Article In Press : Article / Volume 3, Issue 2
- Review Article | DOI:
- https://doi.org/10.58489/2836-2330/021
Human Suicide, an Overview of Management Strategies
1School of Life Sciences, Shanghai University, Shanghai 200444, PRC.
2College of Science, Shanghai University, Shanghai200444, PRC.
Da-Yong Lu*
Da-Yong Lu, Hong-Ying Wu, Ting-Ren Lu. (2024). Human Suicide, an Overview of Management Strategies. Journal of Clinical and Medical Reviews. 3(2); DOI: 10.58489/2836-2330/021
© 2024 Da-Yong Lu, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 03-06-2024
- Accepted Date: 15-07-2024
- Published Date: 12-07-2024
Human suicide, neurobiology, brain image, psychopharmacology, modern technology, suicide prediction
Abstract
Suicide is still a biologically mystery process with a high rate of human mortality. Early clinical evidence suggests that external and internal stresses may drive human neuropsychiatric instability and suicide behavior. Influenced by different stresses, clinical suicide prevention and treatment needs ever-growing diagnostic and therapeutic transition. Bridging the gap between molecular basis and psychiatric intervene has great medical or pharmaceutical importance. Currently, neural-psychiatric evidence and association has provided profound impacts in suicide knowledge gains in experiments and clinics. A great deal of neurobiological and psychopharmacological study can bring new hope for human suicide prevention in completeness. Public health and therapeutic basis are discussed. Final medical success (molecular targeting and curative therapies) in the clinic will ensure high-quality pharmaceutical exists for great numbers of diathesis-tendency and potential suffers.
Conclusion: Next generation of clinical suicide prediction, pharmacology and therapeutic landscapes will be emerged in the near future.
Introduction
Epidemics analysis
Global suicide death is huge (outnumber the death of war and homicide) [1]. Approximately 2% of human mortality is accounted among all episodes of suicide behaviors [2]. However, the incidence of suicide-induced death (SID) is not average distributed. The rates of SID vary between genders, ages and geographic location. The mortality rates also vary between ways of suicide methods (gas, pesticides, rope, gun or others). These kinds of epidemic information and stress should be analyzed for suicide prediction and management promotion.
Internal (genes or pathogenesis) and external (financial crisis and interpersonal distortion) are associated with human suicide increases. Male suicide ranks secondary leading causes for human death at the age range from 15 to 34 in US [3]. In addition, old male retirees with less economic supports show double rates of human suicide behaviors comparing with average age ranges [4]. Unfortunately, human suicide is not well defined at genetic or molecular levels presently. Given a slow pace of knowledge gains for suicide behavioral and biology, accelerating therapeutic comparison between west and east should be made on medical and pharmacological bases.
Medical knowledge
General picture of biomedical study of suicide pathogenesis and intervention is depicted in early [5-10]. It contains different strategies and methods. Guideline for new diagnosis, technology and therapeutic selection can be updated by systematic investigations in molecular and clinical bases. Different topics in this respect are addressed in the followings.
There was a long history of human suicide record in literature (as long as two thousand years in history in both China and western) [11-12]. However, its medical study was not such long. There is still little pathogenesis profiling and specific drug targeting for suicide behaviors (treatments and prediction) in the clinic before this millennium. To reduce the risk and incidence of human suicide, genetic analysis and molecular clues should be translated. After these efforts and transition, management strategies and therapeutic paradigms for human suicide can be helpful.
