or the Local Health Unit (LHU). Their mission is to ensure the provision of personalized health care, without neglecting the objectives of efficiency, quality and accessibility; and they are subject to an objective and permanent evaluation process, with a view to continuous improvement and the achievement of health gains.
Thus, these units are formatted to provide care to a number of users ranging from four to eighteen thousand and the lists of users per doctor are calculated in Weighted Units (UP). In the FHUs, each doctor should be responsible for a minimum list of one thousand nine hundred and seventeen PU, which corresponds to an average of one thousand five hundred and fifty users (Branco & Ramos, 2001).
Normative Dispatch no. 24100/2007 establishes that the criteria and methodology that allow classifying the FHU in these models are developed by the MCSP in conjunction with the ARS and the Institute for Health Informatics and Financial Management (IGIFS).
1.2. Contracting in primary health care: process and performance indicators
The contractualisation process in primary care values the multidimensional performance of the institutions and is based on health care contracting, organised into two sub-processes:
1. External contracting, carried out between the Regional Health Authorities (ARS) and the respective Primary Health Care Units (ACES), formalized by the negotiation of Performance Plans (PD) and the signing of Programme Contracts (PC).
2. Internal contractualization, performed between the CHAs and the respective FHUs, formalized by the negotiation of the Action Plans and the signing of the Letters of Commitment.
The Executive Directors and the Clinical and Health Boards of the ACES take full responsibility for the internal contracting process with the FUs, and the Regional Health Authorities' Contracting Departments are responsible for monitoring the quality and coherence of the processes, ensuring their adequacy and technical robustness.
The external and internal contracting processes are dynamic and interdependent, with a clear and prior alignment with the National, Regional and Local Health Plans, and the design of the process begins in December and is completed by March of the following year.
The internal contracting in ACES covers all its functional units (FHU, UPHC, CCU, URAP and USP), having the same conceptual and methodological framework, namely:
- It is based on the Local Health Plan and the definition of the Local Health Profile;
- It requires the negotiation of a three-year Action Plan with annual goals; and
- It considers the specificities of the different service portfolios of the UFs.
Monitoring and evaluation are operationalized through a Global Performance Index (IGD).
The diversity, both in the contexts of care provision of each FU typology, and in their levels of development and organizational maturity, led to the design of a model that, allowing for the assessment (quantification and qualification) of the performance of all FUs, promotes its continuous improvement and the reduction in the variability of achievable results, in a context of equity between different organizational typologies.
The operationalization of this purpose occurs through performance evaluation based on a multidimensional matrix that brings together an integrated view of the global performance of each FU typology.
For each area of the multidimensional matrix, different subareas, dimensions, metrics and indicators are defined, identifying the expected results. The indicators used in the contracting process are mandatorily included in the PHC Indicators Matrix and respect all its requirements and attributes and the rules of the Indicator Matrix are respected.
According to the 2018 Operation Guide and as far as possible and appropriate, indicators such as:
- Compounds or indices, in complex care processes that require multidimensional reading and monitoring (eg, indicators of access, efficiency, results, technical-scientific adequacy);
- From “Result” (eg, avoidable admissions, chronic patients with controlled pathologies, response times).
The IDG is obtained by the weighted sum of the Areas' Sectoral Performance Indices (IDS_A)[1], which in turn is obtained by the weighted sum of the Sectoral Performance Indices of the Sub-Areas (IDS_S)[2], which in turn is obtained by the weighted sum of the Sectoral Performance Indices of Dimensions (IDS_D)[3] (see Table 1).
The result of each IDG, IDS_A, IDS_S and IDS_D is a value between 0 and 100 (real continuous scale).
The weightings of IDS_A, IDS_S and IDS_D are subject to correction in the following situations:
- Omission of Performance Matrix components (eg existence of a matrix dimension without validated indicators or metrics; existence of a matrix sub-area in which all dimensions were not operationalized);
- FU that, for reasons (context or otherwise) not attributable to itself, cannot assume/do not need any dimension of activity in the multidimensional matrix, a situation in which the calculation of the IDG is obtained by correcting the weights of the remaining dimensions.
