Archive : Article / Volume 1, Issue 1
- Research Article | DOI:
- https://doi.org/10.58489/3066-0955/003
Asthma in India
Public Health Consultant Bengaluru and Professor of Practice, School of Environment Sciences, Public Health, and Sanitation Management, Karnataka State Rural Development and Panchayat Raj University (KSRDPRU), GADAG, Karnataka, India
Suresh Kishanrao
Suresh Kishanrao, (2023). Asthma in India. International Journal of Pulmonology and Disorders.1(1). DOI: 10.58489/3066-0955/003
© 2023 Suresh Kishanrao, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 16-01-2023
- Accepted Date: 28-01-2023
- Published Date: 31-01-2023
GBD, Asthma, COPD, GERD, Rhinosinusitis, Obstructive Sleep Apnoea, Bronchodilators, Asthma Control inhalers, Corticosteroids, Anti-IgE
Abstract
India's burden of non-communicable diseases (NCDs) is escalating. NCDs typically present in individuals aged 55 years or older in many developed countries, but their onset occurs in India a decade earlier ≥45 years of age. The India GBD Collaborators showed that COPD, and asthma made the second largest contribution to the total mortality burden of India, at 10·9%. The crude prevalence rates of Asthma 8·6% (6·1–11·4) in 1990-2016 period.
Asthma is a major and common chronic noncommunicable disease (NCD), affecting both children and adults. Asthma affected an estimated 280 million people in 2022 and caused half a million deaths globally. India contributes to 12.9 % of Global Asthma cases and 42.4% of global Asthma Deaths. The prevalence of Asthma in USA and UK is much higher, so is the treatment adherence, mainly due to better diagnostic facilities and their use.
The diagnosis of Asthma in Low- and middle-income countries (LMICs) is mostly by clinical examination that include, Physical examination -use of stethoscope to hear typical wheeze, Lung function Tests including peak flow meter and spirometers and Chest Xray chest to rule out Pneumonia, TB and Lung Cancer, X-Ray sinuses to rule out Rhinosinusitis. The management principles include 1) use of inhalers (powder or metered dose) for easing breathing like Salbutamol, Lev Salbutamol and Terbutaline 2) Controller medication Inhalers containing Beclomethasone, Budesonide, Fluticasone and Mometasone. 3) Combination of both medications 4) Short courses of Corticosteroids during asthmatic attacks. 5) Anti-IgE (omalizumab for patients with severe asthma.
To comply with WHO Global Action Plan for the Prevention and Control of NCDs and the United Nations 2030 Agenda for Sustainable Development, member countries have committed to improving the diagnosis, treatment, and monitoring of asthma to reduce the global burden of NCDs, to progress towards universal health coverage 2030.
This article reviews the situation of Asthma management in India in general and three case reports to describe the challenges of under- diagnosis and sustained treatment.
Materials and Methods: Review of national and global guidelines for accessibility and utilization of Asthma management, three case reports illustrating challenges
Introduction
India's burden of non-communicable diseases (NCDs) is escalating. NCDs typically present in individuals aged 55 years or older in many developed countries, but their onset occurs in India a decade earlier ≥45 years of age. The India GBD Collaborators showed that COPD, and asthma made the second largest contribution to the total mortality burden of India, at 10·9%. The crude prevalence rates of Asthma 8·6% (6·1–11·4) in 1990-2016 period [1].
Asthma is a major and common chronic noncommunicable disease (NCD), affecting both children and adults. Inflammation and narrowing of the small airways in the lungs cause asthma symptoms, which can be any combination of cough, wheeze, shortness of breath and chest tightness. The symptoms are often worse at night or on waking from sleep. Usually, they resolve spontaneously or with the inhalation of a reliever medication. Exact cause of Asthma is not yet understood but there are multiple risk factors. Inhaled medicines can control symptoms and allow people to lead a normal, active life. Avoiding allergic triggers also help to reduce asthma symptoms [2]. Gastroesophageal disease (GORD), Rhinosinusitis and Obstructive Sleep Apnoea are associated medical conditions [2,11,12,13].