Medical Causalities and Diagnosis
Current concept of human suicides
Early clinical evidence suggests that external and internal risk factors or stresses may drive human neuropsychiatric consequences and suicide behavior. However, an accumulated data suggests that human suicide behavior is not an absolutely impulsive act or behaviors. It is possibly a disease-related. After two decades of hard work, association began to emerge between suicide behaviors and different types of human mental diseases [13-17]. To attain a goal of high-quality suicide management, external stresses, pathogenesis cascade and therapeutic targets should be integrated and targeted. (Figure 1)
Different symptoms and disease categories have been associated for the benefits of suicide managements (co-morbidity). Based on co-morbidity modalities, molecular clues, organ dysfunction and potential drug targets were greatly expanded nowadays. Mental health problems are the main pillow for suicide-related therapeutic industry in west. Under this psychiatric modality and framework, new therapies are gradually developing. (Figure 1)
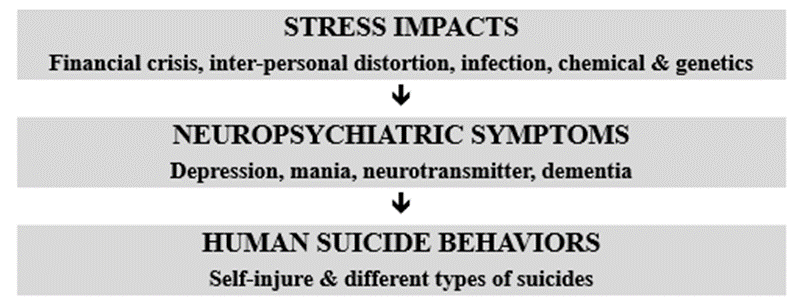
Fig 1: Potential link for suicide onset and progress
Various diagnosis paradigms
A number of anti-psychiatric management strategies are suggested to alleviate potential suicide behaviors and mortality. A long preparedment for combating suicide by existing drug categories are under investigation. Correspondingly, patho-therapeutic relation between suicidal causality and therapeutic paradigms should be built. (Table 1)
Table 1: The linkage between clinical symptoms and neurobiological technology
| Psychological symptoms | Molecular technology |
Language: Speech speed (low) Memory or abstract capability Decision-making: risky and slow Social distortion | Genetic/epigenetic (40 known genes) Cerebral morphology Functional morphology Neurotransmitter (levels and function) |
To gain fundamental knowledge of human suicide, risk factors for genetic predisposition, molecular dysfunctions, multi-omics profiling and neural circuitry connection are well analyzed in statistically significant manner [16-22]. By upholding these biological studies, variable genomic techniques, suicide-associated biomarkers and therapeutic paradigms are emerged after the integration of external variables.
Patho-Therapeutic Mechanisms
Molecular and morphology profiling
Currently suicide ideation is a common feature of all human population. As a result, this public health burden needs to be overcome as early as possible. Since human mental health problems show many identical signs in suicide patients, molecular mechanisms between different psychiatric diseases and suicide ideations should be promoted.
Bad experience may possibly trigger events or behavior of suicide or self-harm. Based on this hypothesis, psychiatric trauma should be aimed for therapeutic drugs or counteractive measures. Drug development pipelines against different suicide deaths or molecules—individually or combinatorial is a modern challenge. To achieve this challenge, clinical evidence and pharmacological targets should be focused in statistical significant manner;
Different molecular pathways for suicide treatments
Major psychiatric diseases associated with suicide (co-morbid) are autism, schizophrenia, mood disorders (depression, uni-polar or bipolar. (Table 2) Diagnostic categories have various drug selection systems and specified in Table 2 and 3.
Table 2: Molecular basis and classification for human suicide targets
| Molecular diagnostic basis | Pathogenesis pathways |
| Neuropsychiatric pathogenesis | Hypothalamic-pituitary-adrenal axis |
| Biomarkers | Bone-derived neurotrophic factor (BDNF) |
| Morphologic characters | structural- or functional magnetized resonance images |
| Neurotransmitters | Dopamine, serotonin and others |
| Patients or relatives | Questionnaire filling |
Table 3: Associations between neurotransmitters and disease categories
| Neurotransmitters | Neuronal diseases |
| Dopamine | Schizophrenia, gabling & hypersexual |
| Serotonin | Depressive diseases & emotional activity |
| Noradrenaline | Normal psychiatric function and neural transmission |
By discovering neuropsychiatric genes or molecules, more effective targeted therapeutics or drugs will be developed [23].
Common means and therapies for suicide reduction
Different types of management strategies in the clinic are listed as
- Education for students, teachers or clinicians [24]
- Stress response mechanisms
- Diathesis and prevention
- Cognitive-behavioral therapy (CBT)
- Restriction for lethal means
- Anti-psychiatric agents
- Drug treatments
- Traditional medicine (herbs) [25]
- Treatment of co-morbid [26]
- High-quality nursery [27-28]
Most available drugs
Currently, the widest used drugs for suicide are ketamine, lithium and clozapine [16]. The effect of ketamine is acute and short. It commonly treats patients in suicide ideation. Its treatment is commonly through injections and responses are quick.
However, lithium and clozapine take effective in long-term and relatively cheaper. They must be aimed on long-term symptoms and disease management.
Importance of basic scientific studies
Since most psychiatric diseases are chronic diseases, curable therapeutics against mental disorders is still a medical dream. It also affects the high-quality of suicide prediction and prevention [29-35].