Table 1 - Calculation of IDG
Global IDG | Sector IDG |
dimensions | |
Area | Sub area | ||
IDG (100) |
Performance (100x0.5) |
Access (100x0.2) - Access Qualification | Coverage (1 000x0.1) |
| Customization (1 000x0.1) | |||
| Telephone answering (1 000x0.1) | |||
| TMRG (1000x0.4) | |||
| Consultation on the day (100x0.1) | |||
| Path (100x0.1) | |||
| Distribution on the day (100x0.1) | |||
| Child health (100x0.25) | |||
| Women's health (100x0.25) | |||
| Adult Health (100x0.25) | |||
| Elderly Health (100x0.25) | |||
Disease Management (100x0.2) - Career path/plan management, Outcomes in acute and chronic disease management | Management of people with diabetes (100x0.25) | ||
| Management of people with hypertension (100x0.25) | |||
| Management of people with respiratory distress (100x0.25) | |||
| Management of people with multimorbidity (100x0.25) | |||
| Prescription qualification (100x0.2) – Technical-scientific adequacy, Effectiveness, Efficiency. | Pharmacotherapeutic prescription (100x0.05) | ||
| Prescription of MCDTs (100x0.03 | |||
| Care Prescription (100x0.02) | |||
Satisfaction (100x0.2) | |||
IDG (100) |
services (100x0.1) | assistance (100x0.8) | Assistance services |
Non-assistance (100x0.2) | Clinical Governance Activity at ACES | ||
| Non-Assistential Activities in Regional Services or Ministry of Health Centers | |||
Organizational Quality (100x0.2) |
continuous improvement (100x0.4) | Hits (100x0.25) | |
| Integrated Assistance Processes (100x0.75) | |||
Safety (100x0.4) | users (100x0.4) | ||
| professionals (100x0.3) | |||
| Risk management (100x0.3) | |||
| Citizen Centrality (100x0.2) | |||
Training (100x0.1) |
internal (100x0.8) For FU professionals | multidisciplinary team (100x0.5) | |
| Interns/students (100x0.5) | |||
| external (100x0.2) | FU and/or its professionals as external trainers | ||
| Investigation work (100x0.5) | Articles, Communications, Conferences (100x0.5) | ||
| Investigation work (100x0.5) | |||
Source: Own elaboration based on doc. TTerms of Reference for Health Care Contracting in the NHS 2018.
All indicators of the PHC indicator matrix with results are available, regardless of whether or not they are used in the calculation of the 2018 IDG. The indicator result reading has the metric already mentioned (0.1,2)[1].
According to the document for the PHC contract for 2018 and after calculating the performance levels of each FHU, we can know which step it belongs to, as shown in the following table.
Table 2 - IDG Performance Levels
Step | Criterion |
THE | <50> |
B | ≤ 50 and < 75> |
C | ≥ 75 and < 85> |
D | ≥ 85 and < 95> |
AND | ≥ 95 |
Source: (ACSS, 2018) Terms of Reference for Contracting PHC 2018 - IDG calculation - UPHC and FHU
When you want to analyze the performance of an organization, as a rule, it is resorted to the determination of a set of performance indicators, commonly known as Key Performance Indicators (KPI). In the specific case of the FHU, the indicators used in contracting are grouped into four major areas: access, care performance, perceived quality and economic performance, as shown in the table.
In order to make the process more flexible and simpler, fifteen indicators are contracted, distributed on the following basis: four for access, eight for care performance, one for perceived quality and two for economic performance (Table 3).
Table 3. Indicators common to FHU
Area | Number [1] | Referrals |
Access | 3.12 | Percentage of consultations to the user by their own family doctor |
| 3.15 | Global Query Usage Rate | |
| 4.18 | Rate of medical home visits per 1000 subscribers | |
| 4.30 | Nursing home visit rate per 1000 registrants | |
Performance care | 5.2 | Percentage of women between 25 and 64 years old with up-to-date colpocytology |
| 5.4 M | Percentage of diabetics with at least 2 HbA1C[2] recorded in the last 12 months since they cover 2 semesters | |
| 5.10 M | Percentage of hypertensive patients with at least one BP assessment[3] in each semester | |
| 6.1 M | Percentage of children with PNV[4] updated at 2 years | |
| 6.1.M | Percentage of children with PNV[5] updated at 7 years | |
| 6. 12 | Percentage of first appointments in life made within 28 days | |
| 6.9 M | Percentage of first pregnancy consultations in the first trimester | |
Efficiency | 7.6 | Average cost of prescribed drug per user |
| 7.7 | Average cost of MCDT[6] prescribed by user |
Source: (ACSS, 2017).
According to what is established in Ordinance No. 212/2017, of July 19, and in the Operationalization Guide of the IDG PHC 2018, we can say that the evaluation process of each of the contracted indicators results in one of three possible qualitative classifications: “hit”, “almost hit”, “not hit”.
This classification corresponds to a scoring system of two, one and zero, respectively. The following table summarizes the FHU assessment metrics (Table 4).
