Current Issue : Article / Volume 2, Issue 2
- Research Article | DOI:
- https://doi.org/10.58489/2837-3367/008
Sinus Symptoms in Cystic Fibrosis Patients and the Role of Interdisciplinary Care
1Division of Pulmonary Medicine. Departments of Medicine, Medical College of Georgia at Augusta University, Augusta, GA
2MD, Departments of Otolaryngology, Medical College of Georgia at Augusta University, Augusta, GA
3Ph. D, Departments of Research, Medical College of Georgia at Augusta University, Augusta, GA
4MD, Departments of Pulmonology, Medical College of Georgia at Augusta University, Augusta, GA.
V. Taskar
L. Acree, N. Ramaswamy, C. Reyes, S. Kountakis, S. Halder & V. Taskar. (2023). Sinus Symptoms in Cystic Fibrosis Patients and the Role of Interdisciplinary Care. Journal of ENT and Healthcare. 2(2). DOI: 10.58489/2837-3367/008
© 2023 V. Taskar, this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Received Date: 24-05-2023
- Accepted Date: 14-07-2023
- Published Date: 17-08-2023
chronic rhinosinusitis, cystic fibrosis, modulator therapy, otolaryngology, sinus surgery, SNOT-22.
Abstract
Chronic rhinosinusitis (CRS) is known to occur in most cystic fibrosis (CF) patients. This phenomenon occurs because the genetic mutations in CF cause impaired chloride ion transport, which affects water transport and thus leads to thick mucus that cannot be cleared easily in both the lower and upper airways. While improvements continue to be made in treatment modalities for CF patients in terms of modulator therapies, the effect on sinus disease symptoms and the role of the otolaryngologist (ENT) continues to evolve. This study investigates the sinus symptoms of CF patients with comparison to ENT involvement in their care, the histories of polyps and sinus surgeries of these CF patients, and how their initiation to modulator treatment has affected ENT involvement in their care. A retrospective health records review was conducted including patients from Augusta University Adult Cystic Fibrosis Center with stratification based on demographics, mutations, modulators, ENT clinic visits, history of polyps or nasal surgery, and reported symptoms of headaches, olfactory dysfunction, and sleep problems. 98 patients of the Augusta University Adult Cystic Fibrosis Center met the inclusion criteria of this study. Most of the patients with reported ENT visits in the past 10 years were white and between the ages of 20-29. The most common modulator therapy of the CF patients was elexacaftor-tezacaftor-ivacaftor at 72.22%. More than half of the patients had a history of sinonasal surgery, and almost half had a history of polyps. In comparing ENT visits to the initiation of modulator therapy, 24% of the patients with reported ENT visits saw an ENT after starting modulator therapy. CRS can contribute to morbidity in CF patients with most patients requiring surgical intervention in their lifetime. Additionally, persistent sinonasal symptoms can reduce the quality of life in CF patients. Despite treatment with modulator therapies, otolaryngologists continue to have a role in interdisciplinary CF management.CF- Cystic Fibrosis; CFTR- Cystic Fibrosis Transmembrane Regulator; CRS- Chronic Rhinosinusitis; EMR- Electronic Medical Record; ENT- Otolaryngologist
Introduction
Cystic Fibrosis (CF) is an autosomal dominant disease that occurs due to a mutation in the Cystic Fibrosis Transmembrane Regulator gene (CFTR) (1). This gene is located on chromosome7, and a defective CFTR protein causes impairment in the transport of chloride ions through mucus-producing cells (1,2). There are 7 classes of CF, and the class indicates the severity and mechanism of the mutation.3 In patients with functional CFTR proteins, water follows the chloride ions through these epithelial cells, and the mucus created is thin and easily cleared.2 In patients with CF, mucus is thick, dehydrated, and cannot be easily cleared, causing increased susceptibilities to bacterial colonization and serious infections (1,2). Colonization and infections in CF patients are generally associated with their effects on the lungs, but the same mechanism occurs within the sinonasal mucosa, leading to symptoms of inflammation and rhinosinusitis (1,4).