Development of curative efficacy should be based on targeting genetics and molecules of disease origins. In order to accomplish this challenge, molecular diagnostics and therapeutics for mental diseases should be future trends. However, the understanding of molecular mechanisms of suicide causality is important yet difficult. To elucidate this topic, mental health problem diagnosis is categorized at different molecules and multiple levels.
Future Direction
Modern diagnosis
Neuropsychiatric diagnosis should be a dominant paradigm for mental disorder diagnosis and treatments. Psychiatrists or clinicians review and treat patients from the analysis of psychiatric sign and scores. This pattern of clinical trials was challenging by modern technology (biological profiling from genome to multi-omics) [36-40]. Combination and integration of both inside and outside stresses is obviously better than those of one system.
Molecular targeting for suicide
Currently, drug for human suicide is a new pharmaceutical challenge. In order to change this situation, molecular drug mechanism and target study is indispensable [41-45]. From molecular study, new drug targets and responses should be investigated at genetic or molecular profiles or levels.
Emotional control
According to law of traditional Chine medicine (TCM), human illness is caused by emotional instability and angry. The hidden molecular aberrant in human is not enough to create a disease or suicide behaviors. In context of Chinese medical book, there are recorded of “disease is caused by psychiatric health problems”, “disease pathogenesis origins in human bodies, angry will be a major risk factor for different disease emerge”, “angry” is the main source of most diseases. According to these remarks, we create a modality of human suicide prevention by TCM. (Figure 2).
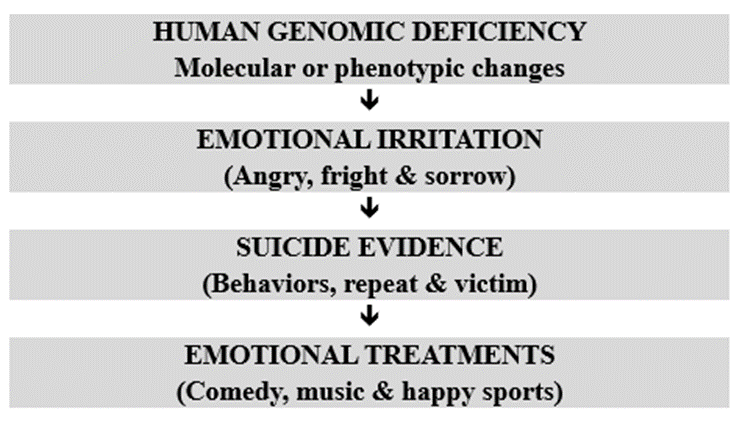
Fig 2: Chinese ways of suicide emergency mechanisms
Knowledge breakthroughs
Neuropsychiatric pathological knowledge can help us to alleviate suicide ideation and behaviors at the greatest rates. To attain this goal, knowledge and technical breakthrough is indispensable, especially curative treatments in the future. Only through molecular biological discovery, a great difference (curative therapy) can be made in the clinical trials.
Conclusion
New vision should be created for the promotion of suicide prevention in the clinic [46-48]. The relationships between chemical, genetic, molecular, morphologic, neurologic, environmental, social and cultural factors should go individually and curable treatments by the utility of bio-agents or PM. In search for suicide-related causations and targeting, molecular biology knowledge is the key [46-48]. By achieving this ambitious plan, new breakthroughs are expecting.
Conflicts Of Interests
Authors declare there is no conflict of interests with other institutes and academies.
References
- World Health Organization: World Health Statistics 2019: Monitoring Health for the SDGs. Geneva, World Health Organization, 2019
- Bondy, B., Buettner, A., & Zill, P. (2006). Genetics of suicide. Molecular psychiatry, 11(4), 336-351.
- Centers for disease control and prevention: WISQARS: Fatal injury reports, national and regional. 1999-2018. https//webappa.cdc.gov/sasweb/ncipc/mortrate.html
- Basta, M., Vgontzas, A., Kastanaki, A., Michalodimitrakis, M., Kanaki, K., Koutra, K., ... & Simos, P. (2018). Suicide rates in Crete, Greece during the economic crisis: the effect of age, gender, unemployment and mental health service provision. BMC psychiatry, 18, 1-8.
- Lu DY. Suicide Risks and Treatments, New Ideas and Future Perspectives. Ed Da-Yong Lu, Nova Science Publishers, 2017, New York, US (ISBN-978-1-53610-601-5)
- Lu, D. Y., Wu, H. Y., Cao, S., & Che, J. Y. (2021). An overview of suicide study. EC Psychology & Psychiatry, 10(3), 37-43.