Asthma affected an estimated 262 million people in 2019 and caused 455000 deaths globally, most asthma-related deaths occur in low- and lower-middle-income countries, due to under-diagnosis and under-treatment [2]. It is included in the WHO Global Action Plan for the Prevention and Control of NCDs and the United Nations 2030 Agenda for Sustainable Development. WHO member countries have committed to improving the diagnosis, treatment, and monitoring of asthma to reduce the global burden of NCDs, to progress towards universal health coverage 2030. [2]
India contributes to 12.9 % of Global Asthma cases and 42.4% of global Asthma Deaths [2] In the national NCD program the diagnostic tools recommended are i) Physical examination -use of stethoscope to hear typical wheeze, ii) Chest Xray chest to rule out Pneumonia, TB and Lung Cancer, X-Ray sinuses to rule out Rhinosinusitis 3) Lung function Test including peak flow meter. The management principles include 1) use of inhalers (powder or metered dose) for easing breathing usually contain Salbutamol, Lev Salbutamol and Terbutaline 2) Controller medication Inhalers containing Beclomethasone, Budesonide, Fluticasone and Mometasone. 3) Combination of Bronchodilators and Preventive medications are also used.4) Short courses of Corticosteroids during asthmatic attacks. 5) Anti-IgE (omalizumab) is an approved treatment for patients with severe asthma that acts on decreasing serum IgE levels, as documented in effectively treating asthma. The program recommends danger signs as i) Asthma attacks not responding to inhalers, difficulty in talking due to breathing problem, peak flow meter readings <50>
According to recent international guidelines, patients with uncontrolled asthma require a prolonged maintenance treatment with high-dose of inhaled corticosteroids (ICS) in association with a long-acting β2-agonist (LABA) plus oral leukotriene receptor antagonist (LTRA). The management of asthma is evolving as more patient-specific, due to better understanding of biology of the development and progression of asthma. The addition of omalizumab, the first targeted biological treatment for asthma, has led to renewed optimism in the management of children and adolescents with atopic severe asthma [8].
The prevalence of Asthma in developed countries like USA and UK is much higher, so is the treatment adherence, mainly due to better diagnostic facilities and their use. While overall 25 million people (7.8% of the population) suffers with Asthma in USA in 2020 [3] in UK 5.4 million people (8%) [4]. The total burden of asthma in India is estimated to be 34.3 million, accounting for 12.9 % of the global burden as of 20 June 2022.
It was previously estimated that the prevalence of asthma in India was about 3%), with a prevalence of 2.4% in adults aged >15 years, and between 4% and 20% in children. Overall prevalence in men was 5.9% and among women 8%. The urban prevalence was around 4.4% among men and women, whereas it was higher at 6.5% among rural men [7] Childhood asthma is a leading cause of emergency department visits, hospitalizations and missed school days. Unfortunately, it can't be cured, and symptoms mostly continue lifelong.
Current study showed a significant reduction in the prevalence of current wheeze (p<0>
The estimated prevalence of self-reported asthma in adult Indians based on analysis of 99 574 women and 56 742 men aged 20–49 years included in India’s third National Family Health Survey, 2005–2006 was 1.8% (95%CI 1.6–2.0) among men and 1.9% (95%CI 1.8–2.0) among women, higher rates in rural than in urban areas and marked geographic differences. After adjustment for known asthma risk factors, women were 1.2 times more likely to have asthma than men. Daily/weekly consumption of milk/milk products, green leafy vegetables and fruits were associated with a lower asthma risk, whereas consumption of chicken/meat, a lower body mass index (BMI; <16>30 kg/m2, OR 1.67, 95%CI 1.36–2.06), current tobacco smoking (OR 1.30, 95%CI 1.12–1.50) and ever use of alcohol (OR 1.21, 95%CI 1.05–1.39) were associated with an increased asthma risk [6].
Data from Indian centres that participated in the multicentre current Global Asthma Network showed a significant decline in symptoms of asthma compared to 2005 and 2013 studies. Most distressing inference was almost 82% of current wheezers and 70% of subjects with symptoms of severe asthma were not clinically diagnosed as having asthma. The daily use of inhaled corticosteroids (ICS) was less than 2.5% in subjects with current wheeze and those with symptoms of severe asthma but less than 1% used daily ICS when asthma remained undiagnosed [6].
