Archive : Article / Volume 1, Issue 1
Case Report | DOI: https://doi.org/10.58489/2836-8657/002
A Giant Retroperitoneal Sarcoma, A Case Report
- General Surgery Department, Al-Basheer Hospital, Amman, Jordan
- School of Medicine, Mutah University, Al-Karak, Jordan.
- Burn and reconstructive surgery Department, University of Texas medical branch, Galveston, Texas, USA
Correspondng Author: Mohammad Abu-Jeyyab
Citation: Hanan Al-Asbahi, Rama Kattua, Marwan Herzallah, Raneem Al-Shnaikat, Md. Al-JaâAwin, A. Nasrallah, Md. Abu-Jeyyab, (2022). A Giant Retroperitoneal Sarcoma, A Case Report. Journal of Surgery and Postoperative Care. 1(1). DOI: 10.58489/2836-8657/002
Copyright: © 2022 Md. Abu-Jeyyab, this is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2022-10-17, Received Date: 2022-10-17, Published Date: 2022-11-22
Abstract Keywords: Retroperitoneum, mass, distention, sarcoma, surgery.
Abstract
Retroperitoneal sarcomas are rare soft tissue tumors that account for only 1%-2% of all solid tumors. The majority of sarcomas occur outside of the retroperitoneum. Retroperitoneal sarcomas account for 10%-20% of all sarcomas, with an overall incidence of 0.3%-0.4% per 100,000 people. Although they can occur at any age, they are most common in the fifth decade of life.
The established diagnosis is based on CT or MR imaging, which is used in patients with these tumors to detect local and distant metastases as well as for preoperative surgical planning.
Surgery is the most common form of treatment for retroperitoneal sarcoma.
And the surgical team discussed the condition of a 28-year-old patient who had been hospitalized.
Introduction
Retroperitoneal sarcoma (RPS) is a rare type of soft tissue cancer that develops from the body's connective tissues and extremely malignant cluster of tumors that arise from mesenchymal cells of retroperitoneum and accounts for 9-15% of total body sarcomas [1]. The mean incidence of retroperitoneal sarcoma is 2.7 per million [2]. In fact, soft-tissue sarcomas which are mesenchymal neoplasms account for up to 1% of all newly diagnosed malignancies at a rate of 3.6 per 100,000 per year and visceral sarcoma of 2.0 cases per 100,000 population per year [3,4]. The overall male to female ratio was 1.1:1; nevertheless, a female predominance of visceral sarcomas was recorded at rate of 1.4: 1; whereas a (1.3: 1) of male preponderance for soft tissue sarcoma in general is found [4].
There are several subtypes of RPS, the most frequent sarcoma subtypes in the retroperitoneum in adults over 55 are well differentiated liposarcoma (WDL) and dedifferentiated liposarcoma (DDL) (40%) and leiomyosarcoma (LMS) (27%). In younger age groups leiomyosarcoma becomes more common than liposarcoma [2]. RPS are usually asymptomatic. On the other hand, in case their size reaches great dimensions they may produce symptoms related to their location and the presence of adjacent vital structures. At diagnosis, the mean size was elicited to be 15–18 cm. To establish a diagnosis, a thorough history and physical examination ought to be obtained followed by imaging studies which is assembled by abdominal and pelvic computed tomography (CT) [1,2]. Chest CT scan have to be performed for the sake of staging if malignancy is highly suspected by clinical evaluation. More importantly, MRI could be used in situations where CT scan is not an option; contraindicated. Also, tumor marker serum lever might assist in diagnosis such as LDH, AFP, bHCG. In addition, a percutaneous biopsy may be required for a definitive diagnosis though not routinely performed [1].
Retroperitoneal sarcomas are managed mainly by surgical intervention. In that However, the surgical excision with microscopically negative margins is considered the cornerstone of treatment. The role of neoadjuvant chemotherapy is not well defined in retroperitoneal sarcomas due to the rarity of the disease and therefore is often extrapolated from trials that include extremity sarcoma [5].
Surgical resection with negative margins is the consistent prognostic factor for RPS. The inability to achieve free microscopic surgical margins is not uncommon [5,6]. This is attributed to the anatomic constrains or local tumor invasion. Not to mention that the histologic grade plays an ultimate role in defining the prognosis factors. It is reflected in the extent of differentiation; in that grading is designated as grade 1, G1 (well-differentiated), grade 2, G2 (moderately well-differentiated), or grade 3, G3 (poorly differentiated/undifferentiated) depending on the degree of cytologic atypia, number of mitoses, and presence and extent of necrosis. (6) The retroperitoneal sarcomas prognosis is relatively poor with an overall survival percentage of 36–58% [7].
In this case report of a twenty-eight-year male with previous history of testicular cancer new presentation of abdominal swelling discovered to be a retroperitoneal sarcoma is demonstrated.