Table 4. Evaluation Metrics of the indicators contracted by the FHU
Score |
Punctuation | Access Performance care Quality perceived |
Performance Economic |
Achieved (result within expected range) |
two | < 90> | < 100% |
Almost achieved (result within acceptable range) |
1 | [80-90%] | ]100 -105%] |
Not achieved (does not comply) |
0 | <80> | >105% |
Source: (ACSS, 2017) Terms of Reference for Health Care Contracting in the NHS for 2018
1.2. Balanced Scorecard (BSC)
The BSC helps organizations to overcome two fundamental issues: the effective assessment of organizational performance and strategy implementation (Kaplan & Norton, 1992), assuming itself as a performance management system aligned with the strategic implementation. The BSC was developed by Robert Kaplan and David Norton who, in 1990, led a study with a dozen companies, aiming to explore new methods of performance evaluation. In 1992, after a research project conducted with 12 large companies, they designed a set of measures that complemented the traditional financial measures, more focused on past events, with operational measures for future value creation, namely in the areas of customer satisfaction, internal processes, learning and growth, all in an integrated manner (Kaplan & Norton, 1992).
- Thus, in addition to seeking to attain good financial results, organisations are enabled to monitor progress in the acquisition of intangible assets required for growth, thus bridging the gap between long term strategy and short term actions (Kaplan & Norton, 1996). The objectives and measures that constitute the four BSC perspectives - financial, customers, internal processes and learning and growth - derive from the organisation's strategy and vision.
- At the beginning of the tool conception the BSC interest focused essentially on adding intangible values to the assessment, enabling a long-term vision (Kaplan & Norton, 1992).
- At a later stage the BSC was already seen as a management system directed towards improvement and planning (Kaplan & Norton, 1993), moving then from an evaluation system to a strategic management system with vision and strategy being placed at the Scorecard's centre (Kaplan & Norton, 1996).
- With the description of the cause-effect relationships between the objectives of each perspective a new instrument emerged, today with a crucial importance at the BSC implementation level - the Strategy Map. Strategy maps, which according to the authors themselves are at least as important as the BSC, are able to communicate both the organisation's strategy and the processes and systems that will help to implement it, through a visual representation of critical objectives and the crucial relationships between them. From a broader perspective, strategy maps show how the organisation will convert resources and initiatives into tangible results (Kaplan & Norton, 2004).
- Thus, the BSC has evolved into a system for communicating strategy and translating strategy into operational terms in stages (Pinto, 2007):
- Performance evaluation system;
- Strategic management system - Evolution 1;
- Strategy communication system - Evolution 2;
- Change management system.
- The BSC can be used as a performance measurement system, a strategic management system and a communication tool (Niven, 2006).
- In the case of public services, this perspective works more as a facilitator or as a constraint in the execution of the organisation's strategy, i.e., it translates into the objective of respecting the budget granted to the institution and using the available resources efficiently and effectively (Maia, 2011). Furthermore, it occupies a leading role, right after the mission, and emerging from it.
- As for the perspective of internal processes, it identifies which processes the organisation should excel in, which processes already exist, which may be subject to improvement actions or the creation of new processes. The measures focus on the processes that have the greatest impact on customer satisfaction and on the achievement of the organisation's financial objectives. In this way, and in public services, the indicators of this perspective are related to the options taken from the perspective of customers and stakeholders, also having a connection with the decrease in costs and maintenance of quality from the financial perspective (Maia, 2011).
- The set of cause-effect relationships between perspectives, goals, objectives and indicators is one of the essential principles in the BSC operation and that differentiates it from other performance assessment systems (Pinto, 2007). Its merit lies in the appropriate combination of these methods and processes, building a consistent and innovative conceptual proposal by combining these elements:
- The social perspective - Increase user satisfaction;
- Optimize health and disease prevention;
- Improve the quality and efficiency of the services provided;
- Improve communication.
If this is the case we can continue to create value for the health services provided to the community.
1.2.1. Application of the BSC in the Health Sector
Considering all performance management systems, the BSC is probably the one that can be used the most in the healthcare field. It has unique capabilities that can be extremely useful for the management of public health services.
According to Zelman, Pink and Matthias (2003) the design and development of performance management systems based on the BSC methodology in the health sector have the following benefits:
- Link performance appraisal to strategy;
- Align professionals with a more targeted strategy for users;
- Facilitate, monitor and evaluate the implementation of the strategy, providing continuous feedback on it, which promotes regular strategic adjustments;
- Facilitate the selection of initiatives and optimize the allocation of resources;
- Communicate the strategy to all levels of the organization;
- Encourage communication and collaboration among health professionals;
- Attributing accuracy and helping to convey relevant information to the public;
- Finding a common language for different professional groups and facilitating the relationship between management and these, as it is a simple and multidimensional tool.