Approximately 25 million people in the U.S. have asthma. This equals about 1 in 13 people. About 20 million U.S. adults aged 18 and older have asthma. Asthma is more common in female adults (9.8%) than male (6.1%) adults. It is a leading chronic disease in children.2 Currently, there are about 5.1 million children under the age of 18 with asthma. Asthma is more common in male (8.4%) children than female children (5.5%). In 2019, 44.3% of children aged 18 and younger who had asthma reported having one or more asthma attacks in the past year. About 47.2% of children under the age of 5 with asthma had an attack. According to the Centres for Disease Control and Prevention (CDC), asthma attacks in children have declined from 2001 through 2019.3 Even though asthma is controllable, it is estimated that 50% of children with asthma have uncontrolled asthma [2]. The data are from national and state surveillance systems administered by the Centres for Disease Control and Prevention (CDC) indicates a prevalence of Asthma to be 8% of adults over 18 years and 7% for children under 18 years in USA. The highest prevalence was among 20–24-year-olds and lowest prevalence of 2.6% among 0–4-year-old children. After age of 5years it remained between 7-10% of each age cohort and the elderly population (>65yrs) had a prevalence rate of 7.7%. Overall female had higher prevalence of 8.9% when compared to Men 6.6%. The gender difference was more pronounced among Boys (8.8%) under 18 years compared to girl under 18 years (5.5%). Among the adults the trend was reversed as women had 9.8% and men 6.6% [5]. National Prevalence of Asthma Attacks among People with Current Asthma by Age (2020) indicates Total surveyed -10,342,170 Asthmatics 41%. Children (<18>
A leading lung charity warned in September 2022 that there are 5.4 million out of estimated 67.5 million (8%) people in the UK with asthma [4]
Case Reports
1.Carcinoid Tumour confusing Br. Asthma: Uncontrolled symptoms that lingered despite aggressive Asthma, therapy warranted evaluation resulting in carcinoid tumour in the left Bronchus, and left lower lobectomy helped in relieving the Asthma to a status of medical management.
Way back during my internship in 1983 A 48-year-old, a village woman, a housewife, was admitted to our Medical College hospital complaining of wheezing and dyspnoea in the midnight. Suspecting status asthmaticus we got the physician examine her and put her on IV corticosteroids for detailed investigation next day. She had been diagnosed with asthma 12 years previously and was well controlled using budesonide at 160 μg + formoterol at 4.5 μg b.i.d. combination therapy until 5 months before her visit to our hospital. She had had a severe asthma attack at that time, during which her wheezing was not well correlated with physical exercise and had persisted for several months. She was treated unsuccessfully with budesonide at 320 μg + formoterol at 9 μg b.i.d. combination, montelukast at 10 mg/day, and oral steroids (30–40 mg/day of prednisolone) during that period, and because her asthma had failed to come back under control, was referred to our hospital and hospitalized for evaluation for anti-IgE therapy.
On examination her vitals were stable with a heart rate of 76 bpm, a temperature of 36.5°C, blood pressure of 110/70 mmHg, and respiratory rate of 28/min on physical examination. Her examination was normal except for decreased auscultation in the left lung. Next day her routine blood count was haematocrit, 40%; leukocyte, 10300; and erythrocyte sedimentation rate 15, mm/hr. Spirometry showed an obstructive pattern (forced expiratory volume in 1 second [FEV1], 2.20 L [82%]; forced vital capacity [FVC], 3.45 L [110%]; FEV1/FVC, 60%). We were unable to show spirometry reversibility. Her skin-prick test was positive for house-dust mites. Total IgE level was 115 kU/L. All data about the patient seemed to indicate that she could be a candidate for anti-IgE therapy.
The routine Chest radiography revealed a left-sided hilar opacity. A CT scan showed a 10-mm nodular lesion located in the left lower lobe bronchus. These radiological findings changed our management plan and diagnosis from asthma to a chest mass. A fibreoptic bronchoscopy was performed, which revealed an endobronchial lesion obstructing the left lower bronchus lumen. Biopsy was not performed for the fear of a risk of bleeding. The cytological examination of Bronchial lavage fluid removed from the left bronchus, was normal.