The damage to the upper airways in patients with CF can manifest as nasal polyps, and endoscopic exams in these patients most commonly reveal some type of abnormalities such as polyps, turbinate congestion, or prominent uncinate processes (2,5). A study previously done by Lee et al. suggests that in adult patients with a cystic fibrosis diagnosis, over 60% have chronic rhinosinusitis symptoms (CRS) (4). These symptoms can include rhinorrhea, nasal obstruction, mouth breathing, headaches, anosmia, restless sleep, facial pain, activity intolerance, voice changes, and halitosis (6,7). According to the Fokkens et al., a chronic rhinosinusitis diagnosis requires sinonasal inflammation and either nasal obstruction, congestion, or discharge in addition to one of the following: facial pain or pressure, anosmia or hyposmia, endoscopic signs of CRS, or CT signs of CRS (8).
While management of CF generally includes the input of pulmonologists, endocrinologists, and gastroenterologists, there is a role for otolaryngologists, especially since chronic rhinosinusitis is considered almost universal in CF patients.4 Treatment of CF has been evolving in the last several years with an increased focus on individualized CF management. The specific classes and gene mutations are important in the treatment for CF patients due to targeted modulator therapies, which are novel drugs focused on trying to circumvent the defects and increasing the collective functioning of CFTR in the cell membranes.4
Based on this information, it can be postulated that majority of CF patients have a history of sinonasal symptoms though the exact role of otolaryngology within an interdisciplinary team continues to evolve with the advent of modulator therapies and their unknown long-term effects on these sinonasal symptoms. To investigate this, a health records review was conducted at Augusta University to assess the role that otolaryngologists play in the care of cystic fibrosis patients in terms of sinus surgeries, ENT visits, and sinonasal symptoms with comparison to the initiation of modulator treatments.
Methods
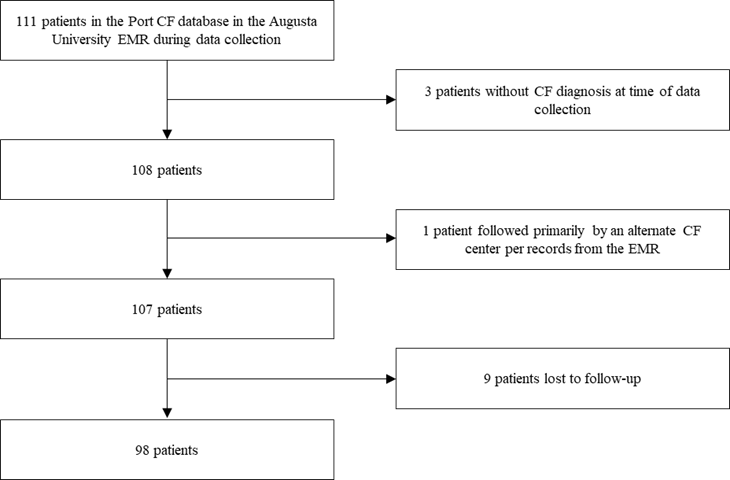
A health records review was conducted by collecting data from the Port CF database and Augusta University electronic medical record (EMR) with local IRB approval (611499-32). This generated a list of patients with cystic fibrosis that was accessed for data collection. Patients in the database with a cystic fibrosis diagnosis, who were over the age of 18 at time of collection, who are followed by Augusta University for cystic fibrosis care, and who have not been lost to follow up were considered for inclusion in the study. In this study, loss of follow up was defined as having no cystic fibrosis appointments in the year 2021 or the years following. The original database included 111 patients. There were 9 patients excluded because of loss of follow up, 1 patient excluded because cystic fibrosis care was managed by an alternate center, and 3 excluded because they did not have a CF diagnosis at the time of data collection. A CF diagnosis was determined based on sweat chloride testing criteria. Of the total 111 in the database, 98 patients met the inclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
Patients included in the Port CF Database within the Augusta University EMR | Patients outside of the Port CF Database in the Augusta University EMR |
Patients diagnosed with CF through sweat chloride testing | Patients not yet diagnosed with CF through sweat chloride testing |
Patients over the age of 18 at time of collection | Patients under the age of 18 at time of collection |
Patients followed by the Augusta University CF center for their CF-related care | Patients with EMR notes documenting that their primary CF care was at an alternate institution |
Patients seen for CF follow-up in 2021 and years following | Patients with their most recent CF appointment occurring before 2021 |
The electronic medical record was reviewed to obtain demographic information such as age, sex, and race. The CF clinic notes were reviewed to gather each patient’s specific gene mutation, current modulator therapy, and the month and year that they began that treatment. Information regarding snoring or other sleep problems, headaches/sinus pain, and/or olfactory dysfunction was also obtained from their chart notes. All visits to the ENT clinic over the preceding 10 years were captured from the electronic medical record, which included details of each patient’s sinonasal surgeries and/or polyps. After data collection was complete, patient information was de-identified, and research was conducted in accordance with ethical principles.