Inamdar, Kaplan and Reynolds (2002) conclude that the BSC, as a tool for implementing a performance management system, can be successfully applied in the health sector, allowing organizations to improve user satisfaction, market positioning and financial results, as well as the call for attention to the importance of commitment on the part of administrators and top management, ensuring all the necessary resources and specific training for professionals.
When this commitment fails, the failure of the BSC application is more likely.
2. Research Methodology
2.1. Framework
The present work consists of an investigation that, regarding its method, can be classified as a descriptive observational investigation. According to Coutinho (2018), this area of investigation involves studying, understanding and explaining the current situation of the object of investigation. Within this type of investigation, the “case study” was used, which according to the same author, is a type of study that has been widely used in all sciences, especially in the social sciences. The case study is an empirical approach that investigates a current phenomenon in its real context, when the boundaries between certain phenomena and their context are not clearly evident, and in which many data sources are used.
2.2. Research instruments and data collection
In order to obtain the information necessary to carry out this study, the data collection technique adopted was document analysis. This research focused mainly on publications (articles and theses) already prepared about the BSC methodology, official documents - documents with the information already dealt with (such as commitment letters from the FHU Calâmbriga and FHU São João) and official websites with information already processed and available to the public.
3. Proposal For A Performance Management Model According To The Bsc Applied To Two Fhu Of Aces Edvii
This study aims to analyze how the BSC can be applied to two FHU of different models of the same ACES, FHU Calâmbriga and FHU São João. Based on this objective and the nature of the object to be investigated, a qualitative approach was adopted to develop the present investigation.
In this sense, in the following points we proceed with the application of the BSC philosophy as presented above, that is, following the guideline of Kaplan and Norton (2000)and theoretically applying the same model to both FHU.
- Mission, values and vision
The Mission of the two FUS is: Ensure the provision of PHC to the population of a given geographic area.
Values are: Develop activities to promote health and disease prevention, provide care in the disease as well as the connection to others, services for the continuity of care; Develop activities of epidemiological surveillance, health research, control and evaluation of results and participate in the training of different professional groups in their different stages, undergraduate, graduate and continuous.
The vision is: it concerns the legislative part that they are obliged to comply with.
- Objectives, indicators, goals of the FHU Strategic Plan
Taking into account the situation diagnosis of ACESEDVII-II, prepared by the local health observatory, the priority areas of intervention of the FHU Calâmbriga and FHU São João are as follows:
- Cardio-cerebrovascular diseases;
- Oncological diseases;
- Diabetes Mellitus;
- Mental health disorders;
- HIV infection AIDS;
- Tobacco consumption;
- Overweight / obesity / promotion of healthy eating;
- Teenage pregnancy.
In addition to the aforementioned areas, and considering the problems and national priorities, the two FHU also include the following areas:
- Respiratory diseases;
- Alcohol-attributable illnesses;
- Accidents
In the case under study, the FHU Calâmbriga and FHU São João:
- The objective will be to maximize user satisfaction;
- The goal will seek greater effectiveness and efficiency in serving users;
- The indicator par excellence will be that of user satisfaction;
- The initiatives to be put into practice include: pprovision of primary health care oriented towards the citizen and the surrounding community in the municipalities of S. João da Madeira and Vale de Cambra, based on the principles of proximity, accessibility, equity and quality, thus contributing to their satisfaction.
- The users' perspective
For the FHU Coordinators under study, users are the main stakeholders in the proper functioning of the FHU.
Thus, the objectives according to this perspective are:
- Increase user satisfaction;
- Improve the performance of employees (doctors, nurses and assistants).
To assess these objectives, indicators can be based on:
- Waiting period for appointments and respective care by the family doctor or nurse;
- % of satisfied and very satisfied users;
- Number of complaints;
- waiting lists for nursing care;
- Mortality and Morbidity Indices;
- # of acute episodes with episode encoding (ICPC2[1])/total number of episodes;
- % of hypertensive patients with blood pressure recorded in each semester;
- % of term newborns with low birth weight;
- Incidence of amputations in diabetics in the resident population/10 000 inhabitant;
- Incidence of cerebrovascular accidents in the resident population/10 000 Inhabitant;
- Consumption of anxiolytics, hypnotics, sedatives and antidepressants on the NHS market, in an outpatient clinic (Defined Daily Dose/1000 inhabitants/day);
- Number of incidents and clinical malpractices reported;
- Number of clinical acts scheduled and not performed;
- Average enrollment per physician;
- Average of assisted by a health professional;
- Average of medical consultations per assisted.