The patient was transferred to the thoracic surgery ward for surgical treatment. She underwent left lower lobectomy and mediastinal lymph node dissection. Histopathological examination revealed an intrabronchial tumour, made up of monotonous cells finely granular nuclei and eosinophilic cytoplasm. No mitotic figures or necrosis was detected. After surgical resection, she was asymptomatic with budesonide at 160 μg + formoterol at 4.5 μg combination therapy and had a better pulmonary function (FEV1, 2.53 L [95%], FVC, 4.29 L [138%]; FEV1/FVC, 59%).
2. Master Krishna – 8 yrs. male. 17/10/2022, brought to emergency admission with C/O cough, difficulty in breathing and tightness in chest. He was diagnosed as Asthmatic 2 years ago, and in the last 6 days the shortness of breath increased to compelled parents to get him to the emergency care.

Family history did indicate either the parents or 4 years older sister suffering from Asthma. On physical examination he was average built boy, with about 25 Kg weight, 120 Cm height, Pulse-100/min, RR- 30/min, BP-90/60. Total IgE was 480, KU/Litre as against a normal range of 400, ESR was elevated at 25/hr against upper limit of 20, and Chest Xray was normal. He was put on I V drip and though which antibacterial Ceftriaxone 1G was pushed twice /day Syrup Erythromycin was 200 mg was given twice orally, along with Budecort and Asthalin inhalers 2 puffs each at a time twice a day were given> Sodium chloride nasal drops 2 ml each for clearing the nose was also given 4th hourly.
A study nearly seven years ago, the Respiratory Foundation of India through the chest disease screening camps organised by Rotary International had reported an incidence of 5 to 7% in the urban population. However, in the last five to six years, this has doubled to 10 to 15% in the city of Chennai [8]. When children travel to school in the morning, they must go through the traffic on the road and are exposed to dense smoke and pollution. Mushrooming of flats system is contributing to increased pollution. Other factors such as dust, mites, and seasonal viral infections that are contributing for the increase in cities like Mumbai, Delhi, Bengaluru, Chennai, Kolkata etc. The use of steroid inhalers for asthma had gone up, indicating better acceptance levels among the people. What is disheartening is that patients do not take inhalers regularly, thinking that inhalers unsafe, may become addiction-prone treatment and causes growth stunting in children. Currently, the compliance level of steroid inhalers is around 15 to 20% only [8]
Case 3 ALLERGY BULLYING leading to Asthma:
A 10-year-old girl with a history of asthma presented to the emergency department with a three-day history of increased work of breathing, cough, and wheezing since early morning on 8 December 2023, a chilly day. She reported no clear trigger for her respiratory symptoms, although she had noted some symptoms of a mild upper respiratory tract infection. With this episode, the patient had been using a short-acting bronchodilator more frequently than she had in the past, without the expected resolution of symptoms.
On the day of presentation, the patient awoke feeling ‘suffocated’ and her mother noted her lips to be blue. In the emergency department, her oxygen saturation was 85% and her respiratory rate was 40 breaths/min. She had significantly increased work of breathing and poor air entry bilaterally to both lung bases, with wheezing in the upper lung zones. She was treated with salbutamol/ipratropium, intravenous steroids & magnesium sulphate. Her chest x-ray showed hyperinflation and no focal findings. The patient's asthma exacerbation resolved with conventional asthma treatment. Her pulmonary function tests were non concerning (FEV 1 - 94% and 99% of predicted) after her recovery.
Her medical history revealed that she was followed by a respirologist for her asthma, had good medication adherence and had not experienced a significant exacerbation for six months. She also had a history of wheezing, dyspnoea and pruritis with exposure to peanuts, chickpeas, and lentils, for which epinephrine injection. In the past, her wheezing episodes had been seasonal and related to exposure to grass and pollens. After a long counselling the patient later revealed that she had been experiencing significant bullying at school, as her classmates had smeared peanut butter on one of her cheeks. She developed pruritis immediately started wheezing and coughing later that day. This event followed several months of being taunted with peanut products at school. The patient was experiencing low mood and reported new symptoms of anxiety related to school.
The trigger for her asthma exacerbation was likely multifactorial, related to exposure to the food allergen as well as the upper respiratory infection. Population-based studies have shown that 20% to 35% of children with allergies experience bullying. In many cases this bullying is related directly to the food allergy [9].
