Archive : Article / Volume 2, Issue 2
Case Report | DOI: https://doi.org/10.58489/2836-2187/013
Scrub Typhus Re-Emergence of The Neglected, Silent Killer in Himachal Pradesh (India)
1M.D. Senior Resident Department of Microbiology, IGMC Shimla India
2M.D. Senior Resident Department of Paediatrics, IGMC Shimla India
3Prof Department of Paediatrics Dr. RPGMC Tanda Himachal Pradesh India.
Correspondng Author: Pankaj Katoch*
Citation: Pankaj Katoch, Vipin Roach & Sanjiv Chaudhary. (2023). Scrub Typhus Re-Emergence of The Neglected, Silent Killer in Himachal Pradesh (India). Journal of Microbes and Research. 2(2). DOI: 10.58489/2836-2187/013
Copyright: © 2023 Pankaj Katoch; this is an open-access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Received Date: 2023-07-06, Received Date: 2023-07-06, Published Date: 2023-07-22
Abstract Keywords: Zoonoses, Hepatomegaly, Splenomegaly, Pediatric, Bicytopenia, Pancytopenia, Acute Encephalitis Syndrome (AES)
Abstract
Scrub typhus is one of the common causes of fever in the foothills of the Himalayan region of India, affecting almost all age groups of patients. Scrub typhus is a zoonotic mite-borne bacterial disease that is transmitted to the population by the bite of larvae of the infected trombiculid mites that bite humans. Currently, scrub typhus appears to be re-emerging and spreading in the non-endemic areas with alarming antibiotic resistance patterns. It is a threat to more than a billion people and causes significant mortality worldwide. Clinical features can present in a variety of ways in patients suffering with scrub typhus. It causes multiple organ dysfunction syndrome and mortality can range 60-70% without effective therapy. Scrub Typhus presenting with bicytopenia, pancytopenia, hepatomegaly, and splenomegaly. This present study aims to know the varied clinical presentation in scrub typhus patients with Pancytopenia and Bicytopenia and the incidence of hepatomegaly and splenomegaly in the paediatric age group. Prospective observational study conducted in the Department of Paediatrics in Dr. RPGMC Tanda Himachal Pradesh (India). The study included all patients except those falling in the exclusion criteria and only after informed written consent. A total of 37 children admitted with scrub typhus bicytopenia and pancytopenia were enrolled for one year, that is from March 2013 to March 2014. Bicytopenia was observed in 30 patients (81.08%) and pancytopenia in 7 (18.91%) cases in typhus patients. Hepatomegaly was observed in 28 patients (73.68%) and splenomegaly in 16 patients (42.10%). Anaemia was seen in 35 (94.59%) patients. Males 13 were less affected than females 24 with a male-to-female ratio of .54 to 1. The most common age group affected was 11-15 years with female prudence with a male: female ratio of 0.54:1. Pallor was the most common sign in 35 (94.59%) followed by hepatomegaly 28(73.68%) and splenomegaly in 16(42.10%) patients. It is very important to start empirical therapy in a patient with fever and multiorgan dysfunction syndrome for scrub typhus to reduce mortality. There is an urgent need to establish next-generation metagenomic sequencing centers in the region at the tertiary-level institutes for the detection of new antigenic variations.
Distribution Of Disease
Scrub typhus is most prevalent on the land known as the Tsutsugamushi triangle ranging north from eastern Russia, Japan, to Papua New Guinea, and Northern Australia to the southeast, and on the north western border to the Arabian Peninsula, and the Maldives and Re-Union islands to the southwestern side. Scrub typhus is endemic in India, Pakistan, Afghanistan, Bangladesh, China, Taiwan, South Korea, Far Eastern parts of Russia, Japan, Papua Neuve Guinea, and some parts of northern Australia. As scrub typhus has been isolated in parts of countries but its presence everywhere cannot be denied.
Pathophysiology
The organism multiplies at the eschar or bite site and spreads to various organs. The Pathology is due to infection of the vascular endothelium. Vasculitis can affect vital organs such as the lungs, liver, brain, kidney, meninges, and skin. The presentations of severe life-threatening complications such as multiorgan dysfunction syndrome can occur. Severe multiorgan dysfunction syndrome can be jaundice, acute renal failure, pneumonitis, acute respiratory distress syndrome (ARDS), myocarditis, septic shock, meningoencephalitis, pericarditis. Acute interstitial pneumonia can present in vasculitis due to scrub typhus because the lungs are believed to be the target organ of this disease.