Since data is provided as frequencies (non-parametric), statistical analysis was performed using the Chi-Squared Test. A P-value of <.05 was set as the standard for statistical significance.
Results
Of the 111 patients in the cystic fibrosis database, 98 met the criteria for inclusion. Table 1 gives the demographic information of patients including age, gender, and race with stratification based on whether they were seen by an ENT in the past 10 years. Out of the 98 CF patients from Augusta University Adult Cystic Fibrosis Center, 54 were seen by an otolaryngologist in the last 10 years. The demographics most associated with ENT visits were patients aged 20-29 and of white race with an equal distribution between males and females.
Table 1: Stratification of patients with CF who visited an ENT in the last 10 years by demographic information
| Did see ENT | Has not seen ENT |
Age (years) | ||
| 10-19 | 1 | 0 |
| 20-29 | 28 | 13 |
| 30-39 | 12 | 14 |
| 40-49 | 6 | 7 |
| 50-59 | 3 | 6 |
| 60-69 | 2 | 1 |
| 70-79 | 2 | 2 |
| 80-89 | 0 | 1 |
Gender | ||
| Male | 27 | 25 |
| Female | 27 | 19 |
Race | ||
| White | 45 | 34 |
| Black | 8 | 9 |
| Hispanic | 1 | 0 |
| Other | 0 | 1 |
| Total | 54 | 44 |
Table 2 provides information on the mutations and modulator therapies with stratification based on whether they were seen by an ENT in the past 10 years. Of those with a known mutation, the most common mutation was F508del/F508del for those with a prior ENT visit and those without. Most patients were on elexacaftor-tezacaftor-ivacaftor modulator therapy regardless of ENT visit status.
Table 2: Stratification of patients with CF who visited an ENT in the last 10 years based on molecular genetics and current modulator therapy
| Did see ENT | Did not see ENT |
| Mutations | ||
| F508del/F508del | 23 | 16 |
| F508del/G551D | 2 | 2 |
| F508del/621+1G->T | 3 | 1 |
| F508del/R553X | 3 | 0 |
| Other/unknown part | 21 | 25 |
| None | 2 | 0 |
| Modulator | ||
| Elexacaftor-tezacaftor-ivacaftor | 39 | 31 |
| Ivacaftor | 0 | 1 |
| Lumacaftor and ivacaftor | 1 | 0 |
| None | 14 | 12 |
| Total | 54 | 44 |
Table 3 provides information on the sinonasal symptoms of patients with cystic fibrosis including headaches/sinus pain, sleep disturbance, and olfactory nerve dysfunction with stratification based on ENT visits within the past 10 years. Regarding rhinosinusitis symptoms, 37.8% of the CF patients experienced headaches/sinus pain but were not seen by an ENT. Additionally, 12.2% experienced sleeping problems and 1% experienced olfactory nerve dysfunction but were also not seen by an ENT. Of note, the association between ENT visit history and the symptoms of headaches/sinus pain as well as olfactory nerve dysfunction were statistically significant (P=0.009 and P=0.032 respectively). The association between ENT visit history and reported sleeping problems was not statistically significant (P=0.079).
Table 3: Stratification of patients with CF who visited an ENT in the last 10 years based on sinonasal symptoms
| Did see ENT | Did not see ENT |
| Headaches/Sinus pain | x2 =11.54 | P=0.009 |
| Occasional | 22 | 31 |
| Frequent | 21 | 5 |
| Migraines | 3 | 1 |
| None Reported | 8 | 7 |
| Sleeping Problems | x2 =3.08 | P=0.079 |
| Yes | 24 | 12 |
| None Reported | 30 | 32 |
| Olfactory Nerve Dysfunction | x2 =4.57 | P=0.032 |
| Hyposmia/anosmia | 8 | 1 |
| None Reported | 46 | 43 |
Table 4 includes the polyp history and sinonasal surgery history for the included cystic fibrosis patients. Of the total 98 patients included, 62.2% have a documented history of sinus or nasal surgery in their lifetime. Of the 98 patients, 45.9% have a documented history of polyps.