- the financial perspective
Thus, the objective, according to this perspective, is to improve the management of each FHU under study. In this phase, financial performance indicators are defined that allow measuring the fulfillment of the level of achievement of the financial objectives – result indicators. According to the FHU Contracting Indicators and Targets, examples are:
- Cost of medications per patient;
- Operating result per patient;
- Value of medical prescriptions per patient;
- % of generic drugs in packaging/total drug packaging;
- Average cost of drugs billed per user;
- Average cost of MCDT's billed per user;
- Average cost per medical appointment;
- Personnel cost fee.
- The perspective of internal processes
The value proposition helps to generate successful action indicators with the target audience, which will then be complemented with more traditional measures of results (outcome indicators), such as the level of satisfaction of the target audience. To achieve the users' goals and, finally, the financial goals, it is necessary to develop performance measures to control the main internal processes and activities that support the target audience's value proposition. According to the Contracting Indicators and Targets of ACES EDVII-II and in turn of the FHU Calâmbriga and FHU São João, examples are:
- Global usage fee for medical appointments;
- Fee for using Family Planning (FP) consultations;
- % of first appointments in life performed within 28 days;
- % of users with the National Vaccination Program (PNV) updated at 14 years of age;
- % of enrollees aged 50-74 with colorectal cancer screening performed;
- Coverage rate in organized cervical cancer screening (25-64 years) in eligible population;
- Coverage rate in organized breast cancer screening (45-69 years) in the resident population;
- Rate of medical home visits per 1,000 subscribers;
- % of users with updated PNV at 7 years old;
- Degree of achievement of contracted objectives;
- The learning and growth perspective
The learning perspective can be related to the need to have employees with competence in the health area, so that human resources can contribute to the optimized management of the FHU.
Learning and Growth indicators are really the "enablers" of the other perspectives. Motivated professionals with the right skills and tool requirements, operating in an organizational climate designed to sustain improvements, are key ingredients in driving process improvements, meeting customer expectations, and ultimately enabling financial returns. In measuring skills (Drucker, 2012)suggests that any organization can be as successful as any other. The only distinction is how you develop your own employees. Niven (2006) presents the following suggestions for measuring human resource development:
- Use core competencies to measure your development - identify the differentiating competencies needed to achieve strategic goals;
- Carry out a personal development plan to increase skills holders;
- Encourage healthy lifestyles;
- Measure the level of training of employees;
- Measure the level of employee satisfaction.
- the social perspective
Once the Health Area manages the needs of users, it will be necessary to consider the possibility of considering a social perspective, since FHU is expected to defend and protect the health of all citizens. This perspective is based on the idea that, ultimately, the user does not expect to ever miss any visit made to his or her family doctor or nurse or to return home worse, he can expect the maintenance of his poor health, so he resorts to his FHU.
Thus, the objective according to this perspective will be to increase/maintain the user's well-being.
For the FHU Board (case under study), we consider a fifth perspective, the social one, in the treatment of the BSC, as we are aware that it is important for the success of the defined strategy, that is, to be relevant, in the sense of the need for protection of the interests of users and others interested in health care.
In this perspective, it is intended to define a set of indicators that allow measuring the social attributes of the FHU Calâmbriga and FHU São João. According to the Indicators and Targets, examples are:
- Presence of a Social Worker to accompany users in cases of socioeconomic need or need;
- % of satisfied and very satisfied users;
- Number of complaints;
- Consumption of anxiolytics, hypnotics, sedatives and antidepressants on the NHS market, seek to know the cause for taking these medications;
- Number of incidents and clinical malpractices reported;
- Number of clinical acts scheduled and not performed.
- cause-effect relationships
The relationships between the various perspectives, objectives, indicators and targets are the
which are presented in the Strategic Map presented below.
The BSC philosophy allows us to verify the linear relationships in the identification of the four present perspectives: financial, customers, internal processes and learning, objectives, targets and indicators” (Pinto, 2007, p. 46). It is this same feature that distinguishes the balanced scorecard from any other performance appraisal system. Figure 1 shows an application of this relationship and can be applied to any FHU, or other public or private entity as mentioned above.
The cause and effect/linearity process will help to identify the infrastructure and skills that each FHU needs to develop in order to support internal processes and thus satisfy users. A well-constructed BSC should describe the strategy in the most appropriately chosen objectives and indicators. The indicators should be linked by cause-effect relationships, from the perspective of learning and growth (the cause) to the financial perspective (the effect), thus identifying the influence on the final result.