- Mann, J. J., Michel, C. A., & Auerbach, R. P. (2021). Improving suicide prevention through evidence-based strategies: a systematic review. American journal of psychiatry, 178(7), 611-624.
- Serafini, G.; Salano, P.; Amore, M. Suicidal ideation: a comprehensive overview. Suicidal Ideation: Predictors, Prevalence and Prevention. Ed. Bradley Weaver. Nova Science Publishing. US, 2015, Chapter 1, pp1-42
- Kapur, N., & Gask, L. (2009). Introduction to suicide and self-harm. Psychiatry, 8(7), 233-236.
- Lu, D. Y., Zhu, P. P., Lu, T. R., & Che, J. Y. (2016). The suicidal risks and treatments, seek medications from multi-disciplinary. Central Nervous System Agents in Medicinal Chemistry (Formerly Current Medicinal Chemistry-Central Nervous System Agents), 16(3), 231-239.
- Shandilya S. Suicide and suicide prevention: a historical review. The Research Journal of Social Science. 2018, 9 (12), 35-40
- Lu, D. Y., Wu, H. Y., Cao, S., & Che, J. Y. (2020). Historical analysis of suicide. J Translational Genetics & Genomics, 4, 33.
- Lu, D., Zhu, P., Wu, H., Yarla, N., & Zhu, H. (2016). Human suicide study, is there an association between suicide and mental illness. Metabolomics (Los Angel), 6(186), 2153-0769.
- Na, E. J., Lee, H., Myung, W., Fava, M., Mischoulon, D., Paik, J. W., ... & Jeon, H. J. (2019). Risks of completed suicide of community individuals with ICD-10 disorders across age groups: a nationwide population-based nested case-control study in South Korea. Psychiatry investigation, 16(4), 314.
- Acheampong, A. K., & Aziato, L. (2018). Suicidal ideations and coping strategies of mothers living with physical disabilities: a qualitative exploratory study in Ghana. BMC psychiatry, 18, 1-8.
- Mann, J. J., & Rizk, M. M. (2020). A brain-centric model of suicidal behavior. American journal of psychiatry, 177(10), 902-916.
- Lu, D. Y., Wu, H. Y., & Xu, B. (2021). Pathology study for human suicide. Health and Primary Care, 5, 1-4.
- Krystal, J. H. (2014). Psychiatric disorders: diagnosis to therapy. Cell, 157(1), 201-214.
- Malhotra, D., & Sebat, J. (2012). CNVs: harbingers of a rare variant revolution in psychiatric genetics. Cell, 148(6), 1223-1241.
- Lu, D. Y., & Wu, H. Y. (2021). Neuropsychiatric approaches for human suicide prediction and management. Int J Neuropsychol Behav Sci, 2, 87-91.
- Lu, D. Y., Wu, H. Y., Xu, B., & Lu, T. R. (2021). Neurobiology for human suicide. International Journal of Science and Research Archive, 2(2), 120-125.
- Lu, D. Y., & Wu, H. Y. (2021). Neuropsychiatric insights for human suicide. Int J Scientific Res Updates, 1(2), 11-18.
- Lu, D. Y., Zhu, P. P., Wu, H. Y., Yarla, N. S., Xu, B., & Lu, T. R. (2018). Human suicide risk and treatment study. Central Nervous System Agents in Medicinal Chemistry (Formerly Current Medicinal Chemistry-Central Nervous System Agents), 18(3), 206-212.
- Rutz, W. (2001). Preventing suicide and premature death by education and treatment. Journal of affective disorders, 62(1-2), 123-129.
- Kwon, C. Y., & Lee, B. (2023, May). The effect of herbal medicine on suicidal behavior: a protocol for systematic review and meta-analysis. In Healthcare (Vol. 11, No. 10, p. 1387). MDPI.
- Salis, F., Belfiori, M., Bellisai, A., Bernardini, E., Murtas, M., Piras, R., ... & Mandas, A. (2024). Cognitive Impairment in People Living with HIV and the Impact of Mood: Results from a Cross-Sectional Study. Journal of Clinical Medicine, 13(6), 1631.
- Lu, D. Y., Chen, Y. Z., Lu, D. F., & Che, J. Y. (2019). Patient’s care and nursery in different diseases. Hospice & Palliative Medicine International Journal, 3(1), 28-30.
- Lu, D. Y., Chen, Y. Z., Lu, D. F., & Che, J. Y. (2019). Patient’s care and nursery in modern medicine. Nursery Practice and Health Care, 1(1), 101.