Molecular Characteristics
O. tsutsugamushi has a type-specific protein, the 56kDa protein, that is, unique to it. As the protein sequence is unique and has cross-reacting epitopes, changes in the sequence have led to differences in the genetic diversity of O. tsutsugamushi. It possesses an immunogen located on the outer membrane surface of O. tsutsugamushi and elicits antibodies.
Introduction
Scrub typhus (Orientia Tsutsugamushi) is a zoonotic intracellular gram-negative bacterial disease transmitted by zoonotic mites and is transmitted to the population by infected trombiculid mites. In a time, interval of 5 to 14 days, clinical signs and symptoms begin to appear, the incubation period in some cases can extend to 21 days. After a bite by Leptotrombidium mite patients starts exhibiting varied clinical features. [1] The disease puts more than 5 million people at high risk and has become a significant occupational hazard in rural workers, adults in agricultural activities, forest occupation workers, soldiers stationed in temporary camps, people residing near bushes and wood stock. [2] Mortality was previously severe and, in some areas, increased to 60% [3] but targeted and effective antibiotics are now available. Clinically presenting features may be nonspecific such as fever, headache, and myalgia, eschar/ rash, or a flu-like disease, but the disease presents in a way that requires confirmation of diagnosis by the laboratory. The characteristic and pathognomic of this disease is necrotic eschar at the bite site. It manifests as a papule at the site of feeding chigger, ulcerates, and progresses to a black crust lesion like a burn to the skin of cigarettes. It occurs before the onset of symptoms and fever. The presence of eschar supports the diagnosis, but its presence can be variable [4] It is more easily seen and diagnosed in Caucasian and East Asian patients compared to dark-skinned South Asians. [5]. The disease generally presents in patients with fever, myalgia, rash, jaundice, thrombocytopenia, capillary leak syndrome, hepatomegaly, splenomegaly, central nervous system (CNS) involvement, and diffuse lymphadenopathy. In the patient, it can present as meningeal involvement, focal neurological deficits, or encephalomyelitis. [6]. Orientia tsutsugamushi is a well-established reason for acute encephalitis syndrome (AES). Other diseases such as the West Nile virus, Japanese encephalitis virus, and leptospirosis have been identified as key reasons for AES. [7] Recently it is been reported from non-endemic areas and with different antibiotic resistance profiles. Pallor is a common but significant sign encountered in pediatric clinics. It can, on the one hand, be due to simple entities like nutritional anaemia but on the other way hand, this can be the first manifestation of serious life-threatening malignancies like leukemia. A comprehensive study is required to identify the cause of the pallor because the etiologies are diverse. There is a wide spectrum of causes that can range from congenital to acquired diseases of pancytopenia and bicytopenia. The etiology of bicytopenia and pancytopenia can range from marrow suppression to infiltration due to life-ending malignancies. [8,9]. The nutritional causes of pancytopenia are relatively more common in developing countries compared to western countries. The generally implicated causative diseases reported in pediatric patients are aplastic anaemia, megaloblastic anaemia, infections such as malaria, enteric fever, leishmaniasis, Fanconi anaemia, malignancies such as acute leukemia, and myelodysplasia. [10] Pancytopenia presents due to marrow replacement or failure and can also occur due to splenic pooling or the peripheral destruction of mature cells. The severity of bicytopenia and pancytopenia and the causative factors are crucial in the management of these patients. [11]Clinical presentation of bicytopenia and Pancytopenia ranges from fever, mild pallor to severe anaemia, tendencies including petechial, bruises, and bleeding in the organs leading to signs such as hepatomegaly and splenomegaly and some life-endangering emergencies. (8) The findings of marrow can vary depending on the causative factors, from normocellular to hypercellular, overshadowed by malignant cells. A decrease in hemopoietic cells can occur as a result of infections, drugs, toxins, or infiltration of malignant cells leading to hypocellular marrow, whereas normocellular or hypercellular marrow can be found in conditions of hematopoiesis, line maturation, and peripheral sequestration of cells, including megaloblastic anaemia and hypersplenism. (12)
Materials and Methods
Written consent in English and Hindi was obtained from the guardian or the patient's parents. In all cases, hematoxylin and eosin staining was done. Special stains such as Perl’s stain, PAS stain, Reticulin stain, etc. were applied when necessary. IgM ELISA was performed on serum samples using the Scrub Typhus Detect test (InBios International, Inc., Seattle, WA, USA) according to the manufacturer's instructions. An optical density (OD) >0.5 was determined to be positive.