Discussions
Patho-physiology-What Happens in an attack:
i) Bronchospasm: The muscles around the airways constrict making airways narrow and air cannot flow freely through constricted airways. ii) Inflammation: The lining of the airways becomes swollen, don’t let as much air in or out of your lungs. iii) Mucus production: During the attack, our body creates more mucus, which clogs airways.
Types of Asthma:
Asthma is classified into types based on the cause and the severity of symptoms [ 6].
For management purposes the Healthcare providers identify asthma as:
- Intermittent: This comes and goes; patient feels normal in between asthma flares.
- Persistent: In such cases symptoms mild, moderate, or severe persist much of the time. How well the patient does during an attack is also considered.
Academic classification based on the causes and onset include:
- Allergic: Some people’s allergies can cause an asthma attack. Allergens include moulds, pollens, and pet dander.
- Non-allergic: Outside factors like Exercise, stress, illness, and weather may cause a flare.
Based on onset time Asthma can be:
- Adult-onset: This type of asthma starts after the age of 18.
- Paediatric: Childhood asthma, begins before the age of 5, and can occur in infants and toddlers. Children may outgrow asthma. Doctors should decide whether a child needs to have an inhaler available in case of an asthma attack.
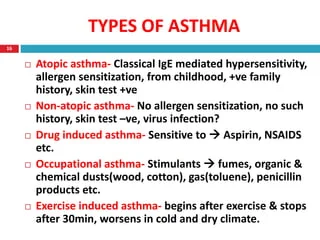
Other types of asthma include:
- Exercise-induced asthma: triggered by exercise induced bronchospasm.
- Occupational asthma: This asthma happens primarily to people who work around irritating substances.
- Asthma-COPD overlap syndrome (ACOS): This type happens when you have both asthma and chronic obstructive pulmonary disease (COPD). Both diseases make it difficult to breathe.