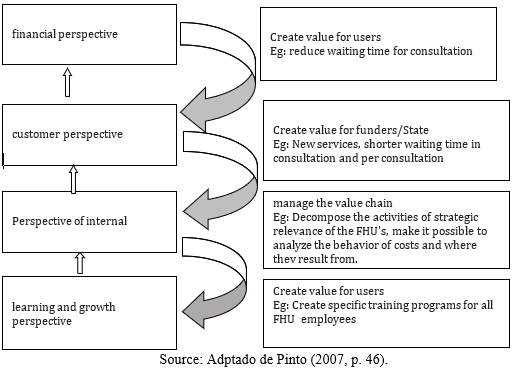
Creating the cause-effect link between performance and indicators is one of the most complex aspects of implementing a BSC, but by overcoming this difficulty, it means that we will obtain a system that articulates the strategy, allows communication to all stakeholders and promotes a constant articulation of the strategy with the environment of the organization.
In practice, cause-effect relationships allow testing the model, that is, they assess whether the BSC is effectively reflecting the organization's strategy.
Thus, the objectives that appear in the base of the BSC, induce higher level objectives, and these, in turn, must allow reaching the final objective – the vision of each FHU.
This cause-effect relationship has been present in the model from the beginning.
Strategic Map
On the strategy map, the objectives of each of the FHU are positioned, arranged in a matrix ordered horizontally, by the five perspectives and, vertically, by the main strategic guidelines. It is a powerful instrument for visualizing objectives and the cause and effect relationships between them. In a reform of this importance and complexity, a strong strategic framework is essential, making it possible to avoid unnecessary delays in critical reform initiatives through more detailed and timely programming. Next, we present the consolidated strategy map for each FHU, where all the perspectives and objectives, within each one of them, are interconnected with the strategy and with the organizational mission.
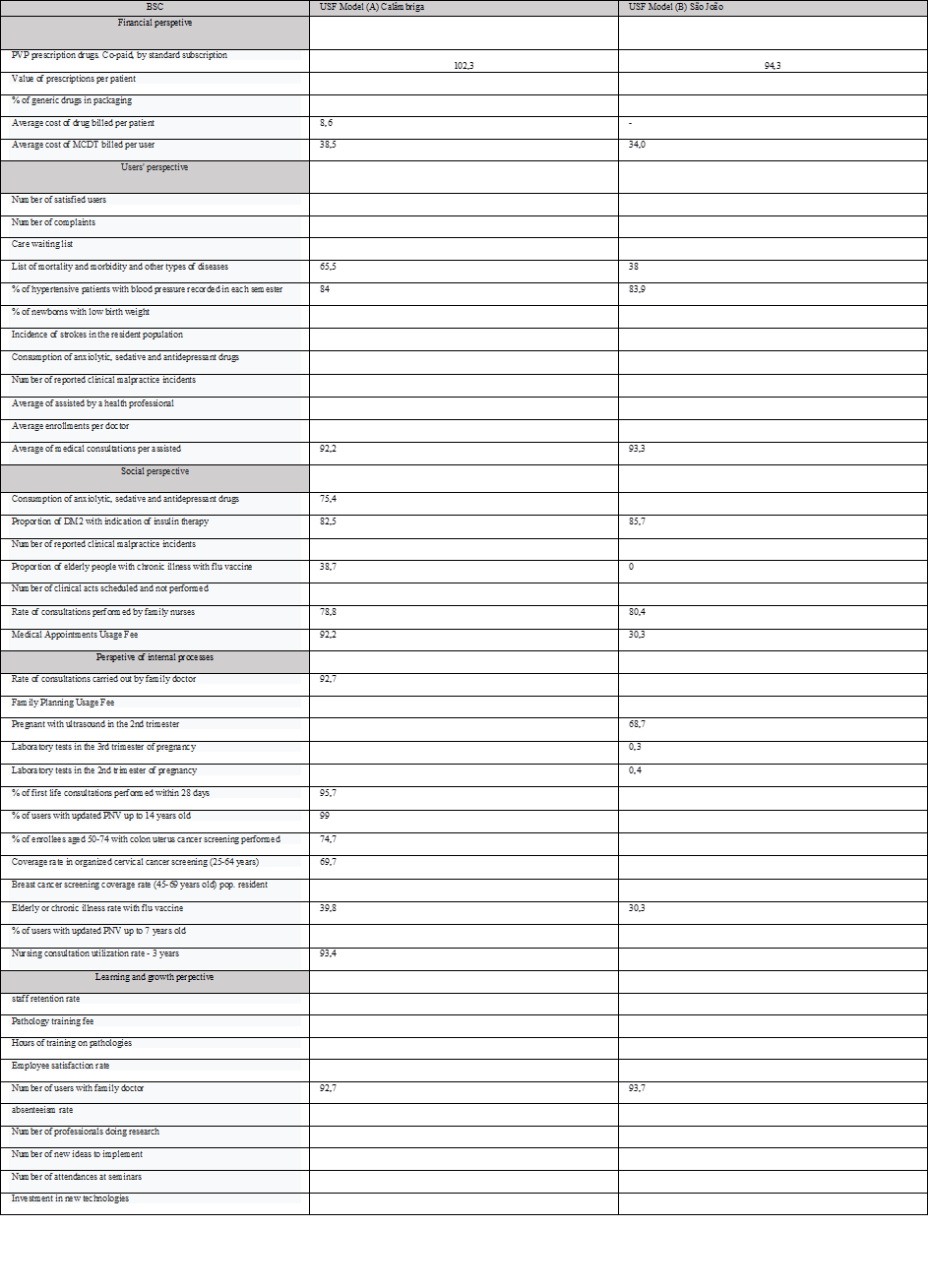
It should be noted here that we were unable to fill in all the indicators, as they are not available for public consultation and the authorization request does not include this part, we leave behind the structure and how they can be applied computerically, or even in the program " excel”.