Case presentation
A 28-year-old male patient, who has history of testicular cancer for which orchiectomy was done many years ago, presented to outpatient department complaining of an abdominal swelling for two months prior to presentation. This condition onset was gradual with progressive course and association of dull-aching abdominal pain and significant weight loss; more than 10% of total body weight, but no other symptom. On clinical examination, generally, the patient has low body built. On local assessment, there is a huge palpable, non-tender, ill-defined, firm and non-pulsating abdominal swelling distorting the contour of abdomen and filling both flanks with no skin changes. Right testis was not palpable; surgically excised. while left one has normal consistency, no tenderness nor palpable masses.
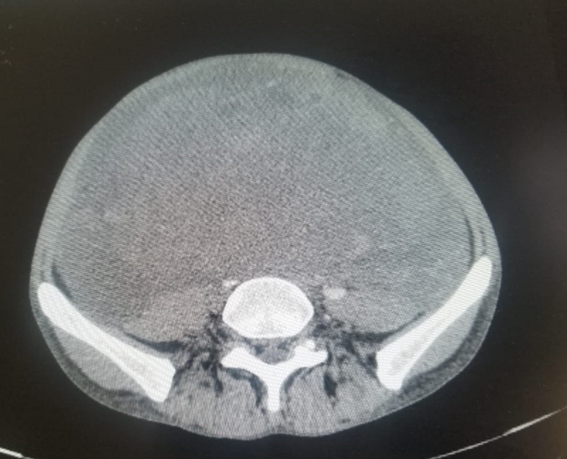
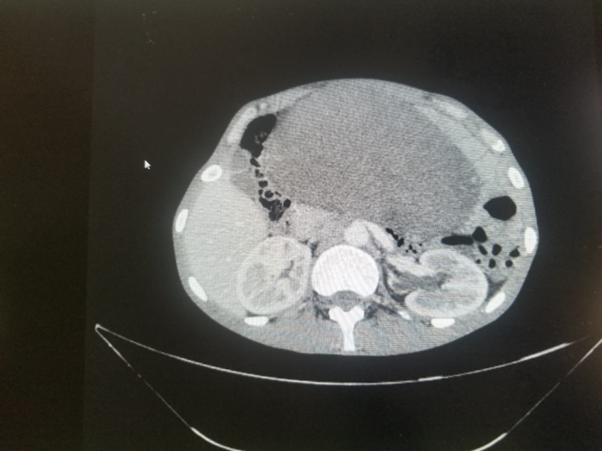
Abdominal and pelvic CT- scan with oral and IV contrast was done. It demonstrated the presence of a huge heterogeneous soft tissue with cystic component mass legion occupying most of the abdomen and pelvic region with increased enhancement of the solid component figure 1,2. Abdominal aorta was compressed by this tumor. However, both ureters, bowel loops, and urinary bladder were encased. Also, moderate hydronephrosis with ureteric dilatation due to compression was present.
Moreover, laboratory investigations show microcytic anemia (Hb 9.4 g|dl, MCV 67), otherwise all other investigations including tumor markers, and metabolic panel were within the normal range.
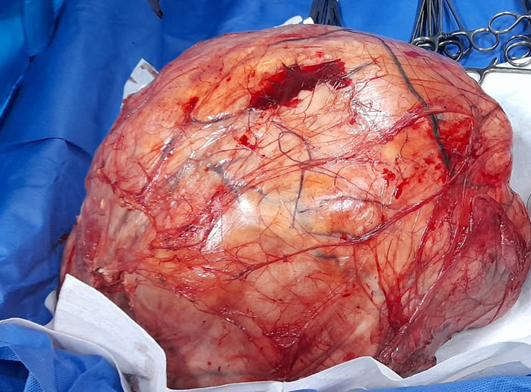
laparotomy was done for excision of the retroperitoneal mass was performed after pre-operative preparation of the patient figure 3. The excised mass was sent to histopathology.
Discussion
Retroperitoneal sarcomas (RPS) are soft tissue sarcomas that present in retroperitoneal region, and originates from mesenchymal tissues including muscle, fat, fibrous tissue, and blood vessels (1,2). They are considered rare as only 9-15% of all adult soft tissue sarcomas (STS) present in the retroperitoneum [3]. There are three principal kinds of sarcoma corresponding to different clinicopathological entities with specific progression, and individual different management means: bone sarcomas, visceral sarcomas that develop in a specific organ and soft tissue sarcomas (STS) arising in connective tissue and extra-osseous connective tissue; these represent about 1% of all adult cancers [4].
The retroperitoneum environment allows sarcomas to grow large before giving any noticeable symptoms [5]. RPS has more than 80 histological subtypes [1], the most common subtype in adults above 55 years of age are the liposarcomas specifically the well-differentiated and dedifferentiated liposarcoma (40%), followed by leiomyosarcoma (27%). On the contrary, leiomyosarcomas are more common than liposarcomas in younger age groups [2].