- Cough Variant asthma: The only symptom is persistent cough
Diagnosis of Asthma:
Asthma is a clinical diagnosis, based on a history of characteristic symptom patterns and evidence of variable expiratory airflow limitation. In well-resourced healthcare settings, this evidence is derived from spirometry with bronchodilator responsiveness- “reversibility” testing or bronchial provocation challenge testing. The differential diagnosis of asthma includes endemic respiratory disease like tuberculosis, HIV/AIDS and parasitic or fungal lung diseases. clinicians place greater reliance on clinical findings and often use syndromic approaches to diagnosis and management. In LMICs, like India even when available, these investigations are still substantially underused (unaffordable or time-consuming in special clinics), and more than one test is often required to confirm airflow variability.
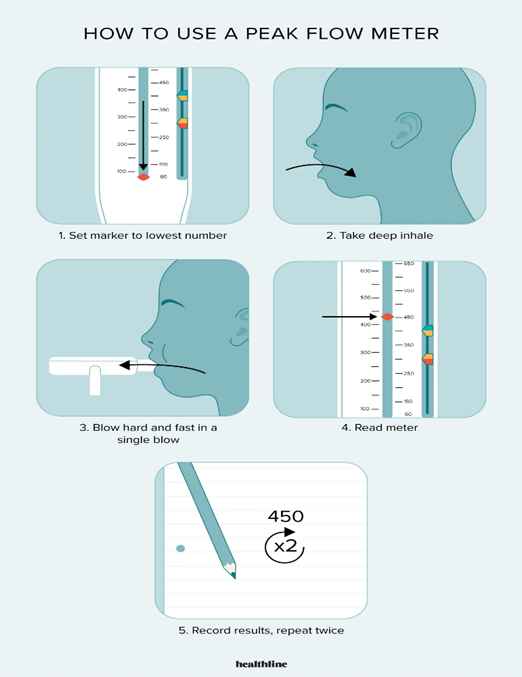
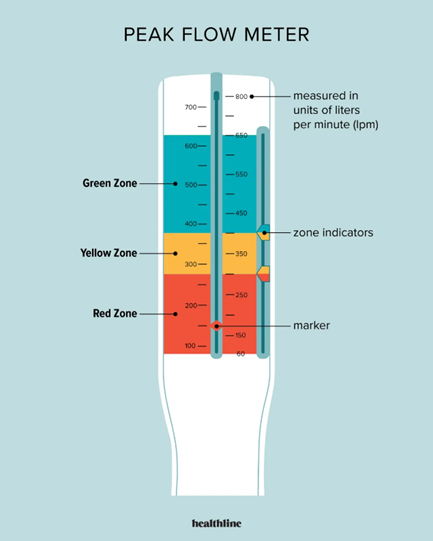
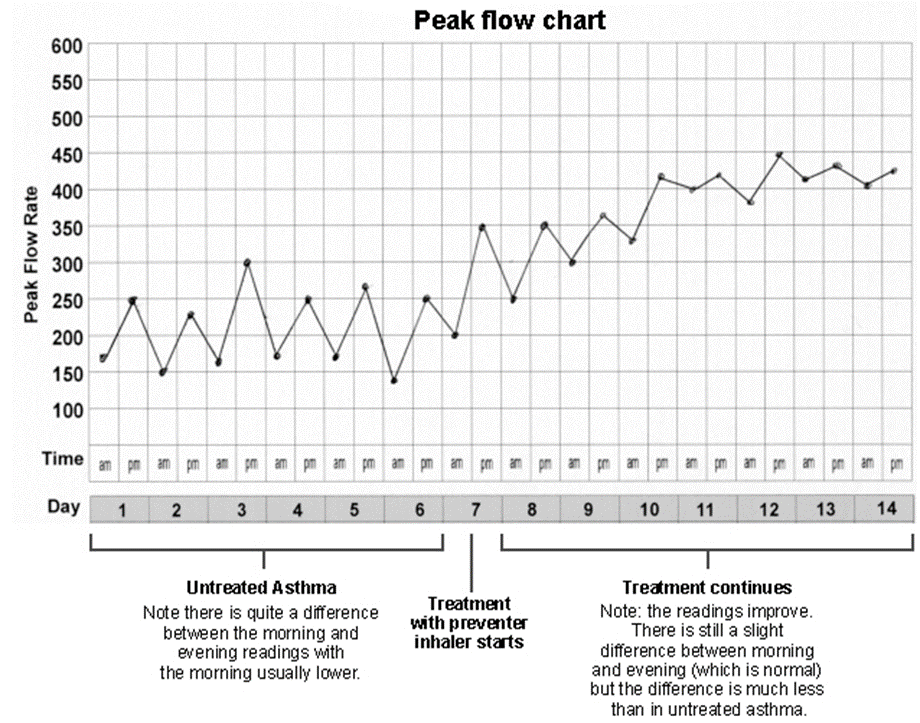
By measuring how fast you're able to breathe out, your peak flow score can indicate whether your airways are narrowed. Peak expiratory flow (PEF) is measured in litres per minute. Normal adult peak flow scores range between around 400 and 700 litres per minute, although scores in older women can be lower and still be normal. FEV1 = forced expiratory volume in one second; PEF = peak expiratory flow.
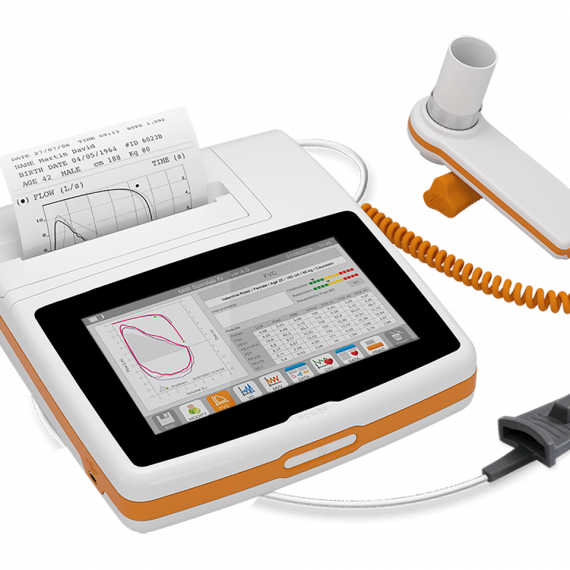
7-inch Touchscreen, all-in-one Spirometer with embedded printer, Real-time test also available on PC, via USB and Bluetooth. Perfect suite in Hospitals and Asthma camps, with its fast and silent built–in thermal printer with customizable printout format. Lightweight for easy mobility, carrying case included, long life Rechargeable Battery.