- Desmyter, S., Bijttebier, S., & Heeringen, K. V. (2013). The role of neuroimaging in our understanding of the suicidal brain. CNS & Neurological Disorders-Drug Targets (Formerly Current Drug Targets-CNS & Neurological Disorders), 12(7), 921-929.
- Yuan, Q., Seow, E., Abdin, E., Chua, B. Y., Ong, H. L., Samari, E., ... & Subramaniam, M. (2018). Direct and moderating effects of personality on stigma towards mental illness. BMC psychiatry, 18, 1-10.
- Jiang, J., Yan, Z., Sheng, C., Wang, M., Guan, Q., Yu, Z., ... & Jiang, J. (2019). A novel detection tool for mild cognitive impairment patients based on eye movement and electroencephalogram. Journal of Alzheimer's Disease, 72(2), 389-399.
- Kohyama J. Serotonin is a key neurotransmitter in suicide. Encyclopedia of Suicide. Vol 3, Ed. Torres OB Chapter 9, 105-114, 2018, Nova Science Publishing, US.
- Lu, D. Y., Che, J. Y., Wu, H. Y., Lu, T. R., & Putta, S. (2020). Suicide risks and prevention, neuropathogenic study. Edeweiss Psyi Open, 4, 124.
- Wang, L., Li, J., Liu, H., Wang, Z., Yang, L., & An, L. (2021). Influence Factors for Decision-Making Performance of Suicide Attempters and Suicide Ideators: The Roles of Somatic Markers and Explicit Knowledge. Frontiers in psychology, 12, 693879.
- Cornelius JR, Walker JD, Klima G, Fisher B. Suicidal symptoms among veterans with chronic PTSD evaluated for treatment at a VA hospital. Suicidal Ideation: Predictors, Prevalence and Prevention. Ed. Bradley Weaver. Nova Science Publishing. US, 2015, Chapter 2, pp43-56
- Kleefeld F. HCV-associated neurological disorders. Internal Med Rev. 2017, 3 (9), 1-9
- Marshall M. Roots of mental illness. Nature, 2020, 581, 19-21
- Sokolowski, M., & Wasserman, D. (2020). Genetic origins of suicidality? A synopsis of genes in suicidal behaviours, with regard to evidence diversity, disorder specificity and neurodevelopmental brain transcriptomics. European Neuropsychopharmacology, 37, 1-11.
- Orsolini, L., Latini, R., Pompili, M., Serafini, G., Volpe, U., Vellante, F., ... & De Berardis, D. (2020). Understanding the complex of suicide in depression: from research to clinics. Psychiatry investigation, 17(3), 207.
- Roiser, J. P., Rubinsztein, J. S., & Sahakian, B. J. (2009). Neuropsychology of affective disorders. Psychiatry, 8(3), 91-96.
- McAllister-Williams, R. H., & Ferrier, I. N. (2009). Pharmacological management of unipolar affective disorder. Psychiatry, 8(4), 113-119.
- McAllister-Williams, R. H., & Ferrier, I. N. (2009). Pharmacological management of unipolar affective disorder. Psychiatry, 8(4), 113-119.
- Dranovsky, A., & Hen, R. (2006). Hippocampal neurogenesis: regulation by stress and antidepressants. Biological psychiatry, 59(12), 1136-1143.
- Lu, D. Y., & Lu, T. R. (2021). Drug discovery for suicide management. EC Pharmacol Toxicol, 9, 76-86.
- Lu, D. Y., Lu, T. R., Zhu, P. P., & Che, J. Y. (2016). The efficacies and toxicities of antidepressant drugs in clinics, building the relationship between Chemo-Genetics and Socio-Environments. Central Nervous System Agents in Medicinal Chemistry (Formerly Current Medicinal Chemistry-Central Nervous System Agents), 16(1), 12-18.
- Ramsøy, T. Z., & Skov, M. (2010). How genes make up your mind: Individual biological differences and value-based decisions. Journal of Economic Psychology, 31(5), 818-831.
- Lu, D. Y., Lu, T. R., Che, J. Y., & Zhu, P. P. (2014). Genetic and Bioinformatic Studies of Antidepressant Drug Therapeutic Efficacy and Toxicity: A Current Overview. Recent Patents on CNS Drug Discovery (Discontinued), 9(3), 193-199.
- While, D., Bickley, H., Roscoe, A., Windfuhr, K., Rahman, S., Shaw, J., ... & Kapur, N. (2012). Implementation of mental health service recommendations in England and Wales and suicide rates, 1997–2006: a cross-sectional and before-and-after observational study. The Lancet, 379(9820), 1005-1012.