. Inclusion Criteria
1. Hospitalized children aged 1 to 18 years.
2. Showing all or any two of the following: and measured by automatic cell counter and reconfirmed by blood culture, which is defined as
a. Haemoglobin < 10gm>
b. White blood cell count <4>
c. Platelet count< 1500>
3. Consent is given by the guardian or the parents of the patient.
Exclusion Criteria
A total of 37 children admitted with bicytopenia and pancytopenia were enrolled from March 2013 to March 2014 ( a one-year prospective study). The following results were noted and analyzed according to age group. The age range in the study group was 1-18 years and a mean value of 11.77 ± ± 4.67 years. The most common group affected was 11-15 years of age 21 (42%) and the least affected age group was 1-5 years (14%).
Other Investigations
For the diagnosis of scrub typhus, Weil Felix's titre of more than 1:80 was considered positive. The diagnosis was confirmed by an enzyme-linked immunoassay Ig M antibody in a positive Weil Friedrich test. In assays of 37 patients, IgM antibody was positive. Blood cultures were performed in all cases with suspected sepsis.
Statistical Analysis
Chi-square was used for statistical analysis. A p-value of <.01 was considered statistically significant.
Results
A total of 37 children admitted with bicytopenia and pancytopenia were enrolled from March 2013 to March 2014 (A prospective study of one year). The following results were recorded and analyzed according to age group. The age range in the study group was 1-18 years with a mean of 11.77 ± ± 4.67 years.
The most common age group affected was 11-15 years 21 (42%) and the least age group affected was 1-5 years (14%). Bicytopenia was observed in 30 (81.08%) and pancytopenia in 7 (18.91%) cases with infection. All cases had anaemia and thrombocytopenia along with leucocytosis.
Discussion
In this study, patients presented with various clinical symptoms and signs. The commonest presenting symptoms of high-grade fever with chills, shortness of breath, and jaundice are nonspecific for tropical fevers. [13] Treatable bacterial diseases such as leptospirosis and scrub typhus are grossly underestimated due to the absence of clinical suspicion and the lack of diagnostic facilities, especially in developing countries. It involves the vasculitis and perivasculitis systems of humans. [14]
This neglected disease must be considered in the diagnosis of those with acute febrile illness or acute encephalitis syndrome, mainly during or after the rainy season, when the grass is abundant in regions endemic to scrub typhus. [15] Diagnosis is based on clinical skills and suspicion, making the attending physician send a sample for investigation, the failure to properly diagnose the disease most likely results in inadequate treatment with less effective β-lactam–based regimens that add to increase, misuse, overuse of antimicrobial therapy and ultimately lead to the development of antimicrobial resistance and an increase in mortality in recent years. Scrub typhus is re-emerging and is becoming a major cause of AES in many parts of India, especially during the monsoon and post-monsoon season. (17) The history of occupation, work profile, and ecological background of the patients where jungles meet human settlements, can be valuable tools in suspected scrub typhus. Scrub typhus can manifest as fever and is quite difficult to distinguish from other prevalent diseases such as typhoid, dengue, and leptospirosis and is generally missed by health care personnel due to symptoms that overlap with other diseases. [16] Splenomegaly was present in 42.10% of the patients. Another study from north India has reported a higher rate of 59%.[18]
Early diagnoses of bicytopenia and pancytopenia and their underlying pathology are very crucial to prognosis and need clinical evaluation and a complete range of exercises. Pallor, bleeding, hepatomegaly, and splenomegaly are generally associated with benign conditions. Fever and lymphadenopathy are generally due to infectious causes. The most common signs in cytotoxic drug-induced or patients receiving immunosuppressive drugs are lymphadenopathy, hepatomegaly, and splenomegaly.
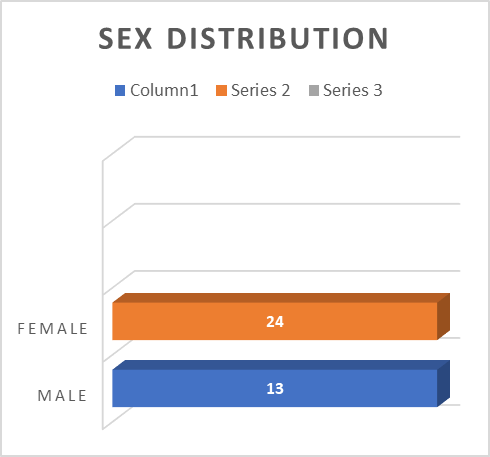
In the present study, a total of 37 children admitted with bicytopenia and pancytopenia and scrub typhus were enrolled for one year (2013-2014) and evaluated. The age range in the study group was 1-18 years with a mean ±S. D age of 11.8 ± 4.62 years. The age group most commonly affected in the present study was found to be of 11-15 years old with 85% of the cases reported from this age group and the least affected age group with 2 cases was 1-5 years. As far as the distribution of these two hematologic disorders in different sex groups was concerned, the number was greater in women (28 %) than in men (22%) with a male vs. female ratio of 0.54:1. Table 1 in the Annexure.