In these cases, the differences are few, as the FHU Calâmbriga seems to have the conditions to move this year to Model B, so the values of the indicators in Table 5 are similar.
In Figure 3 we systematize in a simple way all the perspectives and some of the objectives that can be implemented.
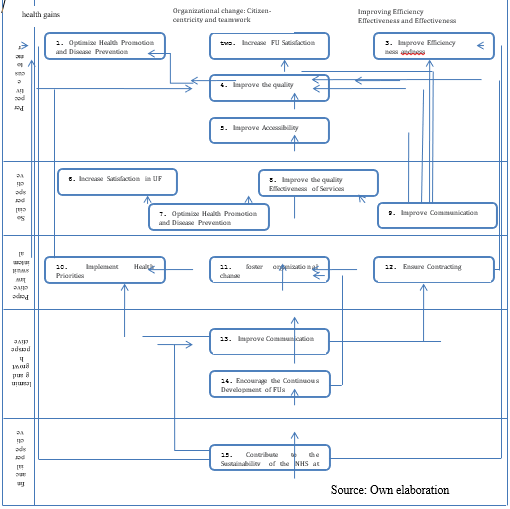
Source: Own elaboration based on the DGS website (2020) and biPHC.min-health.pt
In table 5, we present the “five” perspectives of the BSC applied to the two FHU, with the data that we were able to collect in each of them. We grouped the five indicators according to the perspective of the BSC and the way in which we consider that the indicator best responded to the perspective in question.
Observing the data in the following table, we continue to observe two FHU with different models, but with very similar values.
We can even say that the FHU model A has, in one of the headings in different perspectives, percentage values that are much higher.
As in the case of the Users' Perspective – Morbidity and other types of diseases rate at FHU Calambrica 65.5% and at FHU São João 38.0%.
The rate of use of medical appointments is much lower at the FHU São João, probably related to what we mentioned above, this FHU is located in an urban area with a lot of private health services, causing the population to naturally resort more to these services.
Conclusion
This study focused on two FHUs of the EDVII-AN PC that operate in Primary Health Care (PHC) through a network of PHCs. It is a case study of a markedly theoretical nature, in which the description of a set of elements in the management field was deepened, from the operational to the strategic level.
The general objective of this work was to develop a BSC, as a Strategic Performance Management Instrument, adapted to the Health Service under study, which, if implemented, provides effective management of organisational performance, with an efficient and effective use of resources, in a balanced and strategically aligned way.
In an economic and social context of constant change, it is more than justifiable that organisations seek means to obtain greater control of their performance so that they can, in useful time, put corrective measures in place, should performance not be as desired.
We proposed to study the BSC implementation process in an area such as health. Therefore, we considered it relevant to understand to what extent the implementation of the BSC could contribute to improve its performance, identifying the particularities of the health activity in comparison with most of the other economic activities, and its main attributions, from which we highlight the management of patients and average attendance times for each of them.
Addressing the BSC theoretical model, and the constant evolution it has undergone since 1992, we conclude that it continues to be a performance assessment model to be considered, both for its design and the final information it provides, as it allows for easy reading by users and, therefore, also by FHUs.
In addition to the four traditional perspectives of the application of this instrument, we justify the sense of considering a fifth perspective, the social one, to an area involving the management of human capital originating from users and health professionals.