Table 4: Stratification of patients with CF who have histories of sinonasal surgeries and those with histories of nasal polyps
History of Sinus or Nasal Surgery | History of Nasal Polyps | |
| Yes | 61 | 45 |
| No | 37 | 53 |
| Total | 98 | 98 |
Figure 1 provides information regarding the timeline of the starting year of modulator therapy in comparison to when patients seen by the ENT had their most recent visit. Of the 54 patients who have had an ENT visit in the last 10 years, 35% had seen the ENT in year(s) prior to starting elexacaftor-tezacaftor-ivacaftor in comparison to the 24% who saw ENT in the year(s) after starting elexacaftor-tezacaftor-ivacaftor. Of the 54, 15% saw ENT within the same year of starting elexacaftor-tezacaftor-ivacaftor.
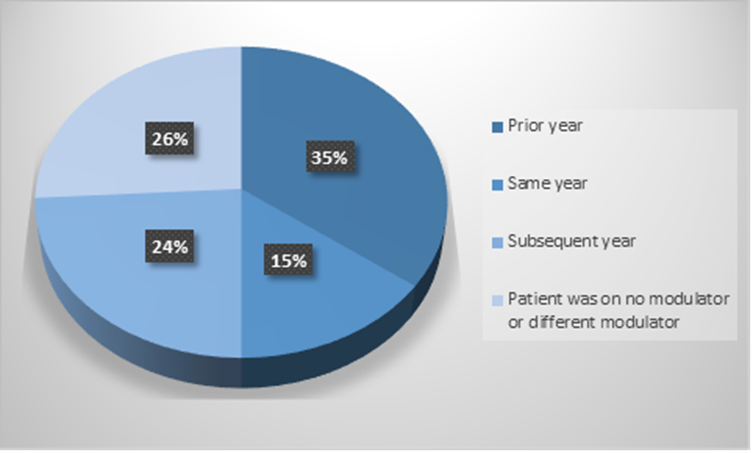
Fig 1: Timeline of most recent ENT visit in comparison to the starting year of elexacaftor-tezacaftor-ivacaftor
Discussion
Despite many cystic fibrosis patients having concomitant chronic rhinosinusitis and necessitating otolaryngology referral, whether the otolaryngologist is an integral part of the CF care team is unclear in both the literature and practice. Around 60% of cystic fibrosis patients are said to have rhinosinusitis, causing symptoms of headaches, rhinorrhea, nasal obstruction, and olfactory dysfunction, symptoms that warrant otolaryngology involvement (9). The current recommendations by the Cystic Fibrosis Foundation task force state that a referral to ENT should occur if a patient has ear, nose, and/or throat symptoms that are recurrent (10). Pulmonology-specific recommendations based on a comprehensive research study is that ENT referrals be placed when the sinonasal symptoms begin affecting a patient’s quality of life (11). However, according to that same research study, otolaryngologists prefer to be part of a patient’s care as soon as a cystic fibrosis diagnosis is received (11). Thus, the recommendations on both sides seem to agree that both pulmonology and otolaryngology have a place in the care plans of cystic fibrosis patients. This current study looked at data collected from the Augusta University Hospital Adult Cystic Fibrosis Center to help understand further the role of otolaryngology in cystic fibrosis patients and to discuss practice-based recommendations to maximize patient outcomes.
In this study, around 38% of patients experienced sinus and head pain, whether it be occasional, frequent, or migraines, and were not seen by an ENT for their symptoms. Additionally, 12% had sleep disturbance and 1% had olfactory dysfunction that were also unaddressed by ENT. Though this does not necessarily indicate a lack of referral or a failure to follow through on the patient’s part, it does show a diminished quality of life for patients living with chronic sinonasal symptoms that could be otherwise relieved with an otolaryngologist’s assistance. Considering this and the recommendations by the Cystic Fibrosis task force, this paper would argue that it may be beneficial for healthcare teams to facilitate an interdisciplinary approach in these patients, involving otolaryngology in care from the beginning.