Table 1: Showing Sex distribution
| Sex | Total % |
| Male | 13 (35.13%) |
| Female | 24 (64.86%) |
Leptospirosis, dengue, and malaria were ruled out for all case-patients.
It was found in the study that the incidence of bicytopenia (81.08%) was found to be significantly higher than that of pancytopenia, with only 18.91
Conclusions
The most common age group affected was 11-15 years with female prudence with a male: female ratio of 0.54:1. The age group most commonly affected was 11-15 years with female prudence with a male: female ratio of 0.54:1. Pallor was the most common sign in all 35 (94.59%) followed by Hepatomegaly 28 (73.68%) and Splenomegaly in 16 (42.10%). It is very important to start empirical therapy in a patient with fever and multiorgan dysfunction syndrome for scrub typhus to reduce mortality. Laboratory parameters such as leucocytosis, thrombocytopenia, and elevated transaminase should be reviewed for correlation. There is an urgent need to establish next-generation metagenomic sequencing centers in the region at the tertiary level institutes for the detection of new antigenic variations.
Recommendation
The latest reports of developing antimicrobial resistance have caught the attention of physicians and epidemiologists, raising the interest reviewed in the development and testing of novel diagnostics to facilitate medical diagnosis. Although cytopenia is reported to be commonly associated with the malignant condition in our condition, scrub typhus infection emerged as the main cause of cytopenia in our study. Therefore, it is recommended that in all geographical areas where scrub typhus is endemic, an appropriate investigation of this treatable infection is carried out. Therefore, in the northern region of India, increasing awareness of the disease and characteristics of the disease will help reduce the mortality of this infectious disease.
Generated Ethics Statement
This study was performed in accordance with the Declaration of Helsinki. This human study was approved by Dr.Rajender Prasad Government Medical College Kangra at Tanda - approval: HFW-DRRPGMC/SACPR/2013/7 All parents, guardians, or next of kin provided written informed consent for the minors to participate in this study.
We confirm that all patient's parents or relatives gave written informed consent.
Funding Statement
Not applicable.
Conflict of Interest Statement
Not applicable.
References
- Xu, G., Walker, D. H., Jupiter, D., Melby, P. C., & Arcari, C. M. (2017). A review of the global epidemiology of scrub typhus. PLoS neglected tropical diseases, 11(11), e0006062.
- Beran, G. W. (Ed.). (2019). Handbook of Zoonoses, Section a: Bacterial, Rickettsial, Chlamydial, and Mycotic Zoonoses. CRC press.
- McDonald, J. C., MacLean, J. D., & McDade, J. E. (1988). Imported rickettsial disease: clinical and epidemiologic features. The American journal of medicine, 85(6), 799-805.
- Mahajan, S. K., Rolain, M., Kashyap, R., Bakshi, D., Sharma, V., Prasher, B. S., Pal, L. S., & Raoult, D. (2006). Scrub Typhus in Himalayas. Emerging Infectious Diseases, 12(10), 1590-1592.
- Kim, D. M., Won, K. J., Park, C. Y., Yu, K. D., Kim, H. S., Yang, T. Y., ... & Shin, H. (2007). Distribution of eschars on the body of scrub typhus patients: a prospective study. The American journal of tropical medicine and hygiene, 76(5), 806-809.
- Sankhyan, N., Saptharishi, L. G., Sasidaran, K., Kanga, A., & Singhi, S. C. (2014). Clinical profile of scrub typhus in children and its association with hemophagocytic lymphohistiocytosis. Indian pediatrics, 51, 651-653.
- Khan, S. A., Bora, T., Laskar, B., Khan, A. M., & Dutta, P. (2017). Scrub typhus leading to acute encephalitis syndrome, Assam, India. Emerging Infectious Diseases, 23(1), 148.
- Bates, I., & Bain, B. J. (2012). Approach to the diagnosis and classification of blood diseases. Dacie and Lewis Practical Haematology, 549.
- Naseem, S., Varma, N., Das, R., Ahluwalia, J., Sachdeva, M. U. S., & Marwaha, R. K. (2011). Pediatric patients with bicytopenia/pancytopenia: review of etiologies and clinico-hematological profile at a tertiary center. İndian Journal of pathology and microbiology, 54(1), 75.
- Rehman Hu et al. The etiological pattern of pancytopenia in children under 15 years. Pak Armed Forces Med J 2003;53:183-7.