In general, retroperitoneal liposarcomas peaks in patients 6 to 7 decades of life with no specific race or sex predominance [6]. However, in this presented study our patient is in his 3rd decade of life (28 years old).
There are some associations between soft tissue sarcomas (STS) and various hereditary cancer syndromes including Li-Fraumeni and neurofibromatosis type 1, however; RPS generally arise as a sporadic entity. Rarely, RPS can be a late complication of radiation treatment [1].
Retroperitoneal sarcomas are frequently discovered incidentally with cross-sectional imaging used for another purpose. Yet, some patients present with abdominal or back pain as considered the most common symptoms, or they can even present with weight loss, anemia, palpable abdominal mass or signs of bowel or ureteral obstruction [5].
This is consistent with the main complaint of the presented case, as the patient in this study was mainly suffering of diffused abdominal pain along with clinically significant weight loss
For a definitive diagnosis we need a combination of CT scan and percutaneous needle biopsy to exclude other retroperitoneal tumors particularly lymphoma, adenocarcinoma, germ cell tumor, and paraganglioma. The diagnosis in this case report was initially established by CT scan and confirmed lately by an excisional biopsy (post-operatively).
However, when CT scan is contraindicated, MRI can be used instead, yet; the isolate use of ultrasound is still not recommended. Despite the limited role of PET scan in retroperitoneal sarcomas assessment, it can still be used in staging other retroperitoneal tumors, such as lymphoma and adenocarcinoma. A biopsy review by an expert pathologist is fundamental which includes an extensive immunohistochemical panel plus access to standardized molecular diagnostic tests if necessary. It is discouraged to take intraoperative biopsy if the retroperitoneal mass is first found during operation because it is considered non-diagnostic and it may disrupt the tumor planes [1].
Because of their location, huge size, and frequently aggressive clinical behavior, RSTS remain difficult to treat. The retroperitoneal sarcomas prognosis is relatively poor with an overall survival percentage of 36–58% [7]. Prognosis is mainly defined by three major factors: the grade of the sarcoma, resection completeness and disease multifocality. The 5-year survival rate is inversely proportional to the tumor mitotic activity which determine the grade of the tumor. The goal of complete resection of the tumor with a microscopically negative margin (R0) usually fails due to the large size of the retroperitoneal sarcomas at presentation and their close proximity or even invasion of nearby vital structures. Multifocal disease restricts the possibility of a complete resection of all tumors, which is essential to a long-term survival [1].
In our case, the patient had undergone surgical intervention with a complete excision of the mass with good recovery.
Conclusion
Treatment and management plan of retroperitoneal sarcomas should be done under a multidisciplinary discussion guidance. This would allow for better outcome and prognosis. Moreover, further trials should be commenced to standardize management of these patients including determination the efficacy of radiotherapy and chemotherapy.
References
- Gladdy, R.A., Gupta, A. and Catton, C.N., (2016). Retroperitoneal sarcoma: fact, opinion, and controversy. Surgical Oncology Clinics, 25(4), pp.697-711.
- Messiou, C., Moskovic, E., Vanel, D., Morosi, C., Benchimol, R., Strauss, D., Miah, A., Douis, H., van Houdt, W. and Bonvalot, S., (2017). Primary retroperitoneal soft tissue sarcoma: Imaging appearances, pitfalls and diagnostic algorithm. European Journal of Surgical Oncology (EJSO), 43(7), pp.1191-1198
- Pham, V., Henderson-Jackson, E., Doepker, M.P., Caracciolo, J.T., Gonzalez, R.J., Druta, M., Ding, Y. and Bui, M.M., (2016). Practical issues for retroperitoneal sarcoma. Cancer Control, 23(3), pp.249-264.
- Honoré, C., Méeus, P., Stoeckle, E. and Bonvalot, S., (2015). Soft tissue sarcoma in France in 2015: epidemiology, classification and organization of clinical care. Journal of visceral surgery, 152(4), pp.223-230.
- Mullinax, J.E., Zager, J.S. and Gonzalez, R.J., (2011). Current diagnosis and management of retroperitoneal sarcoma. Cancer Control, 18(3), pp.177-187.
- Vijay, A. and Ram, L., (2015). Retroperitoneal liposarcoma. American journal of clinical oncology, 38(2), pp.213-219.
- Garcia-Ortega, D.Y., Villa-Zepeda, O., Martinez-Said, H., Cuellar-Hübbe, M. and Luna-Ortiz, K., (2016). Oncology outcomes in retroperitoneal sarcomas: prognostic factors in a retrospective cohort study. International Journal of Surgery, 32, pp.45-49.