The practical application, based on the Strategic Map presented, allowed us to expose in a practical way (one of the BSC objectives, simplicity) the existing relations between the strategies, the strategic objectives, passing through the identification of critical factors, the indicators to be considered for each of the defined objectives and the goal to be achieved. The Map would not be complete if there was no indication of an action programme, that is, what the Health area proposes to do to implement the method, either for subsequent follow-up.
As with any performance assessment method, it is not enough to master the technical aspect, it is necessary, we would even say fundamental, that there is political will and commitment from the ARS and the respective ACES regarding the implementation of the BSC project, since it involves and needs the collaboration of several segments of the FHU. Thus, the Administration must be aware that in a scenario of constant modernisation and competition, a new process that enables complementary and more sophisticated evaluations, in this case the BSC, is very important, so that existing resources may be optimised, with a view to obtaining both greater efficiency and greater effectiveness.
Comparing the indicators common to both FHU models - model A and model B - in the FHUs under study allows us to consider that they are practically similar and that there is linearity in the identification of the four BSC perspectives: financial, customers, internal processes and learning.
References
- ACSS (2017) ‘Termos de Referência para Contratualização de Cuidados de Saúde no SNS para 2018’, Acss, pp. 1–96. Available at: http://www.acss.min-saude.pt/wp-content/uploads/2018/12/Termos-Referencia-Contratualizacao-2019.pdf.
- ACSS (2020) ‘Termos de Referência para Contratualização de Cuidados de Saúde no SNS para 2021’.
- Ahrens, R. de B. (2017) A gestão estratégica na administração. Atena Editora.
- Biscaia, A. R. and Heleno, L. C. V. (2017) ‘A reforma dos cuidados de saúde primários em Portugal: Portuguesa, moderna e inovadora’, Ciencia e Saude Coletiva, 22(3), pp. 701–711. doi: 10.1590/1413-81232017223.33152016.
- Branco, A. G. and Ramos, V. (2001) ‘Cuidados de saúde primários em Portugal’, Revista Portuguesa de Saúde Pública, 2, pp. 5–11. Available at: http://scholar.google.com/scholar?hl=en&btnG=Search&q=intitle:Cuidados+de+saude+primarios+em+Portugal#0.
- Coutinho, C. P. (2018) Metodologia de Investigação em Ciências Sociais e Humanas - Teoria e Prática. Almedina.
- Drucker, P. (2012) The Practice of Management. Routledge. doi: 10.4324/9780080942360.
- Ferreira, M. A. F. (2010) Princípios estruturantes de um Balanced Scorecard Estratégico para Sistemas Integrados de Saúde. Universidade do Porto.
- Gonçalves, I. et al. (2006) Cuidados de Saúde Primário em Portugal Reformar para novos sucessos. 2a. Padrões Culturais.
- Inamdar, N., Kaplan, R. and Reynolds, K. (2002) ‘Applying the Balanced Scorecard in Healthcare Provider Organizations.’, Journal of Healthcare Management, 47(3), pp. 179–195.
- Kaplan, R.S. and Norton, D. P. (2004) Strategy Maps: Converting Intangible Assets Into Tangible Outcomes. Harvard Business Press, Boston, MA.
- Kaplan, R. S. and Norton, D. P. (1992) ‘The balanced scorecard: Measures That drive performance’, Harvard Business Review, 83(7–8).
- Kaplan, R. S. and Norton, D. P. (1993) ‘Putting the Balanced Scorecard to Work’, in The Economic Impact of Knowledge. Elsevier, pp. 315–324. doi: 10.1016/B978-0-7506-7009-8.50023-9.
- Kaplan, R. S. and Norton, D. P. (1996) ‘The Balanced Scorecard: Translating Strategy into Action’, Harvard Business Publishing, 30(June).
- Kaplan, R. S. and Norton, D. P. (2000) The Strategy-Focused Organization. Harvard Business School Press.
- Maia, L. A. A. (2011) Balanced Scorecard : Uma Ferramenta de Gestão no Sector Público Hospitalar.
- https://estudogeral.sib.uc.pt/handle/10316/31106
- Niven, P. R. (2006) Balanced Scorecard Step-by-Step: Maximizing Performance and Maintaining Results. 2nd edn. Edited by I. John Wiley & Sons.
- Pinto, F. (2007) Balanced Scorecard Alinhar Mudança, Estratégia e Performance nos Serviços Públicos. Edições Sílabo.
- Zelman, W. N., Pink, G. H. and Matthias, C. B. (2003) ‘Use of the Balanced Scorecard in Health Care’, Journal Health Care Finance, 29(4), pp. 1–16.