- Tilak, V., & Jain, R. (1999). Pancytopenia--a clinico-hematologic analysis of 77 cases. Indian journal of pathology & microbiology, 42(4), 399-404.
- Iqbal W, et al.Aetiological breakup of 208 cases pancytopenia. J Rawal Med Coll. 2001;5:7-9.
- Varghese, G. M., Abraham, O. C., Mathai, D., Thomas, K., Aaron, R., Kavitha, M. L., & Mathai, E. (2006). Scrub typhus among hospitalised patients with febrile illness in South India: magnitude and clinical predictors. Journal of Infection, 52(1), 56-60.
- Chrispal, A., Boorugu, H., Gopinath, K. G., Chandy, S., Prakash, J. A. J., Thomas, E. M., ... & Thomas, K. (2010). Acute undifferentiated febrile illness in adult hospitalized patients: the disease spectrum and diagnostic predictors–an experience from a tertiary care hospital in South India. Tropical doctor, 40(4), 230-234.
- Chowdhury, P., Khan, S. A., Dutta, P., Topno, R., & Mahanta, J. (2014). Characterization of West Nile virus (WNV) isolates from Assam, India: insights into the circulating WNV in northeastern India. Comparative Immunology, Microbiology and Infectious Diseases, 37(1), 39-47.
- Khan, S. A., Dutta, P., Borah, J., Chowdhury, P., Topno, R., Baishya, M., & Mahanta, J. (2012). Leptospirosis presenting as acute encephalitis syndrome (AES) in Assam, India. Asian Pacific Journal of Tropical Disease, 2(2), 151-153.
- Sharma, N., Biswal, M., Kumar, A., Zaman, K., Jain, S., & Bhalla, A. (2016). Scrub typhus in a tertiary care hospital in North India. The American Journal of Tropical Medicine and Hygiene, 95(2), 447.
- Bhat, N. K., Dhar, M., Mittal, G., Shirazi, N., Rawat, A., Kalra, B. P., ... & Ahmad, S. (2014). Scrub typhus in children at a tertiary hospital in north India: clinical profile and complications. Iranian journal of pediatrics, 24(4), 387.
- Yoo, J. R., Heo, S. T., Koh, Y. S., Kim, S., & Kim, S. (2014). Unusual genotypic distribution of Orientia tsutsugamushi strains causing human infections on Jeju Island. The American Journal of Tropical Medicine and Hygiene, 90(3), 507.
- Nadjm, B., Thuy, P. T., Trang, V. D., Dang Ha, L., Kinh, N. V., & Wertheim, H. F. (2014). Scrub typhus in the northern provinces of Vietnam: an observational study of admissions to a national referral hospital. Transactions of the Royal Society of Tropical Medicine and Hygiene, 108(11), 739-740.
- Silpapojakul, K., Varachit, B., & Silpapojakul, K. (2004). Paediatric scrub typhus in Thailand: a study of 73 confirmed cases. Transactions of the royal society of tropical medicine and hygiene, 98(6), 354-359.
- Niazi M, Raziq F. The Incidence of underlying pathology in pancytopenia: an experience of 89 cases. J Postgrad Med Inst 2004;18:76-9.
- Khan, F. S., & Hasan, R. F. (2012). Bone marrow examination of pancytopenic children. JPMA. The Journal of the Pakistan Medical Association, 62(7), 660-663.
- Ejaz, M. S., Latif, N., Ahmed, I. R., & Inkisar Ali, S. M. (2011). Etiological profile of pancytopenia in children: A hospital based study. Pakistan Journal of Medical Sciences, 27(2).
- Rao, K. S. (2011). Pancytopenia: a clinico hematological study. Journal of laboratory physicians, 3(01), 015-020.
- Pine, M., & Walter, A. W. (2010). Pancytopenia in hospitalized children: a five-year review. Journal of pediatric hematology/oncology, 32(5), e192-e194.
- Pine M. A retrospective review of the etiologies of pancytopenia in hospitalized children without cancer.
- Tareen, S. M., Tariq, M. M., Bajwa, M. A., Awan, M. A., Ahmad, Z., & Javed, Y. (2012). Study of pancytopenia in Balochistan, Pakistan. Gomal Journal of Medical Sciences, 10(2).
- Gupta, V., Tripathi, S., Tilak, V., & Bhatia, B. D. (2008). A study of clinico-haematological profiles of pancytopenia in children. Tropical doctor, 38(4), 241-243.
- Bhatnagar, S. K., Chandra, J., Narayan, S., Sharma, S., Singh, V., & Dutta, A. K. (2005). Pancytopenia in children: etiological profile. Journal of tropical pediatrics, 51(4), 236-239.