Over half of CF patients have chronic rhinosinusitis (9). Like most other diagnoses, the first-line treatment is conservative therapy with medical management. The Cystic Fibrosis Foundation task force recommends functional endoscopic sinus surgery for patients with recurrent rhinosinusitis symptoms that fail to improve following medical management, since there is evidence that sinus surgery improves quality of life in these patients (10). Farzel et al. states that around 25% of these patients will go on to need functional endoscopic sinus surgery due to refractory nasal obstruction (11). This surgery, performed to provide patients both functional breathing and the ability to do saline rinses, is done through otolaryngology. The study at Augusta University showed that majority of CF patients included (62%) have received sinus or nasal surgery in their lifetime, more than expected if only 25% of patients will continue to have symptoms following medical management. This data suggests that otolaryngologists have a role to play in the surgical treatment of more patients than previous studies have shown.
Additionally, Farzel et al. states that around 48% of CF patients have nasal polyps in childhood (11). These polyps have a predilection to recur and will do so within the lifetime of 40% of these CF patients with concomitant chronic rhinosinusitis (12). According to the data collected at Augusta University, 46% of these patients have a documented history of polyps, which is similar to the expected statistics. Due to their recurrence, many patients do require surgical treatment in the form of single or multiple surgeries after trialing steroids, leading some to believe that treatment of polyps alone is an issue not thoroughly addressed for CF patients (12).
Modulator therapies are a novel but integral addition to the treatment of cystic fibrosis. Four oral modulators are currently used for CF treatment including ivacaftor, lumacaftor and ivacaftor, tezacaftor and ivacaftor, and elexacaftor-tezacaftor-ivacaftor (13). Each drug can correct for an issue with the CFTR protein such as improving channel opening, protein folding, or protein trafficking, and due to the specific corrections, specific CF mutations will have the most improvements following therapy (13). Elexacaftor-tezacaftor-ivacaftor is specifically for patients homozygous or heterozygous for the F508del allele (13). Around 71% of the total CF patients included in this study were on elexacaftor-tezacaftor-ivacaftor modulator therapy at the time of data extraction. Current literature on modulator therapies investigates their role in improvements in lung function and in decreased pulmonary exacerbations, and there is some evidence of improvements in sinonasal symptoms as well.12 Modulator therapy has been tied to an improvement in sinonasal quality of life and decreased sinonasal symptoms with less evidence of chronic rhinosinusitis on radiologic imaging within a week of initiating treatment with elexacaftor-tezacaftor-ivacaftor (12). A different study noted improvement within 3 months (14).
However, the data from the Augusta University study shows that 24% of the CF patients who had ENT appointments in the last 10 years did so in the year or years following elexacaftor-tezacaftor-ivacaftor modulator therapy initiation. This would indicate that, despite starting modulator therapy, patients still found benefit in otolaryngology referral for their sinonasal symptoms. Hence, even with the advent of modulator therapy, the data would suggest that there is still a key role for otolaryngology in the treatment of cystic fibrosis patients. Considering that elexacaftor-tezacaftor-ivacaftor was approved for modulator therapy at the end of 2019, this role will only grow and evolve as the long-term effects and benefits of modulator therapy are identified and understood.12 However, it remains important to consider an interdisciplinary approach to cystic fibrosis management, with otolaryngology actively involved in patient care.
This study is limited to the availability and accuracy of the information in the Augusta University EMR and cystic fibrosis database when accessed during data collection. The patients could have seen alternative otolaryngologists outside of Augusta University, and those visits were not included in this study. Additionally, the symptoms of headache, sleeping problems, sinus pain, anosmia or hyposmia were recorded based on the reports of the pulmonologists and otolaryngologists. Because this is a retrospective study, there was no way to standardize whether all patients were asked about these symptoms during each of their appointments. If any of these symptoms were unlisted, that does not guarantee that these patients were not experiencing these symptoms, indicating the potential for a larger number of CF patients to suffer from these symptoms. Additionally, modulator therapies are innovative treatments that will require years of future research to fully understand the outcomes and benefits, especially in terms of treating sinus symptoms. Future research could further illuminate how these symptoms are affected based on the age at modulator therapy initiation as well as how the years of use correspond to the degree of symptom benefit.