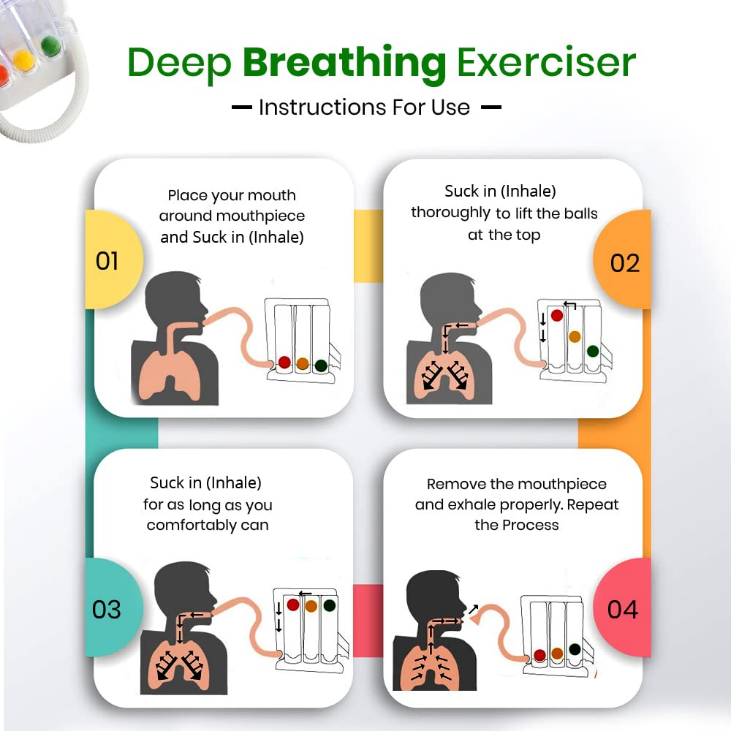

Features of our 3-Ball Spirometer: Color-coded balls in each three chambers prove to be visual incentive to the patient. Air flows into single channel, when it passes through the chamber; it raises each of the three balls depending on the flow inhaled per second. Connecting tube with 12mm OD connector and mouthpiece. Flow rates 600ml/sec, 900ml/sec, and 1200ml/sec by using different colours of ball for easy identification of the flow rates. Can be dis-assembled into parts for cleaning and disinfection. Deep Breathing Exerciser for comprehensive respiratory fitness. Helps achieve optimum lung capacity and restoring disrupted breathing patterns.
Association Between Asthma and Obstructive Sleep:
Asthma and obstructive sleep apnoea (OSA) are the commonest pulmonary diseases worldwide and contribute to significant morbidity and mortality. Indian studies have identified a high prevalence of OSA among patients of moderate to severe asthma which negatively affects quality of sleep and asthma control that further leads to poor quality-of-life in these patients. One study inferred that apnoea-hypopnoea index (AHI) >5/h was found in 15/30(50%) cases with moderate and severe asthma (N=15 each). In moderate asthma 6/15 (40%) and in severe asthma 9/15(60%) were diagnosed to have OSA [11]
Association Between Asthma and Gastroesophageal disease (GERD):
Asthma and acid reflux often occur together in children as well as in adults. It's known that Asthma and acid reflux (especially the severe form- known gastroesophageal reflux disease (GERD) worsen each other. The prevalence of GERD is estimated to be around 30-80% among asthmatics. The proposed mechanisms of GERD induced asthma include a vagally mediated reflex, micro aspiration and altered immune activity. In simple terms GERD causes asthma-like symptoms by two mechanisms: -i) Aspiration of acid particles in the trachea cause coughing, wheezing and pneumonia ii) Acid in the oesophagus causes a reflex phenomenon in the trachea, triggering asthma-like symptoms. This study stresses the need for patients with asthma to be evaluated for gastroesophageal reflux and to be treated with aggressive anti-reflux therapy to reduce morbidity.
Coexistence of allergic rhinitis and asthma in Indian patients:
There is enough evidence of coexistence of Allergic Rhinitis (AR) and Asthma (AS) through (CARAS) survey, and it reinforce the need for early diagnosis and guideline-based management of AR in patients with asthma. The study from 1161 asthma patients with mean age 40.41 [±17.05] years, showed prevalence of coexisting AR was found to be 65.24%, with the highest prevalence (80%) in the southern regions of India. Sneezing (71.78%) followed by watery, runny nose (63.59%) were the most common AR symptoms. Majority (72.32%) of the patients had seasonal AR. Coexistence of AR and asthma was significantly associated with the presence of personal and family history of atopy. Smoking, exposure to biomass fuel, and the presence of pets and animals at home were also significantly associated with AR-asthma coexistence. The usage of oral steroids was significantly higher as 66% patients were prescribed intranasal corticosteroids [13].
Summary
- Asthma is a major and common chronic noncommunicable disease (NCD), affecting both children and adults globally
- India contributes to 12.9 % of Global Asthma cases and 42.4% of global Asthma Deaths. Data from Indian centres that participated in the multicentre current Global Asthma Network showed a significant decline in symptoms of asthma compared to 2005 and 2013 studies.
- An estimated 35 million people are suffering from Asthma in 2023.
- Asthma is a clinical diagnosis, based on a history of characteristic symptom patterns and evidence of variable expiratory airflow limitation. In well-resourced healthcare settings, evidence is derived from spirometry with bronchodilator “reversibility” testing.
- Investigations like X Ray chest and Sinuses are used in complex cases to differentiate TB, Rhinosinusitis, Lung Cancers, as they are scarcely available and are substantially underused (unaffordable or time-consuming in special clinics), and more than one test is often required to confirm airflow variability.
- Most distressing situation is 82% of current wheezers and 70% of subjects with symptoms of severe asthma are not clinically diagnosed as having asthma. The daily use of inhaled corticosteroids (ICS) is 2.5% in subjects with current wheeze and those with symptoms of severe asthma but less than 1% used daily ICS when asthma remained undiagnosed.
- All out efforts need to be made to improve early diagnosis and continuous use of inhalers to minimize the complication and lead almost normal and active life.
References
- Global, regional, and national prevalence of asthma in 2019: Peige Song et.al, J Glob Health. 2022; Published online 2022 Jun 29. doi: 10.7189/jogh.12.04052
- https://www.indianjournals.com/ijor.aspx?target=ijor:lsijls&volume=10&issue=3&article=003
- 2019 Archived National Asthma Data, https://www.cdc.gov/asthma/nhis/2019/data.htm
- Stats on lung health, https://www.asthmaandlung.org.uk/media-centre.
- Paediatric severe asthma: a case series report and perspectives on anti-IgE treatment, BMC Paediatrics volume 18, Article number: 73 (2018)
- Prevalence, time trends and treatment practices of asthma in India: Global Asthma Network study, Mangal Sheetu Singh, et.al, https://openres.ersjournals.com Mangal Sheetu Singh, et.al, ERJ Open Res. v.8(2); 2022 Apr PMC9149387, Doi: 10.1183/23120541.00528-2021
- Prevalence and risk factors for self-reported asthma in an adult Indian population: S. Agrawal, et.al, Int J Tuberc Lung Dis. 2013 Feb; 17(2): 275–282. Doi: 10.5588/ijtld.12.0438
- Asthma, https://my.clevelandclinic.org/health/diseases/6424
- Asthma cases in Chennai double in 5 years, Outdoor pollution the primary cause,
- Case 1: A 12-year-old girl with food allergies and an acute asthma exacerbation, Lop mudra Das, MD .et al, https://doi.org/10.1093/pch/19.2.69
- June 2021The Indian journal of chest diseases & allied sciences 63(2), Anshu Priya et.al DOI: 10.5005/ijcdas-63-2-95 June 2021
- The Prevalence of the Gastro Oesophageal Reflux Disease in Asthmatics, S. Charles et.al, Journal of Clinical and Diagnostic Research 5(4):711-713, January 2011
- Coexistence of allergic rhinitis and asthma in Indian patients, Vikram Jaggi et.al, Lung India. 2019 Sep-Oct; 36(5): 411–416. Doi: 10.4103