Conclusions
Addressing the need and role of otolaryngologists is a critical topic that affects most CF patients. We recommend multidisciplinary, same-day follow-up of CF patients regarding their sinonasal symptoms at all pulmonary and primary care appointments to initiate swift care if symptoms necessitate otolaryngology involvement. Alternatively, consecutive appointments with members of these teams could take out scheduling and travel burden on the patients. The Sino-Nasal Outcome Test (SNOT-22) Quality of Life questionnaire is a valuable tool, as it allows assessment of these patients before and after treatment. This could be beneficial in finding the best ways to treat these patients and maximize their quality of life. Despite evolving treatments and modulator therapies, the care of CF patients still requires a multidisciplinary approach.
Disclaimer
The data reported here have been supplied by the medical records at Augusta University Hospital. The authors have seen and approved the manuscript and report no conflicts of interest.
References
- Ji, K. S., Frank-Ito, D., Abi Hachem, R., Issa, K., Johnson, C., Mohamedaly, O., ... & Jang, D. W. (2022). Endoscopic sinus surgery for cystic fibrosis: variables influencing sinonasal and pulmonary outcomes. American Journal of Rhinology & Allergy, 36(3), 307-312.
- Rafeeq, M. M., & Murad, H. A. S. (2017). Cystic fibrosis: current therapeutic targets and future approaches. Journal of translational medicine, 15(1), 1-9.
- De Boeck, K. (2020). Cystic fibrosis in the year 2020: A disease with a new face. Acta paediatrica, 109(5), 893-899.
- Lee, S. E., Farzal, Z., Daniels, M. L. A., Thorp, B. D., Zanation, A. M., Senior, B. A., ... & Kimple, A. J. (2020). Cystic fibrosis transmembrane conductance regulator modulator therapy: a review for the otolaryngologist. American Journal of Rhinology & Allergy, 34(4), 573-580.
- Robertson, J. M., Friedman, E. M., & Rubin, B. K. (2008). Nasal and sinus disease in cystic fibrosis. Paediatric respiratory reviews, 9(3), 213-219.
- Gysin, C., Alothman, G. A., & Papsin, B. C. (2000). Sinonasal disease in cystic fibrosis: clinical characteristics, diagnosis, and management. Pediatric pulmonology, 30(6), 481-489.
- Chaaban, M. R., Kejner, A., Rowe, S. M., & Woodworth, B. A. (2013). Cystic fibrosis chronic rhinosinusitis: a comprehensive review. American journal of rhinology & allergy, 27(5), 387-395.
- Fokkens, W. J., Lund, V. J., Hopkins, C., Hellings, P. W., Kern, R., Reitsma, S., ... & Witterick, I. (2020). European position paper on rhinosinusitis and nasal polyps 2020. Rhinology: official organ of the International rhinologic society.
- Lee, D. J., Sykes, J., Griffin, K., Noel, C. W., Hyung, B., Chokar, K., ... & Lee, J. M. (2022). The negative impact of chronic rhinosinusitis on the health-related quality of life among adult patients with cystic fibrosis. Journal of Cystic Fibrosis, 21(5), 800-806.
- Kimple, A. J., Senior, B. A., Naureckas, E. T., Gudis, D. A., Meyer, T., Hempstead, S. E., ... & Lee, S. E. (2022, September). Cystic Fibrosis Foundation otolaryngology care multidisciplinary consensus recommendations. In International forum of allergy & rhinology (Vol. 12, No. 9, pp. 1089-1103).
- Farzal, Z., Dean, K. M., Sreenath, S. B., Hodge, S. E., Thorp, B. D., Ebert Jr, C. S., ... & Kimple, A. J. (2020, May). Streamlining care in cystic fibrosis: survey of otolaryngologist, pulmonologist, and patient experiences. In International forum of allergy & rhinology (Vol. 10, No. 5, pp. 591-603).
- Stapleton, A. L., Kimple, A. J., Goralski, J. L., Nouraie, S. M., Branstetter, B. F., Shaffer, A. D., ... & Zemke, A. C. (2022). Elexacaftor-Tezacaftor-Ivacaftor improves sinonasal outcomes in cystic fibrosis. Journal of Cystic Fibrosis, 21(5), 792-799.
- De Boeck, K. (2020). Cystic fibrosis in the year 2020: A disease with a new face. Acta paediatrica, 109(5), 893-899.
- DiMango, E., Overdevest, J., Keating, C., Francis, S. F., Dansky, D., & Gudis, D. (2021). Effect of highly effective modulator treatment on sinonasal symptoms in cystic fibrosis. Journal of Cystic Fibrosis, 20(3), 460-463.


